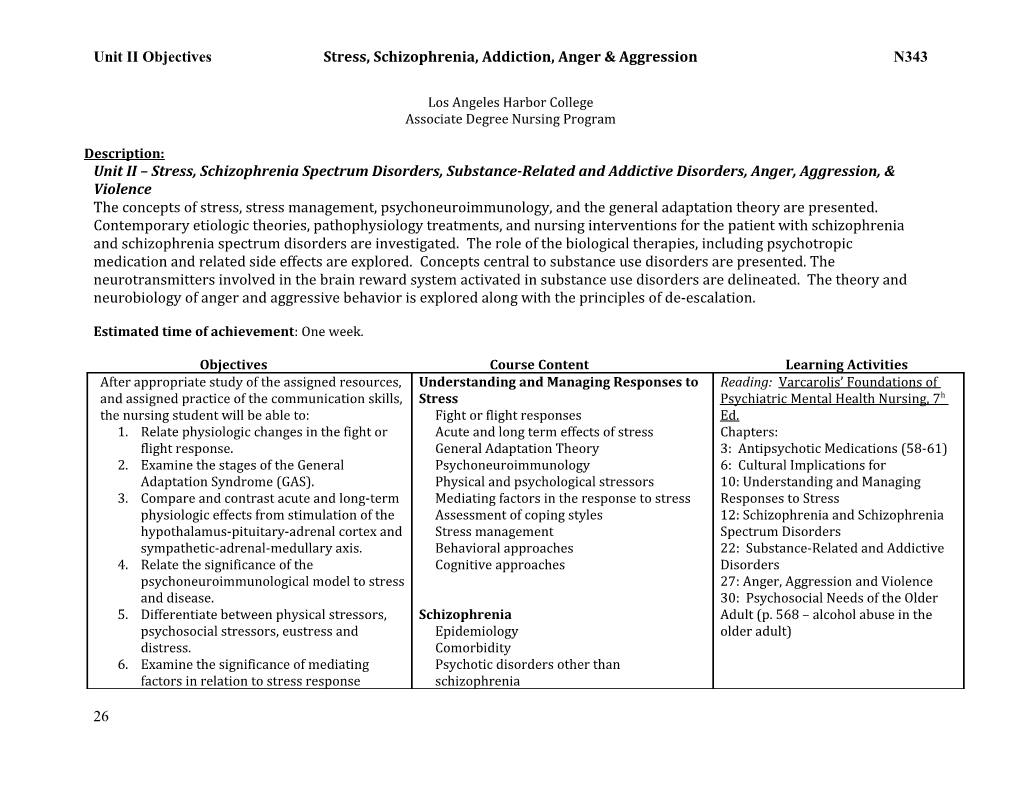
Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
Los Angeles Harbor College Associate Degree Nursing Program
Description: Unit II – Stress, Schizophrenia Spectrum Disorders, Substance-Related and Addictive Disorders, Anger, Aggression, & Violence The concepts of stress, stress management, psychoneuroimmunology, and the general adaptation theory are presented. Contemporary etiologic theories, pathophysiology treatments, and nursing interventions for the patient with schizophrenia and schizophrenia spectrum disorders are investigated. The role of the biological therapies, including psychotropic medication and related side effects are explored. Concepts central to substance use disorders are presented. The neurotransmitters involved in the brain reward system activated in substance use disorders are delineated. The theory and neurobiology of anger and aggressive behavior is explored along with the principles of de-escalation.
Estimated time of achievement: One week.
Objectives Course Content Learning Activities After appropriate study of the assigned resources, Understanding and Managing Responses to Reading: Varcarolis’ Foundations of and assigned practice of the communication skills, Stress Psychiatric Mental Health Nursing, 7 h the nursing student will be able to: Fight or flight responses Ed. 1. Relate physiologic changes in the fight or Acute and long term effects of stress Chapters: flight response. General Adaptation Theory 3: Antipsychotic Medications (58-61) 2. Examine the stages of the General Psychoneuroimmunology 6: Cultural Implications for Adaptation Syndrome (GAS). Physical and psychological stressors 10: Understanding and Managing 3. Compare and contrast acute and long-term Mediating factors in the response to stress Responses to Stress physiologic effects from stimulation of the Assessment of coping styles 12: Schizophrenia and Schizophrenia hypothalamus-pituitary-adrenal cortex and Stress management Spectrum Disorders sympathetic-adrenal-medullary axis. Behavioral approaches 22: Substance-Related and Addictive 4. Relate the significance of the Cognitive approaches Disorders psychoneuroimmunological model to stress 27: Anger, Aggression and Violence and disease. 30: Psychosocial Needs of the Older 5. Differentiate between physical stressors, Schizophrenia Adult (p. 568 – alcohol abuse in the psychosocial stressors, eustress and Epidemiology older adult) distress. Comorbidity 6. Examine the significance of mediating Psychotic disorders other than factors in relation to stress response schizophrenia
26 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
(individual factors, social factors, culture, Etiology/Theory Discussion/Lecture spirituality, and prayerfulness. DSM V criteria 7. Appraise the four coping styles individuals Phases of the disease Clinical Experiences develop to manage stress. Prepsychotic symptoms Prep/Pathophysiology Sheets 8. Measure personal stress level using the Positive symptoms Daily Charting Life-Changing Events Questionnaire and Negative symptoms Mental Status Assessment the Perceived Stress Scale. Alterations in speech Process Recordings 9. Evaluate the role of stress in influencing Alterations in perception History and Assessments mental and physical health. Cognitive symptoms Nursing Care Plans 10. Personally practice and teach stress Affective symptoms Client interaction management techniques to patients Specific nursing interventions including behavioral approaches hallucinations, delusions and associative Simulated Experience (meditation, guided imagery, breathing looseness exercises, muscle relaxation, and Self-assessment when working with patients Online Student Resources: biofeedback) and cognitive approaches who have schizophrenia http://evolve.elsevier.com/Varcarolis (journal keeping, priority restructuring, Potential nursing diagnoses Answer key to chapter review cognitive reframing, humor, assertiveness Outcome criteria based on phase of questions training). treatment Answer key to critical thinking 11. Prescribe other methods of stress Milieu therapy guidelines reduction (sleep, exercise, caffeine Communication guidelines Case Studies and nursing care plans cessation, music, pets, massage, etc.). Teamwork and Safety guidelines NCLEX review questions 12. Identify the schizophrenia spectrum Patient and family health teaching Pre and post tests disorders. Psychopharmacology/Adjunct Treatment 13. Examine the prevalence and comorbidities Typical Antipsychotics Kaplan Resources: of schizophrenia. Chlorpromazine (Thorazine) http://nursing.kaplan.com 14. Distinguish the neurobiologic, genetic, Fluphenazine (Prolixin) Focused psych review tests neuroanatomical, and non-genetic risk Fluphenazine decanoate (Prolixin) Psychiatric case studies factors related to schizophrenia. Haloperidol (Haldol) NCLEX text bank 15. Describe the symptoms, progression, Haloperidol decanoate (Haldol) nursing care and treatment needs for the Loxapine (Loxitane) Medcom Online Video Series: prepsychotic through maintenance phases Thioridazine (Mellaril) http://www.medcomrn.com/lahc of schizophrenia. Molindone (Moban) 16. Differentiate between positive, negative, Perphenazine (Trilafon) VIDM78866AT – Psychotropic cognitive and affective symptoms of Thiothixene (Navane) Medications: Antipsychotic Agents schizophrenia with regard to (a) their Trifluoperazine (generic only) response to traditional and atypical Atypical Antipsychotics
27 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
antipsychotic medications, (b) their effects Asenapine (Saphris) NLL Audio Visuals: on quality of life, and (c) their significance Clozapine (Clozaril) for the prognosis of the disease. Iloperidone (Finapt) DVD 73 Psychology of Addiction 17. Propose and prioritize nursing diagnoses Lurasidone (Lutada) DVD 76 Roots of Addiction: Drug & appropriate for a patient with Olanzapine (Zyprexa) Behavioral Compulsions schizophrenia. Paliperidone (Invega) 18. Identify outcomes for each diagnosis. Quetiapine (Seroquel) 19. Explore how to deal with common Risperidone (Risperdal/Risperdal reactions experienced by nurses working Consta) with schizophrenic patients. Ziprasidone (Geodon) 20. Relate the components of a therapeutic Third-Generation Antipsychotic milieu for patients with schizophrenia and Aripiprazole (Abilify) principles to integrate when the patient is Antidepressants in acute psychosis. Mood Stabilizing Agents 21. Identify and utilize appropriate Benzodiazepines communication techniques for patients Antipsychotic side effects and nursing who are hearing voices, having delusions, management experiencing paranoia, having associative Assessment and interventions for looseness, are catatonic, or disorganized. extrapyramidal side effects 22. Propose ways the patient can cope with Neuroleptic Malignant Syndrome voices and worrying thoughts. 23. Examine patient and family teaching Addictive Disorders principles for schizophrenia. Prevalence 24. Compare and contrast the properties Psychiatric and Medical Comorbidity typical, atypical and third generation Etiology/Theory antipsychotics in the following areas: (a) Codependence mechanism of action/ target Self-assessment neurotransmitters, (b) side effects, toxic Chemically impaired nurse effects, neurotransmitters involved in Signs of intoxication, overdose, treatment for adverse effects, (c) routes and usual overdose, and withdrawal for the following: dosages, (d) pros and cons of use for each Central nervous system depressants class. Barbiturates 25. Analyze the Abnormal Involuntary Benzodiazepines Movement scale and relate it to Chloral hydrate corresponding extrapyramidal symptoms Alcohol (ETOH) assessed. Central nervous system stimulants
28 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
26. Examine nursing measures for Cocaine, crack antipsychotic adverse effects (weight gain, Amphetamines (methamphetamine, anticholinergic effects/crisis, orthostatic dextroamphetamine) hypotension, sedation, extrapyramidal side Opiates effects, metabolic syndrome, Opium agranulocytosis, cholestatic jaundice, and Heroin neuroleptic malignant syndrome). Meperidine (Demerol) 27. Define addiction as a chronic brain disease. Morphine 28. Describe the neurobiologic process that Codeine occurs and neurotransmitters involved Methadone (Dolophine) with activation of the brain reward system. Hydromorphone (Dilaudid) 29. Examine the prevalence and comorbidities Fentanyl (Sublimaze) (psychiatric and medical) of addictive Cannabinoids disorders. Marijuana (cannabis sativa) 30. Distinguish the biologic, genetic, Hashish psychological, sociocultural findings Hallucinogens related to the etiology of addictive Lysergic acid diethylamide (LSD) disorders. Mescaline (peyote) 31. Differentiate the terms tolerance, Psilocybin withdrawal, synergistic effects and Dissociative Drugs antagonistic effects. Ketamine 32. Propose risks associated with synergistic Phencyclidine piperidine (PCP) and antagonistic effects. Salvia divinorum 33. Examine the phenomenon of codependency Dextromethorphan (DXM) and appraise the outcome for both the Inhalants patient and codependent partner when Volatile solvents (paints, aerosols, glue, exhibiting enabling behaviors. gases) 34. Distinguish the difference in signs of Nitrates (butyl nitrite, amyl nitrite) intoxication, overdose, and withdrawal for Anesthetics (nitrous oxide, liquid, local) the following classifications of drugs: Club Drugs central nervous system depressants, MDMA (3,4-methylenedioxy- central nervous system stimulants, opiates, methamphetamine) marijuana, hallucinogens, inhalants, club MDA (methylenedioxy-amphetamine) drugs, and dissociative drugs. Eve/MDE (3,4-methylenedioxy- 35. Compare and contrast the symptoms seen ethylamphatemine) in alcohol withdrawal and alcohol delirium. GHB (γ-hydroxybutyric acid)
29 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
36. Relate knowledge of treatment in overdose Rohypnol (flunitrazepam) for central nervous system depressants, Nursing Diagnoses central nervous system stimulants, opiates, Outcome Criteria hallucinogens, inhalants, club drugs, and Planning dissociative drugs. Nursing interventions 37. Evaluate the relationship between blood FRAMES intervention alcohol level effects in a tolerant versus a Screening, brief intervention, referral to non-tolerant drinker. treatment (SBIRT) 38. Explore withdrawal treatment options for Recovery-oriented systems of care (ROSC) alcohol and opiate withdrawal in the Communication guidelines tolerant patient. Evaluation 39. Differentiate signs and symptoms of Dual diagnosis/Co-occurring disorders alcohol abuse in the older adult. Relapse prevention 40. Compare common reactions experienced Treatment modalities by nurses working with chemically Psychotherapy dependent patients and contrast them with Cognitive-behavioral therapy actual feelings while working with Motivational Interviewing chemically dependent patients in clinic. Transtheoretical model of change 41. Explore the prevalence of addictive Mindfulness and meditation disorders in health care professionals. Group Therapy 42. Propose clues that a nurse may be Family Therapy chemically dependent. Outpatient/residential programs 43. Appraise feelings one may experience Self-help groups when confronted with a co-worker abusing Psychopharmacology: substances at work and develop a plan for Alcohol Withdrawal intervention. Benzodiazepines
44. Propose nursing diagnoses for patients Thiamine (vitamin B1) with addictive disorders. Anticonvulsants 45. Formulate outcome criteria for withdrawal, Folic acid drug treatment and health maintenance. Multivitamins 46. Explore communication guidelines for Naltrexone (Trexan, Revia, Vivitrol) manipulation, denial, anger, impulsivity, Acamprosate (Campral) and grandiosity. Disulfiram (Antabuse) 47. Define patient centered nursing Quetiapine Fumarate (Seroquel) interventions for the patient with addictive Opioid Withdrawal disorders. Methadone (Dolophine)
30 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
48. Explore interventions based on the L-α-Acetylmethadol (ORLAAM) transtheoretical stage of readiness for Naltrexone (Trexan, Revia) change and FRAMES interventions and Clonidine (Catapress) Screening, brief intervention, referral to Buprenorphine (Subutex) treatment (SBIRT). Buprenorphine/naloxone (Suboxone) 49. Relate knowledge of dual–diagnosis principles. Anger, Aggression, and Violence 50. Explore relapse prevention strategies. Prevalence 51. Differentiate evidence-based Comorbidity psychotherapeutic options for chemically Etiology/Theory dependent patients. Assessment 52. Characterize outpatient and residential Predictive factors of violence treatment options for chemically Trauma-informed care dependent patients. Self-Assessment when working with 53. Explore the elements of self-help groups patients who have anger or aggression for the patient and significant others. Nursing diagnoses 54. Examine the prevalence and comorbidities Outcome Criteria of anger and aggression. Planning 55. Compare and contrast three theories that Stages of the violence cycle explore the nature of aggression. Interventions per stage 56. Analyze predictive factors of violence. Teamwork and Safety guidelines 57. Examine how self-awareness can directly De-escalation techniques affect the nurse’s ability to intervene safely Validation therapy in situations of anger and aggression. Restraint, medication, seclusion 58. Propose relevant nursing diagnoses for Documentation of a violent episode anger and aggression. 59. Relate outcome criteria for anger self- control. 60. Discriminate data necessary when planning interventions for anger self-control (patient characteristics, needs based on the situation, environmental qualities, staffing). 61. Differentiate between the stages of violence (preassaultive, assaultive, postassaultive, critical incident debriefing). 62. Compare and contrast nursing
31 Unit II Objectives Stress, Schizophrenia, Addiction, Anger & Aggression N343
interventions based on the stage of violence. 63. Explore the principles of de-escalation techniques. 64. Distinguish the four criteria for the use of seclusion and restraints over verbal intervention. 65. Relate guidelines for use of mechanical restraints (indications, legal requirements, clinical assessment, observation, release procedure, documentation, release protocols).
32