Plasma levels of TIMP-1 are higher in 34-year-old individuals with severe α1-antitrypsin deficiency
Sabina Janciauskiene, Devipriya Subramaniyam, Eeva Piitulainen, Thomas Köhnlein, Tomas Sveger
Supplementary data
Between 1972 and 1974, neonatal screening was undertaken in Sweden to identify AATD in new born infants.[1] One important aim of this screening was to study the natural history and
(patho)physiology of lung and liver disease in AATD. In this cohort lung function tests have been performed every fourth year from the subject`s 16th year and these showed normal mean lung function parameters in subjects both with severe ZZ and intermediate SZ AAT deficiency from the age of 16 up to 30 years of age.[2-3] This study was conducted in accordance with the Helsinki Declaration and approved by the Regional Ethical Review
Board of Lund University, Sweden.
At the 34-year check-up, the AATD individuals, followed prospectively were asked to contribute a blood sample for research. A sub-group of 50 ZZ and 22 SZ and 84 age-matched control individuals agreed to participate.[4] Blood was collected in tubes containing sodium heparin (B-D Vaccutainer system, USA) and was centrifuged within 30 min of collection at
2000 x g at 4°C for 10 min. Plasma was separated and stored within 24 hours at -20°C until assayed.
The collection of lung function data for 34 years check-up is in progress and has not yet been completed. Thus, we will only be able to present combined data from lung function and laboratory tests in the next clinical report from this prospective study. Notably, our study sub- group includes few cigarette smokers (3 in ZZ group and 13 in controls), therefore we do not consider the smoking habit at the present research data analysis. Our previous research reports focused on plasma markers of the serine protease/protease inhibitor balance.[5-7] These earlier findings laid the basis for the hypothesis that compensatory up-regulation of specific serine protease inhibitors in AATD subjects during childhood, adolescence and young adulthood may favourably affect the overall protease/protease-inhibitor balance and protect the lung tissue against proteolytic leukocyte enzymes. There is now increasing evidence that an excessive activity of various proteolytic enzymes in the lung milieu, including members of the metalloproteinase families, may damage the elastin network of the lung.
Metalloproteinases (MMPs) and their inhibitors, the tissue inhibitors of metalloproteinase
(TIMPs), have been shown to participate in extracellular matrix remodeling in the lung and play an important role in the pathogenesis of COPD.[8] As a matter of fact, there is evidence that gene variants of TIMPs influence susceptibility to COPD.[9] Tissue inhibitor of metalloproteinases-1 (TIMP-1) is one of four known TIMPs, and it is the physiological inhibitor of matrix metalloproteinase-9 (MMP-9, gelatinase B).[10, 11] TIMP-1 also acts as a growth stimulator and inhibits cell apoptosis.[12, 13] Previous studies have shown that TIMP-
1 is spontaneously secreted by human granulocytes in both healthy subjects and patients with asthma and COPD.[14] As TIMP-1 is an anti-elastolytic molecule[15], it has been hypothesized that the reduced release of TIMP-1 may contribute to the development of pulmonary emphysema. TIMP-1 has been suggested as an early predictive biomarker of airway obstruction and exacerbation in COPD.[16]
Therefore, in this study we wanted to measure the plasma concentration of TIMP-1 and correlate it with levels of AAT and CRP in asymptomatic ZZ and SZ AATD young adults at about the age of 34, and age-matched controls. The concentrations of plasma CRP and AAT were analyzed by nephelometry at the Department of Clinical Chemistry in Malmo (Malmo University Hospital, Sweden). CRP was analysed using a high sensitivity method with a minimum detection level of 0.2 g/l. Plasma levels of TIMP-1 were measured using a commercially available sandwich enzyme linked immunosorbent assay (ELISA) kit (Catalog
DY970, R&D systems, UK) according to the manufacturer’s instructions. The minimum detectable dose of TIMP-1 was less than 0.08 ng/ml with good intra-assay precision (mean concentration was 0.48 ng/ml with S.D. – 0.02 and %CV – 4.2 when a sample of known concentration was tested 20 times on one plate) and inter-assay precision (mean concentration was 0.51 ng/ml with S.D. – 0.02 and %CV – 3.9 when a sample of known concentration was tested in 40 separate assays). The average recovery and linearity from spiked human plasma was 99% and 100-104%, respectively. In order to avoid bias in the analysis of plasma TIMP-1 levels all samples were coded prior to analysis and analysed blindly by the laboratory assistant.
The data were analysed using the SPSS software (version 17.0.1, SPSS Inc, USA). All variables were analysed for normal distribution by the Kolmogorov-Smirnov test. Because the variables were not normally distributed we therefore used the Kruskal-Wallis and the Mann
Whitney U-test. The estimation of the bivariant correlation between the variables was performed by computing the Spearman`s correlation coefficient. The level of confidence at which the results were judged significant was P < 0.05.
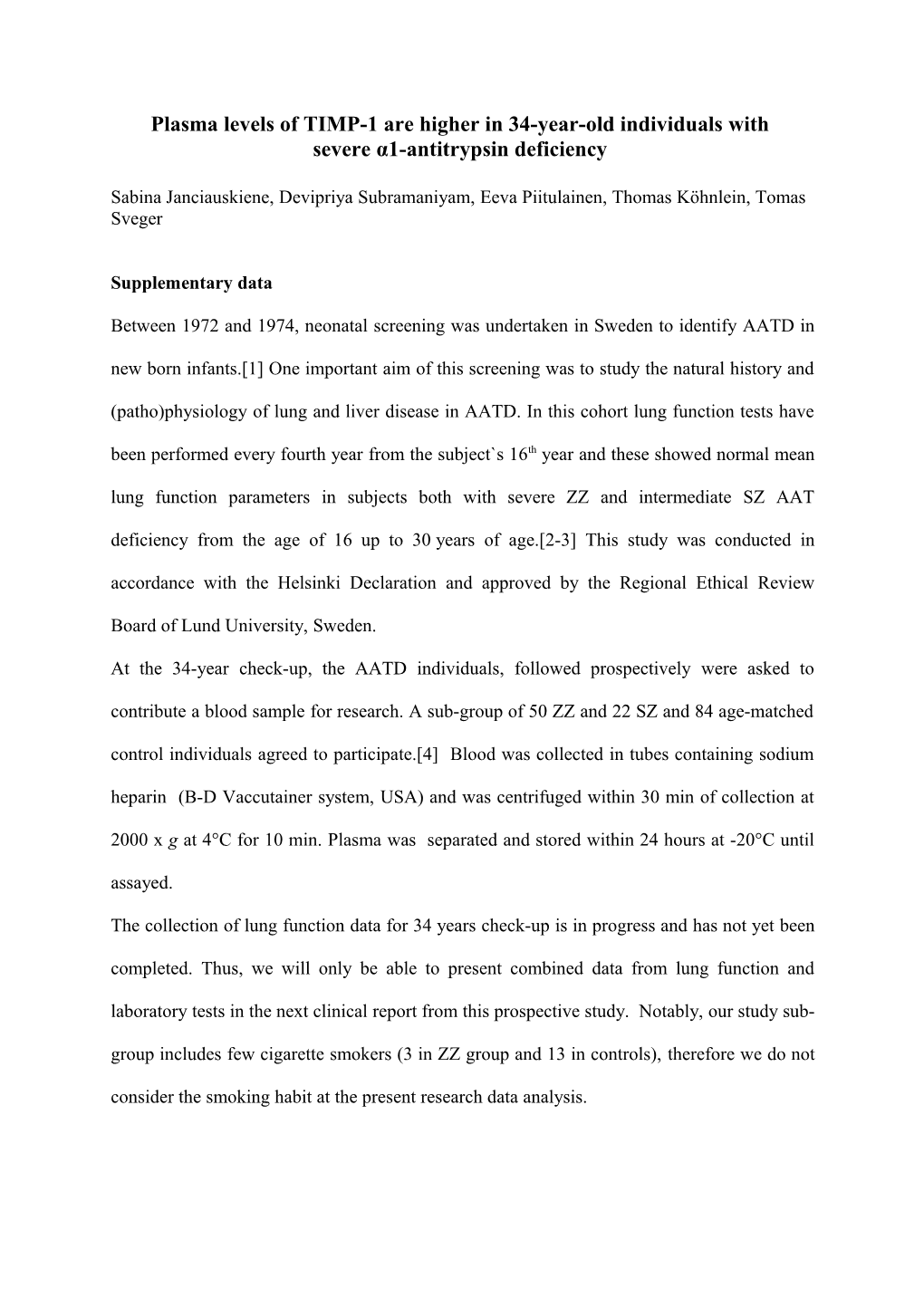
Cigarette smoke has been reported to increase the mRNA levels of TIMP-1 in the lungs in vivo.[17] In our cohort, no significant relationship was found between plasma TIMP-1 levels and smoking habit. The question as to whether circulating levels of TIMP-1 in young adults with AATD may be related to lung function test warrants further investigation. Figure 1
300
) 250 l r =- 0.44, p<0.001 m / g n (
200
n Plot 1 o i t a r t 150 n e c n o c
100 1 - P M I
T 50
0
0,0 0,5 1,0 1,5 2,0 2,5 3,0
AAT concentration (mg/ml)
Figure 1 legend
Plasma levels of TIMP-1 negatively correlate with AAT levels.
Plasma TIMP-1 levels were plotted against plasma levels of AAT for all the individuals included in the study. Higher plasma levels of TIMP-1 correlated with lower levels of AAT
(r=-0.459, p<0.001) as performed by computing the Spearman`s correlation coefficient. References
1. Laurell CB, Sveger T. Mass screening of newborn Swedish infants for alpha
antitrypsin deficiency. Am J Hum Genet. 1975;27(2):213-217.
2. Bernspang E, Sveger T, Piitulainen E. Respiratory symptoms and lung function in 30-
year-old individuals with alpha-1-antitrypsin deficiency. Respir Med.
2007;101(9):1971-1976.
3. Piitulainen E, Sveger T. Respiratory symptoms and lung function in young adults with
severe alpha(1)-antitrypsin deficiency (PiZZ). Thorax. 2002;57(8):705-708.
4. Bernspang E, Wollmer P, Sveger T, Piitulainen E. Lung function in 30-year-old alpha-
1-antitrypsin-deficient individuals. Respir Med. 2009;103(6):861-865.
5. Hollander C, Westin U, Wallmark A, Piitulainen E, Sveger T, Janciauskiene SM.
Plasma levels of alpha1-antichymotrypsin and secretory leukocyte proteinase inhibitor
in healthy and chronic obstructive pulmonary disease (COPD) subjects with and
without severe alpha1-antitrypsin deficiency. BMC Pulm Med. 2007;7:1.
6. Piitulainen E, Carlson J, Ohlsson K, Sveger T: Alpha1-antitrypsin deficiency in 26-
year-old subjects: lung, liver, and protease/protease inhibitor studies. Chest.
2005;128(4):2076-2081.
7. Sveger T, Ohlsson K, Piitulainen E. Adolescents with alpha1-antitrypsin deficiency
have high alpha2-macroglobulin and low neutrophil lipocalin and elastase levels in
plasma. Pediatr Res. 1998;44(6):939-941.
8. Hogg JC, Senior RM. Chronic obstructive pulmonary disease - part 2: pathology and
biochemistry of emphysema. Thorax. 2002;57(9):830-834.
9. Hirano K, Sakamoto T, Uchida Y, Morishima Y, Masuyama K, Ishii Y, Nomura A,
Ohtsuka M, Sekizawa K. Tissue inhibitor of metalloproteinases-2 gene polymorphisms in chronic obstructive pulmonary disease. Eur Respir J.
2001;18(5):748-752.
10. Brew K, Dinakarpandian D, Nagase H. Tissue inhibitors of metalloproteinases:
evolution, structure and function. Biochim Biophys Acta. 2000;1477(1-2):267-283.
11. Olson MW, Gervasi DC, Mobashery S, Fridman R. Kinetic analysis of the binding of
human matrix metalloproteinase-2 and -9 to tissue inhibitor of metalloproteinase
(TIMP)-1 and TIMP-2. J Biol Chem. 1997;272(47):29975-29983.
12. Triebel S, Blaser J, Gote T, Pelz G, Schuren E, Schmitt M, Tschesche H. Evidence for
the tissue inhibitor of metalloproteinases-1 (TIMP-1) in human polymorphonuclear
leukocytes. Eur J Biochem. 1995;231(3):714-719.
13. Zaoui P, Barro C, Morel F. Differential expression and secretion of gelatinases and
tissue inhibitor of metalloproteinase-1 during neutrophil adhesion. Biochim Biophys
Acta. 1996;1290(1):101-112.
14. Cataldo D, Munaut C, Noel A, Frankenne F, Bartsch P, Foidart JM, Louis R. Matrix
metalloproteinases and TIMP-1 production by peripheral blood granulocytes from
COPD patients and asthmatics. Allergy. 2001;56(2):145-151.
15. Russell RE, Culpitt SV, DeMatos C, Donnelly L, Smith M, Wiggins J, Barnes PJ.
Release and activity of matrix metalloproteinase-9 and tissue inhibitor of
metalloproteinase-1 by alveolar macrophages from patients with chronic obstructive
pulmonary disease. Am J Respir Cell Mol Biol. 2002;26(5):602-609.
16. Higashimoto Y, Yamagata Y, Iwata T, Okada M, Ishiguchi T, Sato H, Masuda M, Itoh
H. Increased serum concentrations of tissue inhibitor of metalloproteinase-1 in COPD
patients. Eur Respir J. 2005;25(5):885-890. 17. Clark IM, Swingler TE, Sampieri CL, Edwards DR. The regulation of matrix
metalloproteinases and their inhibitors. Int J Biochem Cell Biol. 2008;40(6-7):1362-
1378.