Sonography-Assisted Venous Access: Details of Technique, Pearls, Pitfalls
Anthony J. Dean, M.D. Assistant Professor of Emergency Medicine University of Pennsylvania
Ultrasound technical and knobology issues 1. Depth 2. Frequency 3. Focus 4. Gain 5. Angle of insonation Ultrasound beams are reflected back towards the transducer with maximum efficiency if the reflecting surface is at right angles to the beam. This is especially true of highly reflective surfaces (“specular reflectors”) such as a needle or a vessel wall. Therefore, to get the sharp images in sono-guided venous access, it’s necessary to rock the probe continually to optimize visualization of these structures, especially since there is usually at least a 30 degree angle between the needle and the vessel (i.e. they cannot both be imaged simultaneously with a 90 degree angle of insonation). 6. Important artifacts a. Shadowing b. Reverberation c. Gain (“Black is Black”)
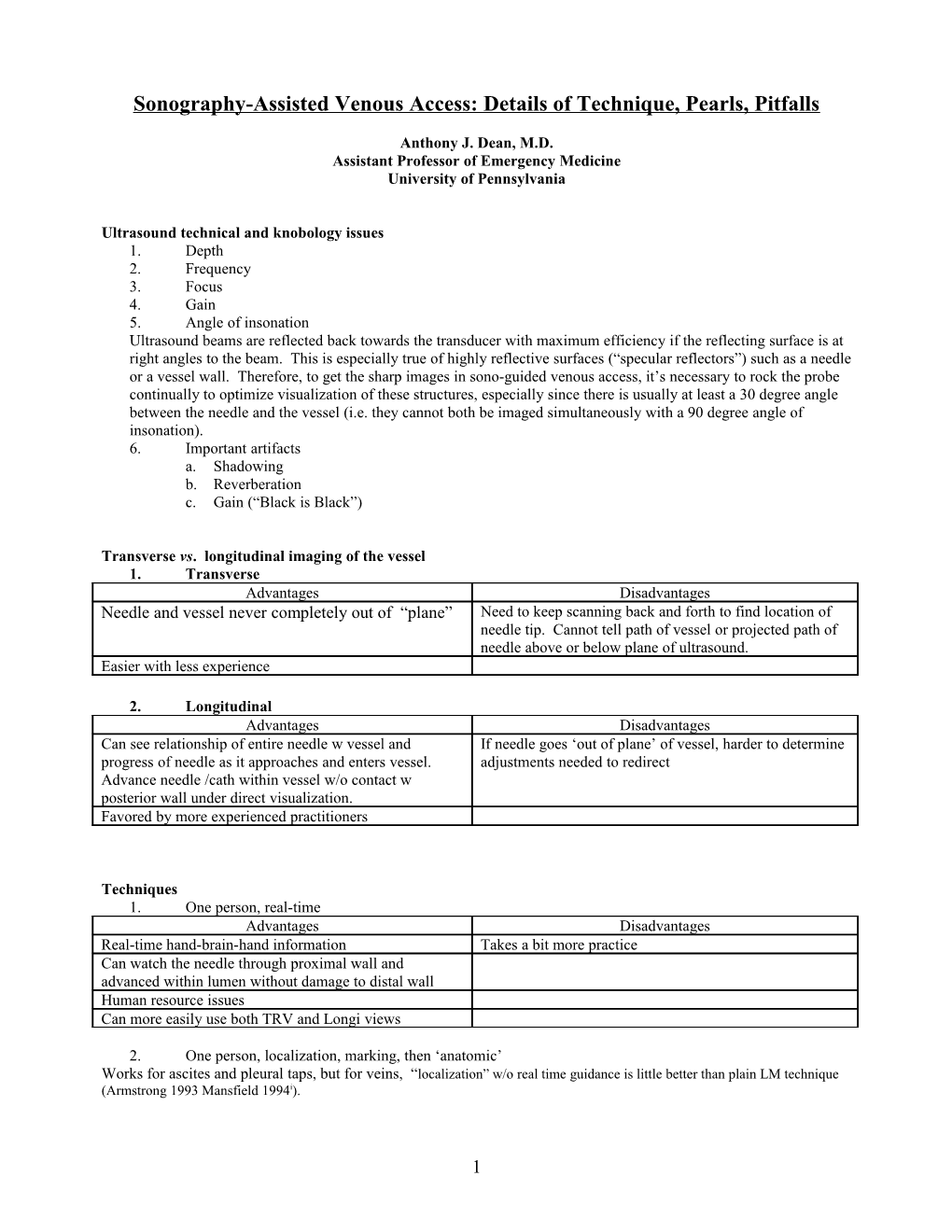
Transverse vs. longitudinal imaging of the vessel 1. Transverse Advantages Disadvantages Needle and vessel never completely out of “plane” Need to keep scanning back and forth to find location of needle tip. Cannot tell path of vessel or projected path of needle above or below plane of ultrasound. Easier with less experience
2. Longitudinal Advantages Disadvantages Can see relationship of entire needle w vessel and If needle goes ‘out of plane’ of vessel, harder to determine progress of needle as it approaches and enters vessel. adjustments needed to redirect Advance needle /cath within vessel w/o contact w posterior wall under direct visualization. Favored by more experienced practitioners
Techniques 1. One person, real-time Advantages Disadvantages Real-time hand-brain-hand information Takes a bit more practice Can watch the needle through proximal wall and advanced within lumen without damage to distal wall Human resource issues Can more easily use both TRV and Longi views
2. One person, localization, marking, then ‘anatomic’ Works for ascites and pleural taps, but for veins, “localization” w/o real time guidance is little better than plain LM technique (Armstrong 1993 Mansfield 1994i).
1 3. One person using needle guides: practical impediments in the ED: stocking and cost issues. 4. Two person Personnel / resource issues. Difficult without a sono-savvy assistant.
By far the easiest technique to master is single operator. From this point on, this is the technique that is discussed and advocated.
While starting out, especially if a preceptor is available, an assistant may be helpful to organize the space, adjust lighting, take the probe once the vein is entered, etc.
Choice of vein and location 1. Peripheral a. In the very obese, will often be able to locate otherwise undetectable veins in usual locations: remember courses of cephalic and basilic veins in upper extremities. b. In patients with damaged veins (chemo, IVDA, etc) often find the deep brachial intact: bicipital groove above antecubital fossa. Watch out for the nerve (easily identified by US).
2. Central a. IJ is by far the most studied and easiest. If this is absent or unavailable, experienced operators find the supraclavicular approach to the IJ-subclavian confluence preferable to the subclavicular approach to the SC. b. Lower IJ is more tethered, therefore more desirable access location, but closer to thorax, therefore often avoided (Denys 1993).
Issues of technique … prepare, prepare, prepare!
90% preparation + 10% perspiration << 10% preparation + 90% perspiration!
1. Ergonomics. a. Have the screen facing you at the patient’s shoulder level. Make sure you have the probe oriented so that the transverse section demonstrated on the screen is spatially in the same orientation as the patient’s anatomy (i.e. the left side of screen will refer to patient’s right when doing peripheral, but patient’s left doing IJ).
b. Be comfortable: this has a major impact on your chance of success! i. For IJ, the patient needs to be in Trendelenburg. If they are on a civil war era gurney without this adjustment, change gurneys unless precluded by extreme exigency (i.e. need STAT access). Would you want a central line started on your dehydrated family member subjecting them to increased risk of multiple sticks, venous trauma, and complications, just because their doctor couldn’t be bothered to put them on the right stretcher? ii. Adjust the height of the gurney [ditto (i) re gurney choice]. iii. For peripheral vein cannulation, find a stool with wheels. This allows for maximal mobility with stability and comfort.
c. Reconnoiter prior to draping and prepping. i. Is the vein present and compressible through it’s entire length? ii. Are there valves present? iii. Does it take sudden turns? iv. Are you sure you’re not looking at an artery in a hypotensive patient (also compressible: use color flow if in doubt). v. Especially important for peripheral access: you need to know where the vein runs in someone’s arm to position yourself, to position the arm, and to position the machine. vi. IJ has aberrant anatomy in 8.5% of cases and has very mobile anatomy w head motion (Denys 1993, Armstrong 1993). Aberrant IJ anatomy in 18% of kids (Alderson 1993).
2 d. Again: check compressibility: avoid the multiple sticks I inflicted on 1 patient culminating in “failed” central venous access 2/2 venous thrombosis. Check for scarring and narrowing if h/o previous CV catheter.
2. Use probe cover and semi-sterile technique even with peripheral lines. a. Probe cleanliness (NOT) b. Patient protection c. The value of the IV site and your time d. Can use sterile glove (unpowdered) in a pinch. e. Widely prep the skin as if for blood cultures.
3. Applying the sterile probe cover. Note: Non-sterile sonographic gel ALWAYS needs to be applied INSIDE the cover, and STERILE gel always needs to be placed between the cover and patient’s skin. a. If doing IJ with sterile technique i. Open sterile probe cover package before donning gloves. ii. Apply generous (NON-sterile gel) to probe iii. Place probe in inverted cover iv. Peel back cover over probe wire v. Lay sterile probe on sterile field of CV access drapes. vi. Caveats: probe easily slides from drapes … gets contaminated or hits the floor ($10,000!) vii. If assistant available, place probe inside cover after you are gloved. b. For peripheral sticks in patients who are venous access challenges, but who do not need a central line, do i –iii as above, apply sterile gel to the prepped skin, and proceed without touching the access site with anything except the needle, the gel, and the probe cover.
4. Analgesia: USE IT! This is a WIN-WIN PROPOSITION for you and the patient. With peripheral lines, as with central lines, squirt 1-3 cc of 1% lido (TB syringe often works) into the venous access site. This has several advantages: a. Patient comfort: many of these pt’s have already had many painful attempts, and the brachial vein is deep and painful to reach. b. Operator comfort: if your puncture site is in the wrong place, or your approach to the vein is off-line, spare yourself the pressure of an anxious and irritated patient! They don’t need to feel this, and you’ll be a hero when you “got the line in one shot … and I didn’t feel a thing!” c. Patient cooperation … patient stays still
5. Needle and catheter length a. Especially with brachial vein in obese patients, the standard 1.25” IV catheter is too short: the first time they shake their arm or bend it, the tip of the catheter is out of the lumen, in the subQ tissues. b. Use at least 1.75 inch catheters c. Consider use of 15cm catheters (pending Service Center supply) d. If necessary, use A-line kits or long caths in central venous access kits w Seldinger technique.
6. Artery vs. vein vs. nerve a. In the upper extremity and neck all 3 are present. i. Artery: pulsatile, usually not collapsible [careful w/ hypotension!], color flow + if available ii. Veins usually not seen w/o tourniquet or Trendelenburg. Thinner walled, collapsible, larger than arteries. iii. Nerves: can see stippled fascicular appearance when angle of insonation right. Non compressible. After application of tourniquet, veins do not show color flow. b. Very light touch not to collapse veins. c. In hypotensive pts, arteries may become collapsible w probe pressure.
7. Probe manipulation a. You will hold the probe in your non-dominant hand (the one normally used to stabilize the skin and-or palpate the vein). b. Hypothenar surface of hand against pt skin to stabilize probe and avoid slippage, maintain correct pressure.
3 8. Angle of needle advance a. May need to be steeper than for subcutaneous vessels: 30 degrees often optimal. This is both because the vessels are often deeper, and one doesn’t want several inches of subcutaneous tunnel (and can’t afford it with normal length catheters), and because a steep angle is needed to pierce the venous wall. b. Steep angle of advance makes puncture of distal wall more likely. Use real-time sonographic visualization of proximal vessel wall entry and advance of needle within lumen. c. Larger needles are more likely to cause penetration of posterior wall of vein. d. Interventional radiologists favor a 90 degree approach to the IJ. I have yet to meet a clinician who is practiced in starting lines without imaging, choose this technique.
9. Vein entry a. Watch the screen. Don’t bother to look for flash-back unless you’re really unsure whether you’re in the vein … this is a sono-guided procedure … you’re probably in a darkened room anyway. b. Once you have entered the vein, the job is only half done! Continue to watch the needle as it is advanced far enough for the bevel and/or catheter to be completely through the vessel wall and inside the lumen. Lower inserting hand toward pt’s skin: this raises the tip of the needle to avoid catching the back wall of the vein. Advance needle another 1 cm in vein under direct sono visualization. c. Put the probe down in a place where it can’t fall on the floor (preferably in its holster on the machine). With your free 2nd hand advance the catheter as for traditional access technique. Secure line as per usual.
4 ULTRASOUND GUIDED VENOUS ACCESS: REVIEW OF THE LITERATURE
The AHRQ (Agency on Healthcare Research and Quality) in its 2001 report identified sono guided central venous access as #8 in a list of eleven “most highly rated in terms of strength of evidence supporting more widespread implementation”ii.
Topic Paper Design N US vs LM Other findings Internal jugular Koski EMJ Crit Care Prospective randomized convenience 56 Avg sticks: 1.2 vs 3.3 10% of previously accessed (IJ) Med 20/3, p424 – 6, A single anesthesiologist Cann’n time 35 vs 198s IJs are occluded 1992iii. IJ Troianos CA. Anaesth Prospective randomized 150 Success 100 v. 96% 2/3 failed attempts by LM Analg: 72: 823-6, 1991iv. 5-7.5 MHz 1st pass succ: 72 vs 54% successful w sono Anaesthesiologists in O.R. Avg Advances: 1.4 vs 2.8 Time: 61 v 117s Carotid punct: 1.3% vs 7.8% IJ Docktor B: Can Assoc Prospective case series. 150 Success 100% 20% of cannulations Rad J: 47 195-201, 1996 Experienced radiologists Avg sticks: 1.1 involve posterior wall Probe as close as possible to clavicle 89% 1st pass success puncture. 5-7.5 MHz 1.3% carotid puncture Avoid puncture site where IJ is anterior to artery (seen in 25% of cases). L sided Ijs more difficult (? Practice issue) IJ Denys BG: Circ 87: 1557 Prosp random 604, then Success: 100 v 88% All levels of experience. – 62, 1993)v 7.5 MHz prospective 1st pass 78 v 38% More experienced operators Needle guide. case series Time 10 v 45s slightly better stats. 29 cardiologists w/ experience of 1-288 in 626 Carotid stick 1.7 vs 8.3% “Modified technique of procedures. Hematoma 0.2 v 3.3% ‘sideways’ puncture to No PTX in 1230 cases avoid CCA”. IJ and SC Randolph AG: Crit Care Meta-analysis of 8 randomized controlled Cumulative Relative risk of failure w sono: 32% Meta-analysis Med 24: 2053-8, 1996vi. trials (RCT) N=533 RR complication 22%. RR multiple passes 60% IJ, SC and Fem Calvert N, et al UK NHS Meta-analysis of 14 RCTs investigating Cumulative RR of failure vs. LM: SC=IJ=0.14. “Very strong evidence that Meta-analysis Health Technology US-guided vs LM technique. (Meta- N=1021 FV=0.29 US-guided CVA is more Assessment 2003vii. Same analysis also of Doppler technique… these Time -70sec (only IJ vs. LM) effective [than LM Data published by Hind et excluded on current table). # attempts IJ -1.5. FV -2.7 technique]” al BMJ 2003viii. Complication rate IJ= 0.43; SC=0.1; FV=n/a Similar results in infants IJ, SC and Fem Rothscild JM, Chapter 21 Meta-anlysis of 5 studies using of IJ (3), RR Failure 71-100% Meta-analysis of AHRQ 2001 report SC(1) and FV (1) approaches (Meta- Red’n mean insertion attempts: 44-54% Error: Reference source analysis also of Doppler technique… these RR complications 83 – 100% not found. excluded on current table).
5 Topic Paper Design N US vs LM Other findings
IJ: effect of Geddes CC: Clin Nephr: Prospective. Residents, fellows. 107 No difference in success rate inexperienced 50/5 329-5, 1998. “Experienced”: > 25 IJ caths, procedures, operators + and “inexperience” < 25 IJ caths 7 operators - sono SC(85%); Fry WR. Arch Surg 134: Prospective case series. Complicated pts 52 Success 100% IJ(13%), 738-41, 1999. (coagulopathy, hypovolemia, unable to lay Complication: 1 PTX only Innominate flat, stenosis, etc) (2%) 5 – 7 MHz, no guide Surgeons Fem (75%), IJ Miller AH: Acad EM 9: Prosp random 71 Sticks: 1.6 vs 3.5 (p<0.0001) (13%), SC 800-5, 2002ix. EM residents w attends Time115 vs 512 s (p<0.0001) (13%) Many inexperienced. Fem vein in Hilty WM Annals EM Prosp random, subj controlled 20 Success: 90% vs 65% LM Femoral v cath in other CPR 29:331-7, 1997. Emergency Physicians 7.5 MHz Advances: 2.3 vs 5 CPR studies similar Tome: 121 v. 124 s (NS) (Jastremski 1984, Sessler 1987) Fem “pulse” w CPR is the vein (not femoral artery) Peripheral Sofocleous CT. AJR 170 Retrospective case series 355 All sono Keep angle between PICC 1613-6, 1998x 5-7.5 MHz Brachial 74%; Basilic 18%; Cephalic 8% transducer and needle 850- placement 70% of pts IVDA 99% success 950 Radiologists Avg sticks 1.2 Peripheral LaRue GD. J Intraven 431 retrospect LM, 326 prospect sono. All 757 Avg sticks 1.2 vs 1.7 Compression of ant wall Nursing 23/1 29 – 34, by one nurse anesthetist 9 MHz Avg advances 1.4 vs 2.4 causes penetration of post 2000xi. Success 99% in both wall in many cases. Success w/ larger caths w sono Peripheral IV Costantino TG et al: Ann PRCT 60 Success 97 vs. 33% Also greater pt satisfaction : in difficult- Emerg Med, 2005 xii 2- person technique. 20 operators. None > Time: 13 vs. 30 min 8.7 vs. 5.7 / 10 access patients 6 lines. 1.7 vs 3.7 punctures. 4 ‘experienced’ [>10 proced] and 16 ‘not experienced’ operators IJ Leung J et al: Ann Emerg PRCT in the ED 130 Success 94 vs 79% Med, 2006 xiii Sonosite TRV real-time vs. landmark Linear array 1st attempt success: 82 vs 71% 10-5 MHz Complications 5 vs. 17% No difference in time.
Notes For LM technique, typical overall success rates 90-95%; carotid stick rates 4-8%; 1st – 2nd pass rates 50 - 60%. (Daily 1970, Schwartz 1979, Golfarb 1982).
Cost: Modest savings $3249 per 1000 procedures anticipated by analysis in Hind article, although this analysis assumes cost of purchase of dedicated equipment for US guided.
6 i Mansfield PF. Hohn DC. Fornage BD. Gregurich MA. Ota DM. Complications and failures of subclavian-vein catheterization. New England Journal of Medicine. 331(26):1735-8, 1994. ii Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Evidence Report/Technology Assessment: Number 43. AHRQ Publication No. 01-E058, July 2001. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/clinic/ptsafety/ iii Koski EM. Suhonen M. Mattila MA. Ultrasound-facilitated central venous cannulation. Critical Care Medicine. 20(3):424-6, 1992 Mar. iv Troianos CA. Jobes DR. Ellison N. Ultrasound-guided cannulation of the internal jugular vein. A prospective, randomized study. Anesthesia & Analgesia. 72(6):823-6, 1991 Jun. v Denys BG. Uretsky BF. Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 87(5):1557-62, 1993. vi Randolph AG. Cook DJ. Gonzales CA. Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta- analysis of the literature. Critical Care Medicine. 24(12):2053-8, 1996. vii The National Health Service Health Technology Assessment 2003; vol 7(12), The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Queen's Printer and Controller of HMSO 2003. www.cinahl.com/cexpress/hta/summ/summ712.pdf viii Hind D. Calvert N. McWilliams R. Davidson A. Paisley S. Beverley C. Thomas S. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 327(7411):361, 2003 Aug 16. ix Miller AH. Roth BA. Mills TJ. Woody JR. Longmoor CE. Foster B. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Academic Emergency Medicine. 9(8):800-5, 2002. x Sofocleous CT. Schur I. Cooper SG. Quintas JC. Brody L. Shelin R. Sonographically guided placement of peripherally inserted central venous catheters: review of 355 procedures. AJR. American Journal of Roentgenology. 170(6):1613-6, 1998. xi LaRue GD. Efficacy of ultrasonography in peripheral venous cannulation. Journal of Intravenous Nursing. 23(1):29-34, 2000. xii Costantino TG. Bruno EC. Handly N. Dean AJ. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. Journal of Emergency Medicine; 2005: 29(4):455-60. xiii Leung J. Duffy M. Finckh A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Annals of Emergency Medicine, 2006; 48(5):540-7.