APPENDIX
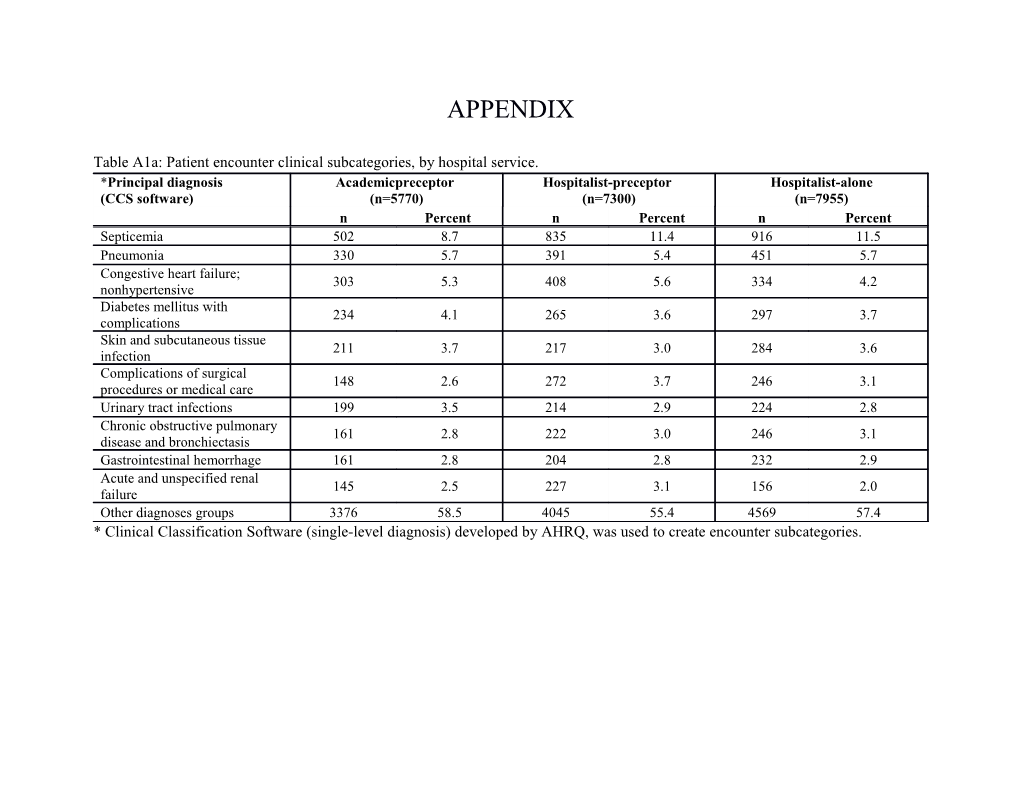
Table A1a: Patient encounter clinical subcategories, by hospital service. *Principal diagnosis Academicpreceptor Hospitalist-preceptor Hospitalist-alone (CCS software) (n=5770) (n=7300) (n=7955) n Percent n Percent n Percent Septicemia 502 8.7 835 11.4 916 11.5 Pneumonia 330 5.7 391 5.4 451 5.7 Congestive heart failure; 303 5.3 408 5.6 334 4.2 nonhypertensive Diabetes mellitus with 234 4.1 265 3.6 297 3.7 complications Skin and subcutaneous tissue 211 3.7 217 3.0 284 3.6 infection Complications of surgical 148 2.6 272 3.7 246 3.1 procedures or medical care Urinary tract infections 199 3.5 214 2.9 224 2.8 Chronic obstructive pulmonary 161 2.8 222 3.0 246 3.1 disease and bronchiectasis Gastrointestinal hemorrhage 161 2.8 204 2.8 232 2.9 Acute and unspecified renal 145 2.5 227 3.1 156 2.0 failure Other diagnoses groups 3376 58.5 4045 55.4 4569 57.4 * Clinical Classification Software (single-level diagnosis) developed by AHRQ, was used to create encounter subcategories. Table A1b: Comorbid conditions for all patient encounter, by hospital service. Academic-preceptor Hospitalist-preceptor Hospitalist *Comorbidities (n=5770) (n=7300) (n=7955) n Percent n Percent n Percent Hypertension 3354 58.1 4621 63.3 4540 57.1 Fluid and electrolyte disorder 2349 40.7 2959 40.5 3060 38.5 Deficiency Anemias 2164 37.5 2863 39.2 2794 35.1 Diabetes w/o Chronic Complications 1543 26.7 2067 28.3 2079 26.1 Chronic Pulmonary Disease 1473 25.5 1996 27.3 2273 28.6 Congestive Heart Failure 1466 25.4 2133 29.2 1974 24.8 Renal Failure 1244 21.6 1905 26.1 1720 21.6 Depression 1056 18.3 1461 20.0 1429 18.0 Alcohol Abuse 978 17.0 842 11.5 977 12.3 Liver Disease 894 15.5 1045 14.3 940 11.8 Drug Abuse 836 14.5 785 10.8 884 11.1 Coagulation Deficiency 680 11.8 735 10.1 685 8.6 Other Neurological Disorders 650 11.3 925 12.7 920 11.6 Diabetes with Chronic Complications 637 11.0 973 13.3 894 11.2 Hypothyroidism 611 10.6 974 13.3 869 10.9 Psychoses 595 10.3 721 9.9 833 10.5 Obesity 455 7.9 573 7.9 677 8.5 Weight loss 394 6.8 556 7.6 723 9.1 Rheumatoid Arthritis/Collagen Vascular 387 6.7 603 8.3 474 6.0 Diseases Valvular Disease 364 6.3 516 7.1 441 5.5 Pulmonary Circulation Disorders 358 6.2 482 6.6 448 5.6 Paralysis 302 5.2 467 6.4 434 5.5 Peripheral Vascular Disease 294 5.1 413 5.7 414 5.2 Metastatic Cancer 242 4.2 294 4.0 239 3.0 Solid Tumor without Metastasis 205 3.6 311 4.3 318 4.0 Academic-preceptor Hospitalist-preceptor Hospitalist *Comorbidities (n=5770) (n=7300) (n=7955) n Percent n Percent n Percent Blood loss anemia 129 2.2 166 2.3 148 1.9 HIV and AIDS 100 1.7 150 2.1 76 1.0 Lymphoma 61 1.1 72 1.0 50 0.6 Chronic Peptic Ulcer Disease 5 0.1 7 0.1 6 0.1 *Comorbid conditions were determined using the Elixhauser Method.
Table A1c: Readmission events within 14, 30 and 60 days, by hospital service.
Academic-preceptor Hospitalist-preceptor Hospitalist Readmission (n=5770) (n=7300) (n=7955) n Percent n Percent n Percent 14-day 504 8.7 670 9.2 604 7.6 30-day 867 15.0 1094 15.0 1013 12.7 60-day 1313 22.8 1746 23.9 1640 20.6 Table A2: Unadjusted patient outcomes reported on the absolute scale- 30-day readmission rate, LOS, index hospitalization cost, cumulative cost (index encounter plus readmissions within 30 days of discharge). Outcome Academic-preceptor Hospitalist-preceptor Hospitalist-alone 30-day Readmission Rate 15.6 15.7 11.7 95% CI (14.3, 17.0) (14.5, 17.0) (10.8, 12.7) Length of Stay * Days 5.52 5.52 6.15 95% CI (5.42, 5.61) (5.43, 5.61) (6.05, 6.25) Cost of Index Encounter* US $ 15211 15245 16728 95% CI (14961, 15466) (14909, 15588) (16338, 17128) Cumulative Hospital Cost within 30 days* US $ 18883 17932 20777 95% CI (18445, 19333) (16633, 19331) (19277, 22394) Estimates from generalized estimating equation are reported on the original scale and adjusted for clustering, unadjusted for covariates. * The variable was log-transformed; ratios reported are the antilog of the parameter estimate, which can be interpreted in the original scale. We included a smearing estimator in log-linear models to account for retransformation bias.
Table A3: Unadjusted patient outcomes 30-day readmission, length of stay, difference in cost of index hospitalization, and difference in cumulative cost (index encounter plus readmissions within 30 days of discharge). Academic-preceptor Hospitalist-preceptor Academic-preceptor Outcome vs. Hospitalist-alone vs. Hospitalist-alone vs. Hospitalist-preceptor 30-day Readmission Odds Ratio 1.20 1.18 1.01 95% CI (1.08, 1.32) (1.08, 1.30) (0.92, 1.11) p value <0.001 <0.001 0.83 Length of Stay* Difference in Days -0.40 -0.38 -0.02 95% CI (-0.50, -0.30) (-0.48, -0.28) (-0.13, 0.09) p value <0.001 <0.001 0.7280 Index Hospitalization Cost* Cost Difference (US $) -966 -903 -66 95% CI (-1298, -625) (-1309, -486) (-382, 991) p value <0.001 <0.001 0.6838 Cumulative Hospital Cost within 30 days* Cost Difference (US $) -976 -1490 559 95% CI (-1741, -176) (-2765, -115) (-320, 1477) p value 0.0172 0.0342 0.2169 Estimates from generalized estimating equation are reported on the original scale and adjusted for clustering, unadjusted for covariates. * The variable was log-transformed; ratios reported are the antilog of the parameter estimate, which can be interpreted in the original scale. We included a smearing estimator in log-linear models to account for retransformation bias.