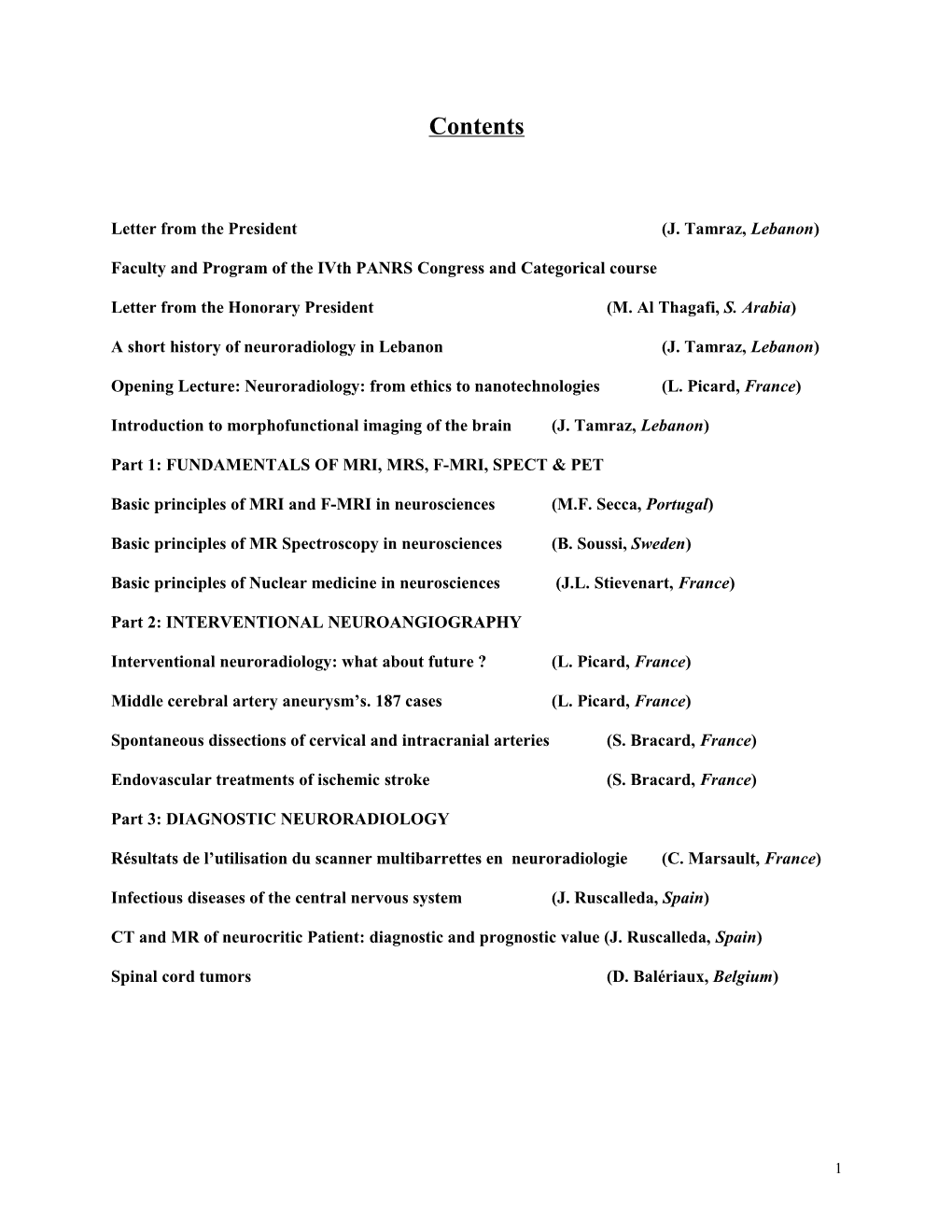
Contents
Letter from the President (J. Tamraz, Lebanon)
Faculty and Program of the IVth PANRS Congress and Categorical course
Letter from the Honorary President (M. Al Thagafi, S. Arabia)
A short history of neuroradiology in Lebanon (J. Tamraz, Lebanon)
Opening Lecture: Neuroradiology: from ethics to nanotechnologies (L. Picard, France)
Introduction to morphofunctional imaging of the brain (J. Tamraz, Lebanon)
Part 1: FUNDAMENTALS OF MRI, MRS, F-MRI, SPECT & PET
Basic principles of MRI and F-MRI in neurosciences (M.F. Secca, Portugal)
Basic principles of MR Spectroscopy in neurosciences (B. Soussi, Sweden)
Basic principles of Nuclear medicine in neurosciences (J.L. Stievenart, France)
Part 2: INTERVENTIONAL NEUROANGIOGRAPHY
Interventional neuroradiology: what about future ? (L. Picard, France)
Middle cerebral artery aneurysm’s. 187 cases (L. Picard, France)
Spontaneous dissections of cervical and intracranial arteries (S. Bracard, France)
Endovascular treatments of ischemic stroke (S. Bracard, France)
Part 3: DIAGNOSTIC NEURORADIOLOGY
Résultats de l’utilisation du scanner multibarrettes en neuroradiologie (C. Marsault, France)
Infectious diseases of the central nervous system (J. Ruscalleda, Spain)
CT and MR of neurocritic Patient: diagnostic and prognostic value (J. Ruscalleda, Spain)
Spinal cord tumors (D. Balériaux, Belgium)
1 Preface
Twenty five years have slipped by since first MR essays performed in vivo. The efficiency of MRI lies in many specific characteristics inherent to this method as its multiplanar ability to explore the patient without moving his body in the three planes, and in fact in any oblique orientation, or to bring out almost all the intracranial and spinal anatomical structures such as the leptomeningeal spaces, the CSF, the white and grey matter, the cranial and spinal verves and the vessels spontaneously visualized even without administration of any paramagnetic contrast media. The absence of beam hardening artifacts from bony structures as those generated in the posterior fossa or at the skull base vicinity, favors the explorations of tumoral processes developing in the orbitofacial region or in the base of the skull. The absence of ionizing radiation makes MRI the modality of choice for follow-up exams, which is of crucial importance in the pediatric field.
MRI is a multiparametric technique that largely depends upon the operator skill. It is also a complicated and highly evolutive imaging method. The choice of the appropriate pulse sequences is largely tributary of knowledge of the patient's clinical history, which contribute consistently to the final positive diagnosis. 3D reformations and volume renderings are powerful complimentary procedures available that add much to the preoperative planning of brain tumors. MR angiography is replacing to a large extent diagnostic conventional angiography.
The need for contrast administration such as the paramagnetic Gadolinium chelates contrast media, is relatively limited as compared to the wide use of iodine solutions with CT. Contrast infusion is usually restricted to infectious or inflammatory diseases, intraaxial and more particularly extraaxial tumoral conditions, base of skull lesions and most of the intraspinal and cord lesions.
Sophisticated techniques are presently used in a routine clinical basis: MR angiography without the need to invariably inject any contrast agent IV, evaluation of CSF flow circulation, without intrathecal injection of a contrast media, perfusion-diffusion imaging, ultra-fast imaging using Echo Planar Imaging, functional imaging, and in vivo MR spectroscopy. These recently implemented techniques on most available systems permit to obtain perfusion measurements using MRI, and identification of an infarct within the first few minutes following the clinical onset. MRI is the sole method available for direct study of the spinal cord. It is the technique of choice to perform to rule out non invasively spinal cord compression.
The search for an optimal cost/efficiency ratio requires first the prescription of the most informative exam. MRI stands as the modality of choice in many of such clinical conditions because it provides most of diagnostic necessities in the neuroimaging field. However, CT scanner remains useful in patients presenting absolute contraindications to MR exams (patients with pacemaker, vascular clips, neurostimulator, ferromagnetic devices etc...), or in cranial traumatology during the acute phase, or in case of suspicion of a subarachnoid hemorrhage in the first 48 hours. A combined approach may be needed for the evaluation of osseous abnormalities or the detection of minute calcifications.Conventional radiography of the skull or spine remain often useful and complementary of the MR exploration. Diagnostic angiography, remains the gold standard procedure for imaging of the vascular system, and MR angiography may be proposed as the primary screening method in conjunction with ultrasonography for the evaluation of extracranial and intracranial vascular systems. They are highly powerful non-invasive methods expanding in the routine practice.
MRI and MRA, MRS and f.MRI, may presently be considered as widely recognized diagnostic tools that have to be performed whenever possible even prior to CT, in any clinical circumstances necessitating to achieve an anatomical or a functional exploration of the head or spine.
2 A short history of neuroradiology in Lebanon (*)
Jean Tamraz, MD, DSc, Professor and Chairman, Department of Imaging, CHU Hôtel-Dieu de France, Université Saint-Joseph, POB : 16 6830, Beirut, Lebanon
Soon after the discovery of X-Rays by Roentgen (1895), the first chest X-ray was performed in thirty minutes using rudimentary equipment, in the French School of Medicine in Beirut, under the leadership of the French Maurice Collangettes S.J., chairman of physics (from 1900 to 1925).
At the same period of time, at the American University School of Medicine, were installed X-Ray systems (in 1900 and 1902), under the chairmanship of Arthur Bacon MD, who performed the very first X-ray of a chest, assisted by Nader Kaddoura MD (1907) and Toufic Hajjar MD (1910). From that time and until 1937, Professor Edward St-John Ward took in charge the radiology department, followed by Professor Kingsley Blake (1931-1934) then Albert Oppenheimer (1934-1934) with his assistants, William Shehadé MD and Georges Saleeby MD who became the head for two years.
The French School of radiology has undergone a major development in the year 1925 with the creation of the “Institut de Radiology et de Lutte contre le Cancer” inaugurated by Professor Regaud from the “Institut du Radium” of Paris. Doctor Lemarche was the first director, followed by Professor Chaumet (1934) who started giving courses in radiology and radiotherapy, and then by François Dupré La Tour S.J. (1941) and Professor Joseph Jalet (1943). From 1946 to 1975 the Institute was directed by Professor Paul Ponthus assisted by Afif Berbir MD and Fouad Boustany MD.
During the second half of the XXth century, general radiology developed under the leadership of several radiologists: Fouad Boustany MD, Fathi Homsy MD, Zahi Hakim MD, Jean Haddad MD, Joseph Haddad MD, and Riad Ghorra MD, from the French school, and Rafic Melhem MD, Philippe Issa MD, Naim Atallah MD, and Ghassan Rizk MD at the American University hospital. Georges Comair MD, trained at the Hôpital d’Instruction des Armées du Val de Grâce, in Paris, returned to Beirut and established a radiology department at the military hospital.
Neuroradiology emerged and individualised in the fifties thanks to the interest of neurologists and neurosurgeons. Early in the fifties, Fouad Sabra, Head of Neurology at the American University Hospital (AUH) performed the first pneumoencephalography and myelography with lipiodol (1951).Vertebral and carotid angiography by direct puncture were first performed respectively by Professor Fuad S Haddad, head of Neurosurgery at the AUH (1955) and by Professor Joseph Hajjar, neurologist (1957), followed immediately by Professor Sami Tohmé, Head of Neurology, at Hôtel-Dieu de France (HDF) University hospital, who performed also pneumoencephalography, angiography and myelography and developed EEG (1959). Ventriculography was initiated in 1962 by Professor Gedeon Mohasseb, Head of Neurosurgery and neuroangiography performed by Professor Raymond Chemaly, at HDF, until the installation of a seriograph for global or selective catheterisation using Seldinger procedures developped by Professor Pierre Zalzal, neurologist at HDF who devoted part of its time to neuroradiology and particularly angiography and air myelography until 1983. In the same period of time (1968) Professor Naim Atallah, Head of Neuroradiology, was performing all neuroradiological invasive techniques at the American University Hospital of Beirut.
With the advent of CT and MR, modern neuroradiology expanded. The first CT scanner (CGR ND 8000) dedicated to head explorations was installed at Hôtel-Dieu de France in 1980 by Professor Sami Tohmé, Head of Neurology department, who performed brain exams, long before the acquisition of a total
3 body scanner (CGR CE 12000) in the Radiology department under the chairmanship of Professor Fouad Boustany. Then came the MR era mostly devoted to neuroimaging and which tended rapidly to replace most neuroradiological exams. Three systems were purchased and installed in the country in 1991-1992, two mid-fields (0.5 T) and one high field (Signa 1.5 T) installed at Hôtel-Dieu de France and running under the direction of Professor Jean Tamraz, neuroradiologist and neurologist, Head of MR and Neuroimaging department since 1992 and Chairman of the department Imaging and Neuroradiology since 2001. The country is at present very highly equipped: 15 mid and 10 high field MR systems, 60 CT scanners, 4 multisclice CT, 22 angiography units, 15 nuclear medicine scanners, 8 centers for linear accelerators, a PET scanner, an EBT scanner and a PET-CT scanner.
(*) from “A History of Neuroradiology (1895-2002), E.A. Cabanis and MT Iba-Zizen Editors, Paris, 2002, pages 353-354, modified (published during the XVIIth symposium Neuroradiologicum, Luc Picard, President, Paris, France, August 18-24, 2002).
P.S.: The invaluable historical data have been collected from Fouad Boustany, Honorary Professor and Chairman of Radiology and Raymond Chemaly, Honorary Professor and Chairman of Neurology, at Hôtel-Dieu de France, Université Saint-Joseph, Beirut, Lebanon.
4 Letter from the Past President and PANRS bylaws
Mohammed A. AL Thagafi, MD Founder & Past President of the PANRS Director of the Radiology Department Armed Forces Hospital, Riyadh, Saudi Arabia
It gives me great pleasure to write this introductory letter for the Pan Arab Neurological Society (PANRS).
The concept of formulating this society started in May 1993 after the World Federation of Neuroradiological Societies had taken a decision to encourage the establishment of regional Neuro-radiological societies throughout the world, with the aim of improving this important sub speciality.
Dr. Hassan Sharif was the representative at the founding committee of the World Federation and attended the meeting in Vancouver. Under the guidance of the late Derek Harwood Nash, who was then the Acting Secretary General WFNRS. The idea of the Pan Arab Neuroradiological Society was born.
The Pan Arab Neuro-radiological society was established in 1994 at its founding meeting, which took place in Beirut, Lebanon. Attempts were made to include all Arab representatives but unfortunately, this proved to be logistically impossible. However, it was the President of the Pan Arab Neurology Society, Dr. Khalaf Al Moutaery, Dr. R. Rizk, the President of the Lebanese Radiology Society and Dr. Ashraf Kurdi, President of the Pan Arab Neurology Society. Their attendance was to witness the birth of the society on behalf of the WFNS.
A second and equally important reason for establishing a regional Pan Arab Society was that it was felt that the time had come to start putting together efforts to form serious scientific societies, arrange symposiums and education, with the aim of improving the practice of neuroradiology with this region.
As the society is still in its early stages, it is our intention to encourage the new generation of neuro-radiologists to join and take advantage of what we, as a society, can offer. Our future is reliant upon the support from each other so that we can ensure the best possible standards of Neuroradiological practice and facilities are maintained.
Since the establishment of the PANRS, we have had the opportunity to organise two Pan Arab African Society Symposiums. The first was in Cairo in 1996 for two days where both national and international speakers presented lectures on a wide range of interesting topics.
The second meeting will take place in Tunisia where once again a national and international faculty will be speaking about experiences within their field.
During the meeting, there will be an Executive Committee Board Meeting where we shall be discussing both the future of the society and ways of improving it.
I hope to see you all in Tunisia and other eminent scientific meetings.
5 PAN ARAB NEURORADIOLOGY SOCIETY (PANRS)
Constitution & By-Laws
ARTICLE I N A M E
The Pan Arab Neuroradiology Society (hereinafter called the Society) shall be composed of Neuroradiological Societies. Colleges, Academies and Kindred Neuroscience Associations Throughout the Arab World. The Society shall be based in (…) and shall have branches in other countries of tne Arab World.
ARTICLE II PURPOSE
1 – Objectives:
The purpose of the Society shall be the advancement of Neuroradiology in all its aspects and to represent Neuroradiology in the Arab World on matters of common interest by:
a - The establishment and maintenance of cooperation between Neuroradiological organizations in the Arab World.
b - The direction and enhancement of the prominent and effective position of Neuroradiology within radiology and the neurosciences.
c - The exchange and dissemination of knowledge ideas and recognized terminology in the field of Neuroradiology.
d - The development of the best possible standards of Neuroradiological facilities and practice.
e - The recommendation and encouragement of Pan-Arab accepted standards of education, training and research in Neuroradiology and its allied sciences.
f - The support of scientific Symposia and annual scientific meetings of member Neuroradiological sciences.
2 – Scientific Meeting of PANRS
A major activity that should evolve and progress shall be the holding of a timely and recurring “Scientific Meeting”. This should represent the scientific arm of the Society and should involve all members and allied neuroscience organizations and should be upholding the highest scientific ideas.
6 Whenever beneficial and advantageous, the Society should collaborate with established regional and international neuroscience groups in order to achieve its objectives.
3 – Other Activities
The Society shall pursue and will achieve its objectives through the following activities:
a - Promotion of scientific research and exchange of ideas in its fields and related topics and publish distribute and exchange such results with relevant Societies.
b - Holding regular conferences, symposia and seminars in the field of Neuroradiology throughout the Arab World.
c - Publish regular bulletins or periodicals to keep readers members up to date with Society’s programmes and progress of research activities.
d - Organize scientific expeditions and to award prizes for meritorious work in open competition.
4 – Foundation of the Society
The initial establishment of the Society shall be by a Founding Committee whose members are either leaders of established Neuroradiological societies or are recognized senior members of the subspecialty in their respective Arab countries. The founding committee shall cease to exist immediately the General Assembly holds its first meeting and a president and members of the Executive Committee and other officers of the Society are elected.
ARTICLE III MEMBERS AND MEMBERSHIP
The Society shall be composed of the following types of Member and Memberships:
A. Members:
Organizations of duly constituted Neuroradiological Societies from the Arab World as Members.
B. Affiliate Members:
Kindred Neuroscience Societies from the Arab World as affiliated member.
Application for membership will be submitted to the Executive Committee and shall contain:
1. A copy of the Constitution of the Society. 2. A list of the officers and members. 3. A report of the previous years Annual General Meeting of the Society and a description of the Societies Scientific activities, journals, etc.
7 C. Active Membership:
To be given to persons who satisfy the conditions of membership and whoever holds a University degree in the area of specialization of Society (Radiology, Neuroradiology). An active member should be resident of the Arab world and must pay the regular fees.
D. Associate Membership:
Associate membership shall be offered to qualified persons who would like to join but do not reside in the Arab world. Associates will be non-voting members.
E. Honorary Membership:
Shall be offered to persons who have contributed financially or otherwise towards the development of the Society within and outside the Arab world. An honorary member shall be chosen by the General Assembly of the Society on the recommendation of the Executive Committee. An honorary member is exempted from payment of registration and subscription fees. An honorary member may attend the General Assembly sessions, and other Committee meetings and take part in the discussions, but will not be eligible to vote on decisions or in elections.
F. Conditions and Procedures for Membership
An individual member of the Society should fulfil the following conditions:
(a) Must pay all dues of the Society. (b) Must submit an application to join the Society. (c) May be recommended by two active members of the Society. (d) Application for active membership should be submitted to the Executive Committee Membership is granted only after the approval of the Executive Committee.
All applications when complete shall review by the Executive Committee and its recommendations shall be submitted to the General Assembly for approval at its next meeting.
Election of Members
Organizations upon recommendation of the General Assembly, may be elected as members of the Society by two-thirds (2/3) affirmative vote of the members of the General Assembly, present and voting. The organization must be truly Arab in its continental arena, and should be primarily concerned with the general aspects of Neuroradiology.
Executive Committee
The Executive Committee, which manages the affairs of the Society, will be composed of not more than ------members chosen by the General Assembly in secret ballot and from among the active members of the Society.
The Executive Committee shall draw up the general policy of the Society and submit it to the General Assembly for approval. The Executive Committee shall also ensure that the functions of the Society are carried out and its objectives are realized.
8 Membership of the Executive Committee shall be for two years, which will be renewable. The Executive Committee shall hold an ordinary session at least once every two years. An extraordinary session may be held when requested by half or more of the members or by one fifth of the General Assembly or by the President of the General Assembly to discuss specific urgent matters (Define a quorum? 1/3 of voting members).
A member who is absent for more than three sessions without an acceptable excuse will be considered as having forfeited his membership.
Duties of the Executive Committee:
The Executive Committee shall issue rules and regulations necessary for the implementation of this statute. Other responsibilities of the Executive Committee shall include drawing the annual budget. Preparation of annual activities, future plans and fixes membership dues. The Executive Committee shall submit the above activities for approval to the General Assembly during the regular session.
President and Vice-President of the Executive Committee:
The General Assembly shall elect by secret ballot a President of the Executive Committee from the active members of the Society. The position shall be held for a period of two years, which will be renewable. The President of the Executive Committee shall be the President of the Society. The President has the right to suggest or choose names for the different committees of the Society.
Officers of the Society:
A. President B. Vice-president C. Secretary General D. Treasurer E. President of the scientific meeting F. Historian
Officers of the Scientific Meeting:
A. President B. Secretary C. Treasurer D. Members – at – Large (2)
General Qualifications of Officers:
All officers of the Societies and Scientific Meeting shall be active Neuroradiologists and full members of one of the Members of the Society. Officers may or may not have been delegates to the General Assembly.
Election of Officers. Terms and Duties:
All officers of the Societies and the Scientific Meeting shall be elected by an affirmative majority vote of the members of the General Assembly present and voting during the Meeting. The President may not be re-elected to this position.
9 Officers of the Societies :
1 - President
The President shall serve as the Chair of the Executive Committee and the General Assembly and shall be an ex-officio member of all Committees of the Society. The President shall exercise the usual authority and assume the responsibilities similar to that of the President of a scientific society. The President may appoint Special (Ad Hoc) Committees and the President with approval of the General Assembly shall be empowered to fill any vacancy which may arise in the offices of the Society, the Scientific Meeting and their committees if not otherwise provided in these by-laws.
2 - Vice President
The Vice President, who shall also be the President-Elect, shall assume the duties of the President if the President is absent or, for any reason, is unable to fulfil the duties of the office.
3 – Secretary General
The Secretary General shall be an ex-officio member of all committees of the Society. The Secretary General shall assume the usual duties and responsibilities of a Secretary General of a scientific society and those duties relating to the Society itself. The General Assembly and the Executive. The Secretary General shall be responsible for the day-to-day activities of the Society.
4 – Treasurer
The Treasurer shall assume the duties and responsibilities common to this office and shall chair the Finance Committee.
The Treasurer shall perform those duties typically related to dues and other monies received by the Society and expend such funds of the Society in accordance with the policies and approval of the Executive Committee and the General Assembly. The Treasurer shall provide the Executive Committee with an operating statement of the Society and the Scientific Meeting and balance sheet at intervals of no longer than twelve (12) months and then specifically at the meeting of the General Assembly during the Scientific Meeting. The Treasurer shall supply to the Audit Committee copies of treasury records prior to the Scientific Meeting.
7 –Historian
The Historian shall be elected by the General Assembly for the term of eight (8) years and may be re-elected.
The Historian shall keep the archives of the Society and of the past, present and future Scientific Meeting.
8 – All elected officers shall serve from the close of the Scientific Meeting at which they were elected until the end of the next Scientific Meeting with the exception of the Historian. This term shall be at least four (4) years.
10 Officers of the Scientific Meeting
All Scientific Meeting officers shall be active neuroradiologists and members of a neuroradiological society of the country in which the Scientific Meeting is to be held. They shall be nominated by the President of that Scientific Meeting and will be ratified by the Governing Council.
Scientific Meeting officers shall serve in office from the close of the Scientific Meeting at which they were elected to the end of the Scientific Meeting for which they were elected to manage its affairs until they are concluded and all financial matters sealed.
1 – President of the Scientific Meeting
The President of the Scientific Meeting shall be an ex-officio member of all committees of the Scientific Meeting and shall be a member of the Executive Committee of the Society. The President of the Scientific Meeting shall exercise the usual duties and responsibilities of a President of a scientific society but shall confine his her attention to those matters related to the Scientific Meeting. The President of the Scientific Meeting shall appoint all special (Ad Hoc) committees of the Scientific Meeting as are necessary to carry out its functions, and will chair its Scientific Program Committee. The President of the Scientific Meeting shall nominate the officers of the Scientific Meeting for ratification by the General Assembly.
The President shall propose the site and date of the Scientific Meeting for ratification by the Governing Council.
The President and Officers of the Scientific Meeting will be responsible for the high standard of the scientific contents of the Scientific Meeting, its scope and duration, and shall respect the principles customs and traditions of the past Scientific Meeting. The prime objective of the Scientific Meeting up to the time of creation of these By-laws was the presentation and discussion of research.
2 – Secretary of the Scientific Meeting
The Secretary of the Scientific Meeting shall be an ex-officio member of all Scientific Meeting Committees and a member of the Program Committee of the Scientific Meeting. The Secretary of the Scientific Meeting shall exercise the usual duties and assume the responsibilities of a secretary of a Scientific Society, which will confine attention to those matters related to the Scientific Meeting.
3 – Treasurer of the Scientific Meeting
The Treasurer of the Scientific Meeting shall assume the duties and responsibilities common to this office and that of a Scientific Society and be responsible to the President of the Scientific Meeting and the Executive Committee. The Treasurer shall accept all monies received by the Scientific Meeting, handle them suitably and expend any of those funds of the Scientific Meeting in accordance with the budget submitted to the Finance Committee of the Federation to whom the Treasurer is responsible and to whom the Treasurer must provide a full financial report at the completion of the respective Scientific Meeting.
4 – Members At-Large
One member at-large shall be the Chair of the local arrangements committee; the other Chair of the Technical exhibits Committee. Both shall be members of the Scientific Program Committee.
11 The number and responsibilities of such officers may be altered when necessary to accommodate local requirements according to geography or custom.
ARTICLE V GENERAL ASSEMBLY
1 – Composition:
a. Officers of the Executive Committee b. Delegates from Various Neuroradiological Societies from the Arab World c. Delegates from Associated Kinder Neuroscience Societies d. All Individuals Holding Membership of the Society
2 – Responsibilities
3 – Honorary President of the Society
The General Assembly shall comprise all active and eligible members who have paid or will pay their annual subscription fees. It will hold an ordinary session, at a fixed date once every two (2) years. The agenda of the meeting shall be prepared by the Executive Committee and invitations issued by the President.
The General Assembly may hold an extraordinary session at the request of the Executive Committee. Rules governing the ordinary session also apply to the extraordinary session meetings. The General Assembly session meetings are valid only in the presence of the majority of its members.
The General Assembly has the following responsibilities:
A. To issue by-law regulations for the organization of work in the Society. B. To approve the annual budget of the Society and the final financial statements every year. C. To approve the annual report of the Society activities prepared by the Executive Committee. D. To elect the President and members of the Executive Committee. E. To approve the annual plan presented by the Executive Committee. F. To discuss the items on the agenda and other matters that need to be studied by the members, within the sphere of the Society activities and to take necessary actions; and to choose an honorary President to the Society upon the suggestion of the Executive Committee.
Honorary President of the Society
The General Assembly appoints the honorary President of the Society upon the proposal of the Executive Committee. The Honorary President is to be a known public figure whose interests are related to the activities of the Society. The honorary President shall preside over meetings of the Society that he attends.
The Society’s Financial Resources and Budget:
The Society’s Financial Resources include:
12 1. Registration and annual subscription of the members. 2. Proceeds from the sale of the Society’s publications and printouts. 3. Dues from any workshops or training programmes held by the Society, and other institutions established to serve the purpose of the Society. 4. Gifts, grants, voluntary contributions and other financial support given to the Society by the Government or the public or private institutions or individuals and which the Executive Committee accepts.
The Executive Committee shall nominate from its members a Treasurer who will keep the society’s accounts and prepare the budget. The budget will be reviewed by the Executive Committee and ultimately be submitted to the General Assembly for approval.
The financial year of the Society shall begin on the first of November and end on the last day of October of the year after.
An Auditor shall be appointed to audit the Society accounts at the end of each financial year. The Auditor’s report shall be submitted to the Executive Committee and the General Assembly of the Society.
The Executive Committee may review and amend the responsibilities of the President, the Vice President, the Treasurer and the Secretary when the need arises.
13
Chapter II – M.F. Secca
Basic Principles of MRI and F-MRI in Neurosciences
Mario Forjaz Secca, PhD Professor de Biofisica, Departemento de Fisica Faculdade de Ciencias e Tecnologia, Universidade Nova de Lisboa, Lisbon, Portugal
Contents Introduction Basic principles of MR The nucleus and the spin The central equation in MRI Faraday's Law Spatial encoding Proton density Basic techniques and sequences of MRI RF Pulses FID Spin Echo Repetition Time T1 Imaging Gradient Echo Echo Planar Imaging Inversion Recovery STIR (Short TI Inversion Recovery) FLAIR MR Angiography Magnetization transfer Contrast agents (Gadolinium) Contrast Enhanced MRA Functional Imaging: principles and techniques Diffusion Perfusion Sequence comparison table Image parameters and contrast Signal to Noise ratio Contrast Spatial resolution Image artifacts Motion and Ghosting Respiratory artifact Magnetic Susceptibility Partial voluming Wrap around Chemical shift Bibliography
14 Introduction
Nuclear Magnetic Resonance (NMR) was originally a field of Physics, which overflowed into Chemistry, Biochemistry and Medicine. Several Nobel prizes have been won in this field. In the prehistory of NMR Isidor Rabi won the prize in Physics in 1944, because of his work on a resonance method for the registration of the magnetic properties of atomic nuclei. In 1952, Felix Bloch and Edward Purcell won the prize in Physics for the discovery of nuclear magnetic resonance in solids. Then, in 1991, Richard Ernst won the prize in Chemistry for his contributions to the development of the methodology of high resolution nuclear magnetic resonance spectroscopy; and in 2002, Kurt Wüthrich won the prize, also in Chemistry, for his development of nuclear magnetic resonance spectroscopy for determination of the three- dimensional structure of biological macromolecules in solution. Finally, in 2003, Paul Lauterbur and Peter Mansfield won the only Nobel missing for NMR: the prize in Physiology or Medicine. The prize was awarded for having made seminal discoveries concerning the use of magnetic resonance to visualize different structures, leading to the development of modern magnetic resonance imaging, MRI, which represents a breakthrough in medical diagnostics and research. The award came more than twenty years after the original work was performed, but it recognized the extreme importance that MRI has had in the field of Medicine.
One of the questions a physicist working in MRI is constantly asked by medical doctors is: What is Nuclear Magnetic Resonance Imaging and how does it work? The physicist normally answers rhetorically: How much Physics do you know? Or, how far are you prepared to go? Like everything else in life MRI can be explained at different levels, advancing more and more as the physical knowledge progresses; a bit like peeling an onion.
Starting from the outer layer we could explain how Magnetic Resonance Imaging works in a few lines, as follows.
The body is made up of atoms, a large proportion of which is Hydrogen. The nuclei of Hydrogen, which have only one proton, because they are charged and spin about themselves, behave like little magnets. These little magnets, when placed in a magnetic field align with it and rotate around the axis of the field in a movement called precession, similar to spinning tops on a table. This precession, or turning, movement is faster the higher the magnetic field. If electromagnetic radiation, like radio waves, at exactly the same frequency of the precessing nuclei is emitted near them they can absorb this radiation, which is said to be at resonance, and they flip, becoming aligned in the opposite direction of the field. When the radiation is switched off the nuclei get rid of the energy they absorbed by emitting back the radiation. Each tissue of the body, because of its different chemical composition and physical state, re-emits radiation at a different rate, known as the tissue relaxation time. This radiation is picked up by an antenna, transforming it into electrical current, which is then used to construct the image we want. Because nuclei are used in a magnetic field and absorb radiation at resonance the method is called Nuclear Magnetic Resonance Imaging. However because of the bad connotations of the word "nuclear" it has been dropped from the name and the method is usually know as Magnetic Resonance Imaging.
It is not the intention of this book to go too deeply into the Physics of MRI, so, to go to next layer, we will keep things simple and show only the essential and easily understood equations.
15 Basic principles of MRI The nucleus and the spin
All matter is composed of molecules, which in turn are composed of atoms. These atoms are constituted of a positively charged nucleus, made up of protons and neutrons, surrounded by negatively charged electrons. In the case of hydrogen the nucleus has only one proton and is surrounded by only one electron. The nucleus rotates upon itself, it has spin. And because it is charged it produces a small magnetic field, behaving like a tiny magnet. This produces what is called in Physics a nuclear magnetic moment.
The magnetic field The magnetic field is a disturbance in space produced either by a permanent magnet or by the passage of current through a loop of wire. It is a field of attractive or repulsive forces generated by moving or spinning electric charges and can be described as a set of imaginary lines that indicate the direction a compass needle would point at a particular position in space. Magnet fields strengths are measured in either Tesla or Gauss, where 1 T equals 10,000 Gauss. In the case of MRI most magnets are made up of loops of superconducting wire, which, because of their virtual zero electrical resistance at low temperature, can withstand very high currents in very thin cross-sections, without dissipation of energy, thus allowing very high fields in compact volumes. The main MRI field is commonly designated by B0.
The central equation in MRI
When a nuclear spin is placed in a magnetic field it tends to align itself with the main field. But, as in the case of a spinning top, it doesn't align completely, forming an angle with the field and rotating about the axis of the main field. This particular rotation is called precession and the angular frequency of precession is called the Larmor frequency and designated 0. If there is only one equation one should remember from Magnetic Resonance it has to be the Larmor equation:
0 = 2π f0 = B0 or f0 = 0 /2π = B0/2π This equation basically states that, for a particular nucleus, the higher the magnetic field the higher the frequency of the precessing nucleus. And it is this dependence of the frequency on the magnetic field that makes MRI possible. is a constant called the gyromagnetic ratio that has a particular value for each nucleus. For example, for Hydrogen, = 2.68108 rad/s/Tesla, and its precessing frequencies for the more common magnetic fields are given in the following table.
Field Frequency 0.5 T 21.3 MHz 1.0 T 42.6 MHz 1.5 T 63.9 MHz 2.0 T 85.2 MHz 3.0 T 127.8 MHz
These frequencies are in the range of VHF radio waves, from short wave to FM, hence they are referred to as radio-frequencies. Another consequence of this equation is that for a 1 ppm (part per million) increase in the magnetic field in a 1.5 T magnet the frequency will change from 42,600,000 Hz to 42,600,042.6 Hz. It is changes like this that allow an image to be acquired as we will see later on. It is possible to observe Nuclear Magnetic Resonance with many different isotopes, as is the case in the human body, in decreasing order of abundance, with hydrogen, 1H, Fluor, 19Fl, Sodium, 23Na, and Phosphor, 31P. However, because of its natural predominant abundance, Hydrogen is the nucleus of choice for MRI. Each isotope has a different , therefore, for the same field their frequencies will be different. For
16 example, for a field of 1.5 T the Larmor frequencies of the previous nuclei are shown in the following table.
Nucleus Frequency 1H 63.9 MHz 19Fl 60.1 MHz 23Na 16.9 MHz 31P 25.9 MHz
The alignment of spins In practice the nuclear spins do not all align with the magnetic field because of the thermal energy associated with temperature. In the simplest case of Hydrogen, with only two spin quantum states, the laws of physics state that there are only two possibilities for the spins: either aligned, in the direction of the field, or anti-aligned, in the opposite direction. Because the anti-aligned spins have an energy slightly superior to the energy of the aligned spins and this energy difference is of the order of the thermal energy for temperatures around body temperature, the spins are almost evenly distributed among the two energy levels. However, there is a slight difference, and it is this difference that allows us to obtain an image from the body. For example, for a field of 1.5 T the spin excess, the difference between the aligned and the anti- aligned spins, at a temperature of 37˚ C (98˚ F), is only of the order of 5 ppm. And it is this fraction that contributes to the signal. Fortunately, because of the very large number of nuclei, there are still enough spins to obtain a signal. As an example, there are around 71019 hydrogen nuclei in a volume of 111 mm3 of water, and a fraction of 5 ppm still yields a spin excess of 31014.
The net magnetization The net magnetization is then the sum of the magnetic moments of all the spins. In equilibrium it will be pointing in the direction of the magnetic field. It is this net magnetization that will produce the MR signal and to simplify the approach to MRI we will concentrate on the behavior of this magnetization as a single varying vector rather than the behavior of the individual spins. This is normally referred to as the classical approach as opposed to the quantum mechanical approach where we look at the individual spins.
The relaxation times T1 and T2 Now, if the spins are left on their own nothing in particular happens, but if electromagnetic energy, of the same magnitude as the difference in energy between the spin levels, is emitted near the spins in the form of radiation, they will absorb that energy, disturbing their equilibrium. Once that electromagnetic radiation is switched off the magnetization will return to equilibrium by re-emitting the energy absorbed. The return to equilibrium is not instantaneous and it can be decomposed in two parts, one along the direction of the main field and the other in the plane perpendicular to the main field. In equilibrium the magnetization has only a longitudinal component in the direction of the field and no transverse components in the perpendicular plane, but after the disturbance the longitudinal component is smaller in general and the transverse component appears. As the disturbance is switched off these components return separately to their equilibrium states, one returning back to the maximum net magnetization value and the other returning to zero. They both vary exponentially: the longitudinal component increases exponentially with a characteristic time known as T1 and the transverse component decreases exponentially with a characteristic time known as T2. The longitudinal time T1 is known as the 'spin-lattice' relaxation time because of its origin in the interactions of the spins with their surroundings. The transverse time T2 is known as the 'spin-spin' relaxation time because of its origin in the interactions between the spins, which cause a dephasing between them. The important point in imaging is that different tissues, because of their different chemical constitutions and different physical states, will have different relaxation times. In other words, T1 and T2 contain tissue information.
17 T2* In practice the transverse component is affected by external field inhomogeneities which cause additional dephasing and suppression of the signal and destroy tissue information. This means that, due to the faster transverse relaxation, T2 should be replaced by a smaller relaxation time designated T2*. Fortunately T2 can be extracted by recourse to a method known as spin echo.
Faraday's Law
Now that we have covered the basic physical principles of Magnetic Resonance, we have to understand the practical side of it (the engineering), that is, how to obtain a signal, and for that we have to understand the Law of Faraday. It states that if one moves a magnetic field inside a coil winding in the direction of the main axis of the coil an electric current is produced at the terminals of the winding. In equilibrium no signal can be detected because the net magnetization is constant, but by placing a coil perpendicular to the main field it is possible to monitor the disturbance as a varying transverse magnetization vector moving inside the coil. This will produce an electrical current that will be taken as the MR signal.
Spatial encoding
To construct an image it is essential to be able to tell what part of the body the signal is coming from. This is achieved by spatially encoding the signal. To understand spatial encoding we will start with a simple image. Let us suppose that we have a choir where each singer sings only one note and the singers for each octave are standing on the same line, with the lower octaves at the back and the higher octaves at the front; also, within each line, the singer on the left sings the lower note and the one next to him on the right sings the next semitone higher. If someone falls, and sings as he does, we can know exactly where it happened, even without looking, because we have encoded the frequencies. If the intensity of the singing is related to the speed at which the singer stands up again, just by listening to the sounds we have a way of telling what is happening to the choir. In imaging this encoding is achieved in practice by making use of magnetic field gradients and taking into account the Larmor equation. The gradients will produce a variation of the magnetic field along a particular direction of space, which will cause a variation of frequencies in that direction. Thus each point in space will produce a signal with a characteristic frequency which will enable the computer to separate the different points in space and reconstruct the image. For practical reasons the gradients in the different directions are not all switched on at the same time, but they are pulsed as the measuring sequence proceeds. The gradients applied in the three main axis are called the slice selection (SS) gradient, the frequency encoding (FE) gradient and the phase encoding (PE) gradient. To make the image acquisition technically possible the signal is acquired line by line until a full slice is obtained, going on then for the next slice.
Proton density
As the image is reconstructed it is divided in small equal volumes where all the spins inside each of them contribute to only one signal value. This means that within each of these volume elements (voxels) the signal assigned to it is an average of the signals of all the individual spins inside it. Each of these voxels will have a different quantity of spins inside it because of the different tissues it encompasses. The consequence of this is that different voxels will have initially different signals as a result of the particular concentration of spins, or protons of hydrogen, hence the designation proton density, which reflects the number of protons contributing to the signal that exist within a voxel.
18 Basic techniques and sequences of MRI RF Pulses
In practice the emission of RF frequency radiation is achieved in the form of a temporary variation of a magnetic field perpendicular to the main field. This field rotates at the resonant frequency and causes the net magnetization to rotate about it, thus disturbing it from its equilibrium state. This burst of radiofrequency energy is called an RF pulse. The longer the RF pulse is switched on the more the magnetization will rotate about it. In this way, by adjusting the pulse time width or intensity, it is possible to achieve a rotation of 90˚, 180˚ or any other angle desired. In MRI a group of RF pulses used to produce a specific type of signal is called a pulse sequence.
FID
The Free Induction Decay (F.I.D.) is the simplest signal obtained from a Magnetic Resonance sequence. By applying a 90˚ pulse the magnetization is rotated from the axis of the main field to a plane perpendicular to it. Because it continues to rotate around the main field in the plane perpendicular to B 0, it induces a current in the detecting coil and as the magnetization relaxes back to equilibrium, the signal decreases exponentially. This decay however is dominated by T2*, and not T2, dependant on the field inhomogeneities, which makes the FID very short in general.
Spin Echo
There is a way of recovering the T2 information that is masked by T2* and that is done by using a technique called Spin Echo. In this sequence a 180˚ pulse is applied some time (TE) after the original 90˚ pulse and some of the signal, originally lost after the FID, is recovered as a kind of echo that comes and goes. The best way to understand this process is to look at the system from the individual spin perspective. Right after the 90˚ pulse the spins, which are originally in phase, begin to dephase, some turn faster and others turn slower due to the spatial variations in magnetic field, causing the net magnetization to disappear quickly. However, when the 180˚ pulse is applied some time later the spins are reversed, that is the faster ones which moved further away from the origin now have a longer way to go to reach back the origin, while the slower ones which didn't move so far have a shorter way to reach back the origin. Because this movement of coming into phase is a mirror image of the dephasing movement they all reach the starting point at the same time and then restart to dephase. It is this temporary coming into phase that is called the spin echo. The main characteristic of the spin echo is that it retains the physical information about T2 and eliminates the influence of T2*, therefore an image based on the signal height of the echo is said to be T2 weighted. If, however, TE is very short, T2 relaxation has no time to occur, so the signal height will be proportional to proton density. This means that a spin echo with a short TE will be DP weighted and with a longer TE will be T2 weighted. The spin echo sequence implies that for a DP weighted sequence, the higher the DP the brighter the signal, and for a T2 weighted sequence, the longer the T2 the brighter the signal. (Fig.1)
19 Fig. 1 - Two axial images acquired in the same plane: (a) DP weighted image with a TE = 20 msec. (b) T2 weighted image with a TE = 90 msec.
Repetition Time
The repetition time (TR) of a sequence is the time between repetitions of the basic sequence of the imaging sequence. The sequence can be repeated for instance if it is necessary to improve the signal to noise. The repetition time is also the time taken to obtain each phase line measurement within a single slice, therefore the time required to produce an image is determined by the product of TR by the number of phase encoding steps. The TR can affect image contrast, making it one of the image parameters.
T1 Imaging
To obtain a T1 weighted image the spin echo sequence is repeated but with a short TR. This means that the net magnetizations of the tissues with short T1's will have time to recover to equilibrium but the magnetizations of the tissues with long T1's will have no time to recover. In this way tissues with shorter T1 will show brighter signals than the tissues with longer T1's. By varying the value of TR the contrast between the tissues with different values of T1 can be adjusted. (Fig. 2)
20 Fig. 2 - A spin echo T1 weighted axial image with a TR = 400 msec.
Gradient Echo
The spin echo sequence requires that the net magnetization recovers to its equilibrium position along the direction of the main field before repeating the sequence, and for tissues with a long T1 this can greatly increase the acquisition time. The incomplete recovery of the magnetization implies that there will be a signal loss. The gradient echo method allows a much faster acquisition by a combination of two techniques: a rotation of the magnetization less than 90˚ and a faster way of producing an echo. The purpose of rotating the magnetization less than 90˚ can be seen in the following diagram (Fig. 3).
21 Z direction F = 0Þ E = 15Þ E D = 30Þ D
C= 45Þ C
B B= 60Þ
A = 90Þ E D C B XY direction
Fig. 3 - Variation of the XY and Z components of magnetization with flip angle.
Let us consider several rotations of the magnetization, known as the flip angle, as shown in the figure. For a flip angle of 90˚ the magnetization only has components in the XY direction and no component in the Z direction, taking its full time to recover (approximately five times T1). For a flip angle of 45˚ the components in the XY and Z directions are equal, that is, about 71% of the net magnetization. For a flip angle of 30˚, the component in the XY direction is 50%, but the Z component is 87% of the net magnetization. For a flip angle of 15˚, the component in the XY direction is 25%, but the Z component is 97% of the net magnetization. As can be seen, the use of a small flip angle can produce a magnetization in the XY direction which is sufficiently large to yield a detectable signal but reduce very little the longitudinal magnetization, implying that it will recover to equilibrium more rapidly and allowing a much shorter TR. The faster way of producing an echo is achieved by the use of a special gradient rather than a sequence of 90˚-180˚ pulses. In this case a strong dephasing gradient, which will produce a dephasing faster than that caused by the external field inhomogeneities, is applied for a short time. At some point the gradient is reversed, causing the spins to rephase and go through a temporary echo a time TE after the original flip angle pulse. In the gradient echo it is the reversing polarity of the readout gradient that produces the echo, having no need for a 180˚ pulse. This allows the minimum TE to be reduced. One of the problems with the gradient echo, as opposed to the spin echo, is that it does have T2* effects from the external field inhomogeneities, manifesting themselves as a l oss of signal and geometric distortion which becomes worse as TE increases. This problem is more pronounced in the vicinity of interfaces with different magnetic susceptibilities, like air-tissue. The increased sensitivity of gradient echo pulse sequences to susceptibility effects makes them the methods of choice for perfusion imaging and brain functional imaging.
22 Echo Planar Imaging
Echo planar imaging (EPI) is a fast imaging technique that acquires an entire image within a single TR period. To fully understand this technique it is important to understand the strange concept of k-space as opposed to the image space. Let us start with an example, if we look at a cylinder from the top we see a circle, but if we look at it from the side we see a rectangle. One perspective shows us the roundedness of the cylinder while the other shows us its squareness. The object we are looking at is the same but we are highlighting its different properties by looking at it from different angles. And that is exactly what the image space and the k-space do, they look at the MRI from different perspectives, but describe the same phenomena. Fortunately there is a mathematical tool that allows us to convert from one perspective to the other and that is called the Fourier transform. The image itself is in the image space and the k-space is equivalent to the space defined by the frequency and phase encoding directions. While conventional sequences acquire one line of k-space for each phase encoding step, which occurs every TR seconds, EPI acquires all lines of k-space in a single TR period. This is achieved by cycling the phase and frequency encoding directions so as to cover the k-space of the image. There are several methods to obtain echo planar images, which include conventional EPI, spiral EPI and square-spiral EPI, whose names refer to the way k-space is covered. Because of the possibility of obtaining 15 to 30 images per second, depending on the acquisition matrix, one of the important applications of echo planar imaging is in obtaining ultra-fast images allowing real time acquisitions. There is, however, a price to pay for the extra speed and it is the image quality and sharpness.
Inversion Recovery
By applying a 180˚ pulse at the beginning of a sequence it is possible to invert the alignment of the spins from being aligned with the magnetic field to being anti-aligned. If the spins are then left to themselves they return back to equilibrium which is the aligned position. As they do that the magnetization goes from negative, through zero, to positive, that is, the magnetization recovers from inversion, hence the name Inversion Recovery. Because different tissues have different longitudinal relaxation times (T1) their magnetizations will go through zero at different times. If one starts a 90˚-180˚ spin echo sequence at exactly the time the magnetization of a specific tissue is going through zero, then that tissue will produce no signal. This time interval between the inversion pulse and the rest of the sequence is called the inversion time or TI. The main reason for using inversion recovery sequences is either to increase T1 contrast or to eliminate the signal from a particular tissue.
STIR (Short TI Inversion Recovery)
One of the specific inversion recovery sequences is used to eliminate the signal from fat and is called STIR (Short TI Inversion Recovery). This is achieved by using a short TI of around 150 to 180 msec, which is the time the protons from fat take to reach zero magnetization after being inverted. The main disadvantage of this sequence is the low signal to noise ratio because the magnetization of all the other tissues is also close to zero.
FLAIR
The other common inversion recovery sequence is used to achieve heavy T2 weighting without signal from the CSF. This sequence is called FLAIR (Fluid Attenuated Inversion Recovery). The signal from the CSF can be attenuated using a TI around 2000 msec, which produces a heavy T2 weighting of the images without virtually any signal from the CSF. The main disadvantage of this sequence is the necessity of very long TRs to allow the CSF to relax completely. (Fig. )
23 MR Angiography
MR angiography (MRA) is referred to as the ensemble of techniques that allows MR to image the flowing fluids in the body. In the past angiography was only possible with the injection of contrast in the blood vessels, but it would not distinguish between flowing and stationary blood. The methods of time-of-flight and phase contrast MRA, however, are sensitive to the flow of blood.
Time-of-Flight Angiography The Time-of-Flight (TOF) method makes use of the movement of blood through the imaging plane. For instance, for the spin echo acquisition of a slice through which a blood vessel passes, a 90˚ pulse affects the whole slice. However, when the 180˚ pulse is applied, the blood that has experienced the 90˚ pulse is already out of the slice so it does not contribute to the signal leaving a signal void, as can be seen from the figure. (Fig.4) 90Þ pulse 180Þ pulse
Flowing Flowing blood blood
Imaging plane Imaging plane Fig. 4 - Movement of blood magnetization away from the imaging plane.
This can be used for angiography by applying a 90˚ pulse outside the imaging plane, so that only the blood that flows into the plane within a time TE of the 90˚ pulse is prepared for the 180˚ pulse and will produce an echo. The rest of the slice will produce no signal. (Fig. 5) 90Þ pulse 180Þ pulse
Flowing Flowing blood TE blood
Imaging plane Imaging plane
Fig. 5 - Movement of blood magnetization into the imaging plane.
This method only works for flow into the plane and will not take into account flow in the plane.
Phase Contrast Angiography
24 The phase contrast (PC) method works on a different principle, making use of the dephasing produced on the spins by a non-linear bipolar magnetic field gradient, that is, one which has two lobes, one positive and one negative. If the positive lobe comes first the bipolar gradient is said to be positive and if the negative lobe comes first the gradient is negative. The positive lobe of the gradient will dephase the spins in one direction and the negative lobe will dephase in the opposite direction. If the spins are stationary the total dephasing will be zero, that is, the stationary spins will not be an affected. But if the spins have a velocity component in the direction of the gradient, the dephasing of the different lobes of the gradient will not be compensated. In PC angiography two imaging sequences are performed, the first one with a positive bipolar gradient pulse and the second one with a negative bipolar gradient pulse. Then the raw data from the two is subtracted. The signals of the stationary spins cancel and the moving spins have a net signal, producing an image of the flowing spins. To obtain the optimum signal, the spins of the fastest flowing blood should acquire 90˚ of phase after each bipolar gradient pulse, or 180˚ in total. All the other spins with slower velocities will acquire smaller phase shifts. Only those spins with a component in the direction the bipolar gradient will produce a signal. . With PC angiography it is possible to obtain quantitative measurements of velocities both for vascular flow and for CSF flow, by means of adequate software, that will convert phase measurements into velocity values. It is also possible, by measuring vessel areas, to obtain fluid flow rates. (Fig. 6)
Fig. 6 - (a) Axial oblique plane perpendicular to the Aqueduct showing the flow area measured. (b) Graph of the average CSF flow through the cardiac cycle. (c) Summary table of the flow parameters calculated.
Magnetization transfer
The hydrogen nuclei in the body exist not only in water and fat but also in other macromolecules like proteins. However these protons do not contribute to the MR signal because they have a very short T2 relaxation time, since they are tightly bound. They are in fact excited at the same time as the water protons, but their signal decays in less than a millisecond. In MR a system that has a short T2 responds to a very large range of frequencies and a system with a large T2 responds to a narrow range of frequencies. This means that the protons bound to the macromolecules can respond to an RF pulse shifted, for instance, 1500 Hz, from the resonant frequency of the water protons, without affecting these. However, the protons of water bound to these macromolecules will interact with them and will become partly saturated. In this way the signal from highly proteinated tissues, like brain, liver and muscle, will become suppressed. (Fig. 7)
25 Water protons
Presaturation pulse Protons bound to macromolecules
1500 Hz shift Fig. 7 - Diagram for the magnetization transfer process.
Magnetization transfer is used normally to improve the suppression of the signal from brain and muscle when performing MRA TOF, but it can also be used to obtain information on the protein contents of some tissues.
Contrast agents (Gadolinium)
Although MRI is a very powerful imaging technique not all pathologies are clearly contrasted using only proton density or relaxation times weighting. For example, some meningiomas and small metastatic lesions do not show on normal imaging. And considering that some of these intra-cranial lesions have an abnormal vascular bed or a breakdown of the blood-brain barrier, a magnetic contrast agent that distributes throughout the extracellular space became an obvious choice to improve image contrast. Some purists believe that the fact that MRI is a non-invasive method is one of its strengths and should be kept that way, but the clinical efficacy of the paramagnetic contrast is more than proven to amply justify its use. All the common contrast agents used in MRI are Gadolinium chelates, which are not directly imaged but produce an effect, which is imaged. Gadolinium is the element of choice because of its high number of seven unpaired electrons. Each unpaired electron has a magnetic moment 657 times bigger than that of a proton, so seven unpaired electrons can induce relaxation a million times better than an isolated proton. This implies that both T1 and T2 are reduced, although the enhancement caused by the shortening of T1 is stronger than the signal loss caused by the shortening of T2; and that is why with Gadolinium contrast the images obtained are normally T1 weighted. The actual amount of T1 shortening is dependent on the concentration of Gadolinium injected and the signal enhancement depends also on TE and TR.
Contrast Enhanced MRA
One of the recent uses of MR contrast agents is in MR angiography. The injection of the contrast into the blood reduces the T1 relaxation time in the blood vessels relative to surrounding tissues, therefore a rapid volume imaging sequence with a short TR value will produce a large signal for blood and a very small signal for the long T1 tissues surrounding the blood vessels. This technique enables the acquisition of very good vessel images without recourse to the flow properties of blood. It works in the same way as digital angiography but is not selective. One of the advantages is the possibility of imaging vessels with awkward geometries and turbulent flow, which are difficult to obtain using standard TOF or PC angiography. Because of the high quality of contrast enhanced MRA (CE- MRA) images it is becoming the modality of choice in MR angiography. (Fig. 8)
26 Fig. 8 - A CE-MRA image showing the carotids all the way from the aorta.
Functional Imaging: principles and techniques
The term Functional Imaging in MRI is a very general term that covers any technique that gives functional information rather than just anatomical information. That is, any technique that acquires time dependent imaging data should be called functional imaging. Flow, perfusion, diffusion, tagging and brain activation belong to this category. However, when functional magnetic resonance imaging (fMRI) is mentioned it is normally referred to brain activation. In this section we are concentrating on this latter technique. Brain activation can be studied either by direct methods, those that measure directly the electrical activity of neurons, like EEG (electrical effect) and MEG (magnetic effect); or indirect methods, those that measure the hemodynamic response to the neuronal electrical activity, like 15O PET (blood flow) and fMRI (BOLD effect). The indirect method used by fMRI can be understood by following the chain of physiological events that describes it. When a set of neurons fire, there is a local increase in glucose consumption which in turn produces an increase in oxygen consumption. This induces an increase in regional cerebral blood flow (rCBF) and an increase in regional cerebral blood volume (rCBV) with a consequent increase in blood velocity. In the blood there is a decrease in oxygen extraction fraction producing an increase in oxyhemoglobin and a decrease in deoxyhemoglobin. In this sequence of events the most common approach used in fMRI is the Blood Oxygen Level Dependent (BOLD) contrast. The decrease in deoxyhemoglobin, because of its high paramagnetism, produces a decrease in local microscopic field gradients, which in turn produces an increase in T2*. This corresponds to an increase in signal, which is measured by the MR equipment. The ideal sequence to use is a rapid sequence with T2* sensitivity, which detects changes in magnetic field, usually a Gradient Echo EPI. fMRI has its own limitations both in spatial resolution and temporal resolution. In terms of spatial resolution, although for a standard image the voxel volume is, approximately, 3 3 5 mm3, it is theoretically possible to go down to 0.5 0.5 1 mm3. The temporal resolution is limited by the hemodynamic lag of 4 to 8 sec in the response to the neuronal electrical activity and the speed of the scanner hardware, presently of the order of 10 frames per sec. To achieve optimal functional imaging it is important to have the highest possible magnetic field, powerful and fast gradients and a powerful computer with adequate software to manipulate the image.
27 The pulse sequence used will look for small variations in the signal of the T2* weighted image. Since these variations are very small it is necessary to obtain a large number of images as the activation paradigm is performed. The paradigms normally consist of blocks of 30 sec of rest followed by 30 sec of activation. During rest no activity is maintained. During the activation period the task being studied is performed. The activation can be motor, sensory, visual, auditory, language generation and others. The images obtained directly from the system do not show any visible characteristic to the naked eye. It is necessary to treat the images mathematically by comparing the variation of intensity of the pixels in a certain image as a function of time with the variation that one would expected in the theoretical ideal case of the particular activation paradigm, which corresponds to a square function. This comparison is done statistically, pixel by pixel, and colour coded to indicate if they are more or less correlated with the activation paradigm. The final images are then obtained by superimposing the statistically processed EPI images on the anatomical images obtained for the same slices. It should be noted however that the images obtained with the EPI sequence are very sensitive to changes in magnetic susceptibility and can be heavily distorted. It is normally necessary to correct the EPI images by computer. It is important to stress that there can be false positive signals, due in particular to blood vessels and eye movement. (Fig. 9)
Fig. 9 - A functional image showing the language premotor cortex activation for a phonetic language generation paradigm.
There are several clinical applications for fMRI now being tried like tumor surgery planning, AVM’s, epilepsy, addiction, schizophrenia and AIDS. Functional brain activation imaging with MR promises to be clinically useful, but only with a more robust and complete image processing and being very careful with the definition of the paradigm used and the verification of its implementation.
Diffusion
While MR angiography and flow measure the movement of spins from voxel to voxel, MR is capable of measuring microscopic translational motion within each voxel. This motion can be the molecular diffusion of water and the microcirculation of blood in the capillary network, referred to as perfusion. Diffusion is the process by which molecules and other particles mix and migrate due to their random thermal motion. Diffusion imaging is acquired in a similar way to phase contrast angiography, using a specific bipolar gradient with very high strength and duration of the gradient lobes to detect the slow molecular diffusion in the body. This bipolar gradient will cause a signal loss in the diffusing spins, which depends on the
28 diffusion coefficient and the b value. The b value is determined by the strength and duration of the gradients and has units of s/mm2. High b values can eliminate the T2 effect and improve the visualisation of the white matter fibres and can be useful to differentiate sub-acute from chronic infarcts. (Fig…) It is possible to obtain maps of diffusion in the three different orthogonal directions, or combine the three images into a single map of overall diffusion. With specific research software it is possible to calculate the diffusion tensor and deduce the actual direction of the diffusion, and even obtain the direction of the neuronal axons. (Fig. 10)
Fig. 10 - Two images on the same location of a patient with infarcts. (a) A FLAIR image on the left and (b) a diffusion image on the right.
Perfusion
Perfusion in MRI is the study of the net transport of magnetization into a volume of tissue, which refers to the capillary blood flow to the tissue, measured in ml/min.g. This technique requires the use of a contrast agent to distinguish the perfused from the unperfused tissue and it can be performed either with endogenous or exogenous contrast agents. The more common perfusion technique, known as Dynamic Susceptibility Contrast (DSC), is achieved by injecting a bolus of contrast agent, like Gadolinium. A rapid EPI series of slices is acquiring through the region of interest and then repeated at a rapid rate, of the order of one per second, as the contrast is injected. This repetition is performed from just before the injection until about 30 seconds to a minute after the arrival of the bolus. For most people best results are achieved with the use of a power injector, which can produce a steady injection rate of between 3 and 5 ml/s, hard to achieve by hand. After acquisition it is necessary to perform some quantitative analysis of the images to look for variations in the arrival of the contrast agent between the pathological and normal regions. This is performed either on the manufacturers workstations or with specific software. The blood flow to the brain tissue is known as cerebral blood flow (CBF), but two other quantities are of interest in perfusion: the cerebral blood volume (CBV) and the mean transit time (MTT). However, because these absolute quantities are difficult to quantify, they are normally replaced by their relative values, indicated respectively by rCBF, rCBV and rMTT, but it is normally preferable to compare the values from the ipsi-lateral and contra-lateral side. On a first approach, the parameters measured directly from the concentration time curves, like the negative enhancement integral, the bolus arrival time and the time to peak, and the peak height can be
29 approximately related to rCBV, rMTT and rCBF, however they are strongly dependent on the shape of the bolus. The pixel by pixel analysis of the images for the required parameters is usually presented on a colour coded scale, overlaid on an anatomical image, producing images similar to those of nuclear medicine. The other perfusion technique, known as Arterial Spin Labelling (ASL), uses the magnetic tagging of protons in the arterial blood supply, thus avoiding the injection of an external contrast agent. This tagging can be achieved by applying a saturation pulse to the feeding arteries, which prepares the blood before it enters the slice of interest, and then acquiring an image of the slice. Following that, a second image acquisition is obtained, but with a different tagging excitation. By subtracting the two images, signal differences are obtained only in the regions where the tagged blood has reached. Because of the small signal it is normally necessary to average over a large number of acquisitions. ASL has the disadvantage of only producing CBF and not CBV or MTT, but it has the advantage of being sensitive to brain activation.
Sequence comparison table
With the evolution of MRI many manufacturers started developing their own sequences, or their versions of the standard sequences. Some of these sequences although slightly different and called different names are practically equivalent. This diversity of nomenclature can introduce some chaos in the field when dialoguing amongst different platforms, since it is important to know if the same sequences are being used for a particular study. With this in mind we present a sequence comparison table where equivalent sequences for four of the major manufacturers are presented on the same line.
Sequence comparison table.
Image parameters and contrast Signal to Noise ratio
The main parameter to assess signal quality is the Signal to Noise Ratio, designated by SNR. This is defined as the ratio of the average signal over the standard deviation of noise. The signal comes only from the spins that were excited intentionally when selecting the slice, or volume, of interest and the noise comes from many other sources, the main one being the patient. As mentioned above, only the spin excess between the aligned and anti-aligned spins contribute to the signal, but all the other spins, as they jump up and down from the two energy levels, can emit a random radio-frequency photon, which contributes to the background noise. Obviously if the sensitive volume of the coil is large it will detect a large number of these random transitions, producing a large noise. Therefore the smaller the coil the closer it will be to the excited spins, producing a larger signal, and detecting fewer random transitions, consequently producing less noise; that is, a smaller coil will have a higher SNR. For example, a head coil has a higher SNR than a body coil, and a small surface coil placed close to the anatomy of interest will have an even higher SNR than the head coil. There are several factors affecting SNR, like voxel size, number of excitations and bandwidth. The voxel size affects the signal and the other parameters affect the noise. The larger the voxel size the larger the number of spins inside it, so the signal is directly proportional to the voxel size within a tissue of uniform spin density. The SNR also depends on the number of excitations, but not in a linear way. In fact the SNR is proportional to the square root of the NEX, for example, going from 1 to 4 NEX only improves the SNR by a factor of 2. Another factor that influences the SNR if the receiver bandwidth, but here the dependence is inverted, the SNR is inversely proportional to the square root of the bandwidth, that is, if the bandwidth is increased by a factor of 4 the SNR is decreased by a factor of 2.
30 Contrast
Contrast is the relative difference between the signals of adjacent voxels and can be defined as the difference of signal intensities divided by the average signal intensity in two adjacent regions. To differentiate one tissue from another it is very important to increase the contrast between them. The main factor determining the tissue contrast is the choice of sequence and its parameters, since for a particular sequence each tissue will have a particular signal height. For example, to differentiate a tumor from the surrounding tissue it is essential to choose a sequence that maximizes the contrast between the tumor and the surroundings. Once the image is acquired it is possible to improve the contrast by manipulating the image in the post- processing stage, but this should be done very carefully because it can mask the original information obtained.
Spatial resolution
The spatial resolution of an image is determined by the number and size of points composing it and it will determine the smallest anatomical structure that can be resolved. It is inversely related to voxel size, the higher the spatial resolution the smaller the voxel size. The two main factors determining spatial resolution are the field of view (FOV) and the matrix size. If you diminish the FOV maintaining the same matrix the voxel size goes down and if you maintain the FOV but increase the matrix the voxel size goes down as well. We should bear in mind that if the matrix size is doubled, for instance from 256x256 to 512x512, the number of voxels goes up by a factor of four and their volumes go down by a factor of 4. Therefore, as the resolution goes up the voxel size goes down and this implies that the SNR goes down as well. As always in MRI there is a price to pay for a particular improvement.
Image artifacts
MRI has a multitude of factors that affect the appearance of the image and this makes it very interesting and rich. However, one of the problems with this is that it is possible that a few of these factors will go out of control producing an image that does not reflect the real state of the anatomy, in other words, the image will have artifacts. Although sometimes artifacts may destroy the quality of the image, with the possibility of making it useless, some other times they can just be ignored, but the major danger of some of the artifacts is that they can be confused with pathology, leading to misdiagnosis. Therefore it is important to understand the aspects and the causes of the major artifacts and how to deal with them. All manufacturers have a series of standard techniques to eliminate or compensate for the major artifacts.
Motion and Ghosting
The most common cause of image artifacts is patient motion. Random motion will just produce a blurred image and is avoided by asking the patient to be still or sedating in extreme cases. However, not all movement can be controlled by the patient, for instance, the blood keeps on pulsating. And any motion that occurs regularly in a repeating pattern will not cause a blurred image, but will produce one or more 'ghosts' in the phase encoding (PE) direction. If the 'ghost' occurs inside the image it can produce either a darker or brighter area in the surrounding tissue that can confused with pathology. The way to avoid this artifact or at least reduce it is by using cardiac gating or a spatial presaturation pulse on the side of the incoming blood. Sometimes, if it is unavoidable, changing the order of the phase
31 encoding and the frequency encoding gradients shifts the 'ghosting' to an area that is not important and leaves the area of interest clear. (Fig. 11)
Fig. 11 - An image showing both a motion artifact on the left and right and a blood flow artifact running from left to right.
Respiratory artifact
Another source of periodic motion is respiration, and this can also cause ghosting, but because it is the whole chest and abdomen that moves the artifact appears above, below and throughout the body. This artifact is avoided either by using respiratory gating, improving the quality of the image significantly but doubling, or more, the acquisition time, or by using a method known as respiratory compensation, which will clear the coherent 'ghosts' above and below the image but will produce a slight blur all across it. (Fig. 12)
32 Fig. 12 - An image showing a respiratory artifact, from top to bottom.
Magnetic Susceptibility
To obtain good MRI images it is essential that the magnetic field is as homogeneous as possible, because the spatial encoding is based on a precise distribution of the linear field gradients. Unfortunately there are several things that can distort the magnetic field affecting adversely the quality of the image. The main parameter affecting the homogeneity is the magnetic susceptibility, which says how much a substance will be magnetized when placed in a magnetic field. This can be a problem not just due to the presence of foreign objects within the body but also due to differences in magnetic susceptibilities of adjacent tissues. If the magnetic susceptibility of the region being imaged is fairly homogeneous there will be no major changes in the magnetic field. However, if the magnetic susceptibility of adjacent tissues differs much, like the transition between air and tissues (lungs and sinuses), there will appear an artifact at the separating edges. Because of their high magnetic susceptibility, the presence of metallic objects (like dental implants, clips and shunts) within the volume to be imaged will distort drastically the local magnetic field and it is possible to have a total loss of signal in a particular region, surrounded by a strong distortion of the signal.
Partial voluming
Normally the width of the voxels, that determines the resolution in the imaging plane, is smaller than their depth, except in the case of 3D volume acquisitions. This depth, called the slice thickness, is normally of the order of 5 mm. If a group of voxels incorporates the edge of a structure there will be a blurring of the image around these voxels because their volume averages the signal from different tissues. This process is called partial volume. The way to diminish this problem is to reduce the slice thickness.
Wrap around
The phase encoding (PE) gradient produces a phase shift in the spins that varies between 180˚ and –180˚. However if the field of view is too small there will be excited tissue outside the FOV, producing phase shifts above 180˚ and below –180˚. Because the equipment cannot measure phases outside the 180˚ and – 180˚ range, values above 180˚ will be confused with those near the –180˚ and values below –180˚ will be confused with those near the 180˚. As an example, some tissue outside the FOV assigned a phase shift of 190˚ will be confused, in the reconstruction, with the tissue inside the FOV assigned a phase shift of -170˚. This will produce what is called a wrap around in the PE direction. In a sagittal slice of the head this can cause the nose to appear on the back of the head. (Fig. 13)
33 Fig. 13 - An image showing a wrap around artifact, with the nose and mouth appearing at the back of the head.
Chemical shift
The different chemical environment of the nuclei of hydrogen in water and fat produces a slightly different magnetic field around them, that causes the protons in fat to resonate at a frequency lower than the protons of water. This difference is 3.5 ppm, which at 1.5 T corresponds approximately to 224 Hz. One consequence of this is the appearance of white and dark bands at fat/tissue boundaries, as is exemplified in the figure below. (Fig. 14)
Fat
Water Original object
Frequency encoding gradient
Image obtained
Signal Water Water void and Fat Fig. 14 - Diagram showing the original object and the image obtained due to chemical shift.
34 The image reconstruction computer assumes that a spin with a particular frequency comes from a particular point in space. However, because the fat protons have a resonant frequency lower than that for the water protons, along the frequency encoding gradient all their spins will be considered to come from a slightly displaced position when compared with the water protons. This can have two effects. One is producing a dark band, or signal void, in an area where the fat signal should be but no water exists. The other is the appearance of a white band due to the existence of two different signals, from water and fat, with exactly the same frequency which add up. By exchanging the frequency and phase encoding gradient directions these artifacts can disappear from some of the boundaries.
Note
All the images shown were obtained on a 1.5 T GE CVi system at Ressonancia Magnética de Caselas, Lisbon, Portugal.
Bibliography
– “All You Really Need to Know About MRI Physics” Moriel NessAiver. Simply Physics, Baltimore, 1997. – “Physics of MR Imaging. Magnetic Resonance Imaging Clinics of North America. Volume 7, Number. 4, November 1999” Ed. J. Paul Finn. W. B. Saunders, Philadelphia, 1999. – “Magnetic Resonance Imaging. Physical Principles and Sequence Design” e. Mark Haacke, Robert W. Brown, Michael R. Thompson, Ramesh Venkatesan. Wiley-Liss, New York, 1999. – “MR Imaging Abbreviations, Definitions, and Descriptions; A Review” Mark A. Brown, Richard C. Semelka. Radiology, 647, Dec. 1999. – “Magnetic Resonance in Medicine. 4th Completely Revised Edition” Peter A. Rinck. Blackwell Wissenschaft-Verlag, Berlin, 2001. – “MRI From Picture to Proton” Donald W. McRobbie, Elizabeth A. Moore, Martin J. Graves, Martin R. Prince. Cambridge University Press, Cambridge, 2003. – “Quantitative MRI of the Brain. Measuring Changes Caused by Disease” Paul Tofts (Ed.). Wiley, Chichester, 2003.
35 Chapter III – B. Soussi
Basic principles of MR Spectroscopy in Neurosciences
Bassam Soussi, MD, PhD Professor and Director of NMR Research Lab & Bioenergetics Grp, Wallenberg Laboratory, Sahlgrenska University Hospital Gothenburg Unviersity SE-413 45 Göteborg, Sweeden
AIM OF CHAPTER
The aim of this chapter is to provide a comprehensive introduction to the new possibilities that Magnetic Resonance Spectroscopy (MRS) offers in clinical neurosciences. Focus will be on what MRS can do rather than what MRS is. For simplicity, basic physical and chemical principles will not be much explored and are referred to elsewhere.
INTRODUCTION
For over half a century, interest in Nuclear Magnetic Resonance (NMR) has bee n continuously increasing. From structural analysis in smaller organic molecules, to biochemical macromolecules, tissue extracts, isolated intact organs and in vivo studies in animals and humans.
For almost two decades, in vivo MRS has been a revolutionary technique in biomedical research. Today, it is a powerful tool in neurosciences giving noninvasive access to the chemistry of the human brain in health and in disease.
Nuclei like 31P, 1H, 13C, 19F and 23Na have been studied in various organs. However, early applications of in vivo MRS began with the measurements of 31P metabolites in isolated organs and surface regions like skeletal muscles from intact animals.
Historically, 31P has been the most studied nucleus. However, MRS of the brain today relies mostly on 1H examination due to its relative ease i.e. high natural abundance (99.9%) and sensitivity (100%). Numerous studies have shown that MRS can detect pathophysiological changes in the brain tissue in a number of diseases.Therfore, this chemically specific technique with its ability to examine the mechanisms of disease is continuously gaining attention from clinicians.
In vivo MRS should be seen as complementary to the well established clinical MRI, providing quantitative nondestructive analysis of the biochemistry of the brain cells without the use of radioactive tracers. It is possible to integrate spectroscopy with conventional MRI equipment of 1.5T or higher magnetic field by adding appropriate hardware and software available from MR manufacturers.
Theoretical background MR theory is described elsewhere. For more detailed physical and chemical aspects of the technique see references.
The basic principles for MRS are the same as for MRI. It is suitable however, to mention some aspects that are related to spectroscopy. Briefly, and put in its simplest form:
36 The interaction between atomic nulclei (possessing a spin that gives a magnetic moment) and radio waves when an external static magnetic field is applied gives rise to a electromagnetic signal.
The electromagnetic signal obtained after the application of a 90° radiofrequency pulse is called free induction decay (FID).
At the same time, each nucleus is charecterized by the time constants T 1 (longitudinal relaxation) and T2 (transveral relaxation).
The decaying signal is the result of the relaxation of the nuclei from their excited state to their relaxed state.
The FID is then converted to a spectrum by a Fourier transformation (mathematical algorithm).
The “spectral“ chemical shift ( ) is measured in parts per million, (ppm) and is a characteristic of the variation in resonance frequency. Its specific dependency on the chemical environment of a particular nuclei makes it like a “finger print“ of the analyzed substance. Figure 1 shows the conversion of a FID to a spectrum by Fourier transformation.
Localization “Image guided spectroscopy“
Figure 2 (A, B) ilustrates the selection of a volume of interest (VOI) based on a topographical MR image in order to acquire a proton MR spectrum. The same strategy is used in the example in figure 3 to get a 31P MRS localization based on a topographycal MRI.
Localization methods
Early localization methods started with surface coil localization which is based on RF pulses and the use of surface coils for spatial localization. A disadvantage of this procedure is surface tissue contamination of the spectra.
Multi-shots methods
ISIS Image -selected in vivo spectroscopy (ISIS) uses a combination of 8 pulses. The VOI is pre-selected, based on MRI scan and is repeatedly excited. The ISIS method has been applied to both 31P and 1H. One advantage of this method is that it can be used without T2 weighing. However, the eight phase cycles used in localization might make shimming difficult.
Single-shot methods
Two methods are widely used and basically similar.
1) STEAM Stimulated Echo Aquisition Mode (STEAM) uses a stimulated echo generated by three 90°pulses (90°- 90°-90°). It is mostly used in 1H spectroscopy. Signal loss due to motion sensitivity at long echo times is a
37 disadvantage. This method is suitable for short TE acquisitions.
2) PRESS Point Resolved Spectroscopy (PRESS), involves a double spin echo scheme (90°-180°-180°) which theoretically gives improved S/N. This method is most suitable to 1H spectroscopy where small volumes and/or metabolites with long relaxation times T2 are of interest.
Chracteristic patterns seen in STEAM and PRESS spectra in patients with acute brain injury are shown in fig 6.
Spectroscopic imaging
Spectroscopic imaging is the simultaneous acquisition of spectra from many volumes using phase encoding. It is suitable for both 1H and 31P. This method offers the advantage of investigating many slices simoulnateously. However, the S/N is lower the an in single-voxel techniques.
Water and lipid suppression
The 1H peak from brain water is dominant as well as the resonance from precranial lipids. Since most 1H signals from brain metabolite are present at concentrations less than 10 mM, water and lipid suppression techniques are essential in 1HMRS. Water suppression can be done using Gaussian chemical shift selective pulses (CHESS). The water signal is pre-saturated by using frequency selective 90° pulses. Outer volume selective pulses may be applied to pre-saturate the lipid resenance. However, by using localization technique such as PRESS and STEAM lipid areas can be kept outside the VOI.
Sensitivity
The analytical limit is around 1 mM. MRS is thus not a very sensitive technique. However, many of the 100% naturally abundant 31P and 1H metabolites are present in cellular concentrations in the mM range. In localized in vivo spectroscopy, theoretical minimum resolution is around 1 ml for 1H and 15 ml for 31P. Generally, volumes for brain 1H MRS vary from 4 - 30 ml at 1.5T and typically used VOI is around 8 ml. Resolution can be improved at longer aquisition times and with increasing magnetic field strength. Several factors can influence the sensitivity during an MR examination. For example, the presence of paramagnetic species, or the slow exchange between bound and unbound forms of molecules, can cause signalbroadening. Changes in viscosity, inhomogeneity of magnetic field and many exchamge processes could also affect the line shape of a resonance.
However, despite this relative insensitivity, no other method can do today what MRS can.
Field strength
Most clinical MRS is performed at 1.5T to this date. Higher field strength permits better resolution of overlapping peaks. Field strengths of 3 and 4 T for clinical research have been available for a few years. Today, in vivo magnets of 9 T for experimental research are commercially available. A comparison illustrating improvment in resolution with increased magnetic field strength is shown in figure 4 (a, b).
Spectral quantitation
38 For calculation of in vivo metabolite concentrations it is important to apply quantitaion methods using internal and/or external standards. Absolute quantitation is possible but remains difficult. Relative concentrations and areas of peak ratios are also useful and widely used.
Problems associated with spectral quantitation
Common technical problems encountered arise from: motion artifacts magnetic susceptibility effects partial volume effects
Motion artifacts may arise from breathing or any other movement. Susceptibilty effects may arise from the variety of adjacent tissue to the VOI complicating shimming and affecting field homogeneity. Partial volume effects are caused by the region surrounding the VOI affecting adequate metabolite quantitation. This is particularily problematic when large volumes (> 8 ml) are selected. Smaller VOI can can chosen at the cost of lower signal/noise ratio. Higher magnetic field might solve this problem.
Additionally, general factors like lower field strength, poor shimming and the low concentration of a particular metabolite may complicate calculation of peak areas due to, non-Lorentzian lineshapes, base line distortions and resonance overlap.
Metabolic information
1. 31P MRS
A representative 31PMRS spectrum of the human brain at 1.5T is shown in figure 5a. where peaks of major metabolites observed are assigned. The peaks of , and -ATP, and of PCr and Pi can be clearly identified. Phosphomonoesters such as phosphocholine, phosphoethanolamine and sugar phosphates are under normal conditions are also present on both sides of the Pi resonance and might partly overlap the Pi peak at lower fields.
The -ATP peak is the most reliable in analyzing ATP concentrations, while the a and g resonances contain contributions from NAD and ADP respectively.
Free Cytoplasmic ATP can be calculated from the creatine kinase reaction
PCr2- + ADP- + H+ <----> ATP2- + Cr assumed to be at equilibrium:
Keq = [ATP][Cr]/[H+][ATP][PCr]
The intracellular pH is calculated from chemical shift of Pi relative to Pcr according to the formula where d is the chemical shift: pH= 6.75 + log [( -3.27)/(5.69- )]
2. 1H MRS
39 Figure 5b shows a representative 1H MRS spectrum of the human brain aquired at 1.5T with major observable peaks are assigned.
1H MRS detects a number of metabolites present in relatively low concentrations (< 10 mM), when water and fat suppression techniques are used. Major 1H metabolites observed are commented below:
N-acetyl -aspartate (NAA) produces a large resonance in a H2O suppressed 1H spectrum. The peak may contain up to 20% contributions from Aspartyl-glutamate (NAAG). NAA is generally associated with neurons and axons in the adult brain. It has received considerable interest in several disorders where there is neuron loss. However, its function is largely unknown.
The creatine (Cr), resonance originates from intracellular Cr and PCr these are involved in the creatine kinase reaction and consequently in energy metabolism.
The Choline (Cho) peak arises from a mixture of glycero-phosphoethanolamine and glycero- phosphocholine. Both phospholipids are present in cellular membranes. This resonance can provide information about cell density and membrane integrity (or peroxidation).
A glutamate and glutamine (Glu, Gln) peak can be detected in the human brain. Glutamine is a precursor of glutamate. Glutamate is involved in neurotransmission. Gamma-aminobutyric acid (GABA), also present but in lower concentrations during normal physiological conitions may overlap with the Glu, Gln resonance at 1.5T field strength.
Myo-Inositol (MI) provides a relatively large resonance and is involved in osmotic regulation across the cellular membrane and could be specific for glial cells. The amino acid glycine may also contribute to the myo-inositol resonance. Scyllo-inositol, an isomer of inositol appears also as a singlet peak more downfield. Taurine resonates close to the scyllo-inositol region.
Glucose, an important substrate in brain metabolism gives rise a week but observable coupled resonance. It is more easily detected under hyperglycemic conditions. Lactate can be detected as a boublet resonance in brain tissue. Under normal conditions, lactate is present at around 1 mM concentration and is increased during ischemic conditions as a result of anaerobic glycolysis leading to a more distinct peak.
The brain tissue is rich in lipids. These might be detected as broad resonances with contributions from several fatty acyl chains. Measurement of lipids may be useful in evaluating myelination and membrane breakdown.
The dominant 1H and 31P biochemicals in the human brain are also listed in tables 1 and 2 respectively. Resonance frequencies are given in ppm. The concentrations and ratios are mean values from the literature and are rather orientational than absolute.
MRS and bioenergetics
High energy phosphates such as ATP and Pcr are markers of cellular ability to perform chemical and mechanical work. The PCr /Pi is a direct thermodynamic measure of mitochondrial oxidative phosphorylation.
Extensive experimental studies duing the past 15 years have confirmed the high value of 31P MRS in the understanding of cellular bioenegetics. Numerous studies have used the bioenergetic behaviour as a
40 marker in monitoring disease development and drug effect. Figure 6 illustrates this. The series of spectra show on one hand the behaviour of phosphorous metabolites in an experimental skeletal muscle ischemia and reperfusion model; and on the other hand, the effect of treatment with ascorbate, a potent antioxidant, on the recovery of high energy phosphates during post ischemic reperfusion.
In clinical applications, 31P MRS has been useful for diagnosis and therapy follow-up of metabolic myophapthies. Calculation of the intracllular pH and PCr degradation and resynthesis during muscle exercise and recovery from exercise in patients with muscular and metabolic diseases according to suitable potocoles has been used successfully.
31PMRS have been helpful in studying metabolic diseases of mitochondrial origin where changes in lactate and PCr/Pi are taken as markers like in KearnsSayre syndrome.
Aerobic oxidation of glucose provides the human brain cells with energy. 31P MRS can register of metabolic changes during brain hypoxia where a reduction in oxygen and substrate supply leads to energetic failure and consequently to neuronal dysfunction and membrane breakdown. Thus loss in Pcr and ATP can be dected as well as decreases in intracellular pH. Possible structural membrane changes can be demonstrated from changes in PDE and PME. Intracellular pH and/or lactate are useful markers of low oxygen availability in the cell. It is well that anaerobic metabolism leads to lactate accumulation and in the brain tissue the resulting acidocis might in turn lead to neuronal damage.
Metabolic encephalomyopathies
Brain ischemia and hyoxic/ischemic disease in newborns where cerebral energetics can be monitored to study oxidative and glycolytic metabolism where parameters like pH, Pi/ATP has proven to be good markers. Anaerobic glycolysis in brain is an indication of impairment in mitochondrial function. Decreased PCr/Pi and elevated lactate levels are indications that could help the diagnosis of that metabolic disorders. In cases of hepatic encephalomyopathy, Kearns-Syre syndrome and pyrovate dehydrogenase deficiency, MRS is used to monitor therapy.
Brain trauma
Posttraumatic brain injuries might affect cerebral energy metabolism. Decreases in ATP and in intracellular pH were shown by 31PMRS. Elevated lactate probably due to increased anaerobic glycolysis and diminished NAA were also reported from 1HMRS examinations. In neonateswith acute brain injury 1HMRS examination was able to predict outcome through variations in NAA, Glu/Gln and lactate as illustrated in figure 7.
Stroke
Stroke is associated with degradation of high-energy phosphates (ATP, Pcr) ans increase in inorganic phosphate (Pi) and intracellular acidocis as documented from early 31P MRS insvestigations. Additionally, Typical 1H MRS of patients with stroke show levated lactate and reduced NAA. Follow-up after the acute infarction period might reveal continued loss in NAA as well as acidocis in the ischemic regions of the brain. These parameters are certainly useful in monitoring the affect of medication.
Alzheimer Disease
41 1H MRS using short TE STEAM revealed that myo-inositol is increased in AD. NAA is also decreased in the brain indicating diminished number of healthy neurons. Figure 8 illustrates abnormalities in 1H MRS spectum in a patient with AD.
AIDS
Neurologic disorders such as AIDS-encephalitis and AIDS -dementia resulting from HIV infection have been successfully studied by MRS. Reductions in NAA and increases in Cho have been detected.
Brain tumor
MRS can distinguish between recurrent tumor and tissue necrosis. Adequate tumor diagnosis and therapy monitoring during the various stages of a tumorous disease are important for optimal treatment. Both 31P and 1H MRS have been utilized for diagnosis and therapy monitoring of brain tumors. NAA is decreased in brain gliomas. Studying changes in tumor-type dependent metabolites is an area of active research. Lipids and lactate peaks corelate well with necrotic tumor. High-energy phosphate and phospholipid (ATP, PCr, PDE, PME) levels vary in reponse to radiation therapy, chemotherapy and even to nutrition (in experimental cancer).
This suggests to utility of 31PMRS in tumor therapy monitoring focusing on cellular bioenergetics and phospholipid metabolism.
However, biochemical heterogeneity within the tumor tissue is still difficult to study because of poor resolution on commonly available clinical equipment (1.5T). Brain tumor classification though network analysis and and pattern recognition might shed further light on the different tumor types and degree of activity.
Multiple Sclerosis
Changes in NAA, cho and lactate correlate with axonal damages, demyelination and inflammation observed in MS patients during various stages of the disease. These metabolites can be monitored to the study the outcome of new treatment.
Epilepsy
31P MRS showed that the PCr/Pi is dramatically decreased during seizures and normalized after seizure discharge. The glutamine and glutamate peak is elevated in the hippcampus while NAA is diminshed in patients with chronic epilepsy . Changes in GABA have been correlated with drugs affecting GABA metabolism. An increase in lactate has also been reported in focal epilepsy of extratemporal origin.
These biochemical changes in epiteptogenic region of the brain indicate that 1HMRS can be clinically useful in the diagnosis of this disease as a complement to MRI.
Schizophrenia
31P spectroscopy studies revealed increases in PDE and decreases inPME in the prefrontal cortex of
42 schizophrenics. Alterations in these lipids vary with different brain regions and stages of the disease. Reductions in NAA and glutamate have been reported from 1H spectroscopy investigations. These reductions were largely found in the hypocampal area/mesial temporal lobe
Additional neurological diseases under evaluation include:
Huntington disease
Increases in lactate and in Pi and decreases in PCr in Huntington disease implicate mitochondrial oxidative phosphorylation in the disease process.
Migraine
31P studies showed diminished PCr and increased Pi and ADP which indicates energetic disturbances in brain tissue in patients with migraine.
Parkinson Disease
A decrrease in the neuronal marker NAA and an increase lactate/NAA ratio were reported by 1HMRS.
Psychiatry (mood disorders)
Both 31P and 1HMRS have been used in investigation mood disorders where changes in energy metabolism , lipids and Cho were observed. This indicates the potential of MRS in monitoring the effect of psychopharmacological drugs.
CONCLUSIONS
MRS is a unique and powerful technique that has been applied to a number of brain diseases. It can be correlated with imaging and other clinical data for confirmation. It is useful in diagnosis and prognosis of disease and mostly in the evaluation of the noninvasive monitoring of response to treatment.
Metabolic information from MR spectra is an emerging component in modern neurochemistry.
In neuroresearch MRS is definitely a revolutionary tool that will help understand the brain biochemistry of mechanisms of disease. MRS if introduced into a clinical practice could be very supportive in clinical decision making.
Spectral quantification is still difficult therefore relative concentrations of metabolites are usually calculated.
Most reports are difficult to compare due variations various parameters in the methodological set up. Additional complicating factors are the diversity in clinical material studied and exact anatomical localization (including gray-white matter separation). Discrepancies in results can thus be expected .
In vivo MRS is a complex technology that requires the simultaneous optimal adjustment of multiple parameters during an examination.The most critical task in MRS however, is not spectral aquisition but rather spectral analysis . This latter is time demanding and necessitates appropriate know-how in order to interprete the results, eliminate arifacts and quantitate data often by complex procedures and finally statistically analyze the findings.
43 The precise role of many identified metabolites is still unclear. Therefore, along with experimental mechanistic research, incorporation of MRS in clinical practice as much as possible would increase the body of information since what is still needed is the characterization of spectral patterns in disease conditions and in healthy control conditions.
Major benefits
High chemical specificity in studying: energy metabolism, lipid metabolism, amino acid and intermediary metabolism, noninvasive regional serial measurements of metabolite in patients and controls subjects. Therapy response. Mechanistic studies of inherited and acquired brain metabolic diseases.
Generally, MRS is well suited for the exploration of diffuse brain diseases where it provides new insights.
Technical improvements
Major technical improvments by manufacturers in terms of hardware and user friendly software has contributed largely to the increase in the number of clinical studies using 1HMRS along with conventional MRI.
Automation of methods for shimming, water suppression and peak integration will replace the manual adjustment of several parameters thus increase reproducibility and certainly spread the use of this technique.
FUTURE STUDIES
Future studies should focus on multidisciplinary multicentre projects for the development of standardized reproducible measurements e.g. : Instrumental calibration protocoles (internal/extern standards) Protocoles for quality assessment Comparison of methodologies used for data aquisition, analysis and metabolite quantitation betwen different centres
Collaborative efforts are necessary for the evaluation of the value of MRS in diagnosis, prognosis and therapy monitoring in order to enhance clinical workability.
Future technological improvements in magnetic field strength, gradients, data processing and analysis will also encourage more applications of 13C and 19F.
And last, envision in vivo non-invasive access to highly localized and reliable chemical information as a routine clinical procedure in health and in disease... Life would become much easier for both patient and clinician. Until then MRS continues to be an area of intensive investigation.
44 REFERENCES and suggestions for further reading:
Clinical MRS reviews
1. Novotny E, Ashwal S, Shevell M. Proton magnetic resonance spectroscopy: an emerging technology in pediatric neurology research. Pediatr Res 44 (1): 1-10, 1998.
2. Rudkin TM, Arnold DL. Proton magnetic resonance spectroscopy for the diagnosis and management of cerebral disorders. Arch Neurol 56 (8): 919-26, 1999.
3. Vion-Dury J, Meyerhoff DJ, Cozzone PJ, Weiner MW. What might be the impact on neurology of the analysis of brain metabolism by in vivo magnetic resonance spectroscopy? [editorial]. J Neurol 241 (6): 354-71, 1994.
4. Iles RA, Burns SP. In vitro NMR spectroscopy in the diagnosis and investigation of metabolic disorders. Quart. Magn. Res. in Biol. Med. 2 (1): 35-42, 1995.
5. Radda GK. The use of NMR spectroscopy for the understanding of disease. Science 233 (4764): 640-5, 1986.
6. Gruetter R, Weisdorf SA, Rajanayagan V, Terpstra M, Merkle H, Truwit CL, Garwood M, Nyberg SL, Ugurbil K. Resolution improvements in in vivo 1H NMR spectra with increased magnetic field strength. J Magn Reson 135 (1): 260-4, 1998.
MR Principles
7. Andrew ER. An introduction to nuclear magnetic resonance in biomedicine. Can Assoc Radiol J 41 (1): 2-7, 1990.
8. Hoffenberg EF, Kozlowski P, Salerno TA, Deslauriers R. Evaluation of cardiac 31P magnetic resonance spectroscopy: reviewing NMR principles. J Surg Res 62 (1): 135-43, 1996.
9. Woodward P. MRI for technologists. McGraw-Hill, p. 432, 2000
10. Mitchell DG. MRI Principles. Saunders company LTD, W B, p. 288, 1998.
11. Longmore DB. The principles of magnetic resonance. Br Med Bull 45 (4): 848-80, 1989.
12. Wehrli WF, Shaw D, Kneeland JB. Biomedical magnetic resonance imaging. New York: VCH Publisher, p. 601, 1988.
Gadian DG. Nuclear Magnetic Resonance and its application to living systems.Oxford: Clarendon Press, 1982
Slichter CP. Principles of Magnetic resonance Spectroscopy. Second edition, Berlin: Springer- Verlag. 1978.
45
Farrar TC & Becker ED.Pulse and Fourier Transform NMR.New York: Academic Press, 1971.
Experimental applications
13. Bollano E, Omerovic E, Bohlooly M, Kujacic V, Madhu B, Tornell J, Isaksson O, Soussi B, Schulze W, Fu ML, Matejka G, Waagstein F, Isgaard J. Impairment of cardiac function and bioenergetics in adult transgenic mice overexpressing the bovine growth hormone gene. Endocrinology 141 (6): 2229-35, 2000.
14. Lagerwall K, Daneryd P, Schersten T, Soussi B. In vivo 31P nuclear magnetic resonance evidence of the salvage effect of ascorbate on the postischemic reperfused rat skeletal muscle. Life Sci 56 (6): 389-97, 1995.
15. Lagerwall K, Madhu B, Daneryd P, Schersten T, Soussi B. Purine nucleotides and phospholipids in ischemic and reperfused rat skeletal muscle: effect of ascorbate. Am J Physiol 272 (1 Pt 2): H83-90, 1997.
16. Lukes D, Madhu B, Arvidsson N, Gustavsson M, Mjornstedt L, Soussi B, Olausson M. In vivo 31P MRS evaluation of the rejection process and differences in anesthetic procedures in a concordant xenotransplantation: mouse heart to rat modell. Transplant Proc 29 (7): 3159-60, 1997.
17. Madhu B, Lagerwall K, Soussi B. Phosphorus metabolites in different muscles of the rat leg by 31P image- selected in vivo spectroscopy [published erratum appears in NMR Biomed 1997 Sep;10(6):302]. NMR Biomed 9 (8): 327-32, 1996.
18. Omerovic E, Basetti M, Bollano E, Bohlooly M, Tornell J, Isgaard J, Hjalmarson A, Soussi B, Waagstein F. In vivo metabolic imaging of cardiac bioenergetics in transgenic mice. Biochem Biophys Res Commun 271 (1): 222-8, 2000.
19. Omerovic E, Bollano E, Basetti M, Kujacic V, Waagstein L, Hjalmarson A, Waagstein F, Soussi B. Bioenergetic, functional and morphological consequences of postinfarct cardiac remodeling in the rat. J Mol Cell Cardiol 31 (9): 1685-95, 1999.
20. Sorensen V, Jonsson O, Pettersson S, Schersten T, Soussi B. In vivo 31P NMR OSIRIS of bioenergetic changes in rabbit kidneys during and after ischaemia: effect of pretreatment with an indeno-indole compound. Acta Physiol Scand 162 (4): 495-500, 1998.
21. Soussi B, Idstrom JP, Bylund-Fellenius AC, Schersten T. Dynamics of skeletal muscle energetics during ischemia and reperfusion assessed by in vivo 31P NMR. NMR Biomed 3 (2): 71-7, 1990.
22. Soussi B, Lagerwall K, Idstrom JP, Schersten T. Purine metabolic pathways in rat hindlimb perfusion model during ischemia and reperfusion. Am J Physiol 265 (4 Pt 2): H1074-81, 1993.
23. Hajek M, Burian M, Dezortova M. Application of LCModel for quality control and quantitative in vivo 1H MR spectroscopy by short echo time STEAM sequence. Magma 10 (1): 6-17, 2000.
24. Podo F, Henriksen O, Bovee WM, Leach MO, Leibfritz D, de Certaines JD. Absolute metabolite quantification by in vivo NMR spectroscopy: I. Introduction, objectives and activities of a
46 concerted action in biomedical research. Magn Reson Imaging 16 (9): 1085-92, 1998.
25. Chen W, Adriany G, Zhu XH, Gruetter R, Ugurbil K. Detecting natural abundance carbon signal of NAA metabolite within 12- cm3 localized volume of human brain using 1H-[13C] NMR spectroscopy. Magn Reson Med 40 (2): 180-4, 1998.
Epilepsy
26. Duc CO, Trabesinger AH, Weber OM, Meier D, Walder M, Wieser HG, Boesiger P. Quantitative 1H MRS in the evaluation of mesial temporal lobe epilepsy in vivo. Magn Reson Imaging 16 (8): 969-79, 1998.
27. Hajek M, Dezortova M, Komarek V. 1H MR spectroscopy in patients with mesial temporal epilepsy. Magma 7 (2): 95-114, 1998.
28. Rothman DL, Behar KL, Prichard JW, Petroff OA. Homocarnosine and the measurement of neuronal pH in patients with epilepsy. Magn Reson Med 38 (6): 924-9, 1997.
29. van der Grond J, Gerson JR, Laxer KD, Hugg JW, Matson GB, Weiner MW. Regional distribution of interictal 31P metabolic changes in patients with temporal lobe epilepsy. Epilepsia 39 (5): 527-36, 1998.
30. Vainio P, Usenius JP, Vapalahti M, Partanen K, Kalviainen R, Rinne J, Kauppinen RA. Reduced N-acetylaspartate concentration in temporal lobe epilepsy by quantitative 1H MRS in vivo. Neuroreport 5 (14): 1733-6, 1994.
Stroke and acute brain injuries
31. Blamire AM, Graham GD, Rothman DL, Prichard JW. Proton spectroscopy of human stroke: assessment of transverse relaxation times and partial volume effects in single volume steam MRS. Magn Reson Imaging 12 (8): 1227-35, 1994.
32. Ford CC, Griffey RH, Matwiyoff NA, Rosenberg GA. Multivoxel 1H-MRS of stroke. Neurology 42 (7): 1408-12, 1992.
33. Friedman SD, Brooks WM, Jung RE, Chiulli SJ, Sloan JH, Montoya BT, Hart BL, Yeo RA. Quantitative proton MRS predicts outcome after traumatic brain injury. Neurology 52 (7): 1384- 91, 1999.
34. Gideon P, Rosenbaum S, Sperling B, Petersen P. MR-visible brain water content in human acute stroke. Magn Reson Imaging 17 (2): 301-4, 1999.
35. Holshouser BA, Ashwal S, Shu S, Hinshaw DB, Jr. Proton MR spectroscopy in children with acute brain injury: comparison of short and long echo time acquisitions. J Magn Reson Imaging 11 (1): 9-19, 2000.
36. Ross BD, Ernst T, Kreis R, Haseler LJ, Bayer S, Danielsen E, Bluml S, Shonk T, Mandigo JC, Caton W, Clark C, Jensen SW, Lehman NL, Arcinue E, Pudenz R, Shelden CH. 1H MRS in acute traumatic brain injury. J Magn Reson Imaging 8 (4): 829-40, 1998.
37. Wardlaw JM, Marshall I, Wild J, Dennis MS, Cannon J, Lewis SC. Studies of acute ischemic
47 stroke with proton magnetic resonance spectroscopy: relation between time from onset, neurological deficit, metabolite abnormalities in the infarct, blood flow, and clinical outcome. Stroke 29 (8): 1618-24, 1998.
Schizophrenia
38. Keshavan MS, Sanders RD, Pettegrew JW, Dombrowsky SM, Panchalingam KS. Frontal lobe metabolism and cerebral morphology in schizophrenia: 31P MRS and MRI studies. Schizophr Res 10 (3): 241-6, 1993.
39. Nasrallah HA, Skinner TE, Schmalbrock P, Robitaille PM. Proton magnetic resonance spectroscopy (1H MRS) of the hippocampal formation in schizophrenia: a pilot study. Br J Psychiatry 165 (4): 481-5, 1994.
40. Riehemann S, Volz HP, Smesny S, Hubner G, Wenda B, Rossger G, Sauer H. Phosphorus 31 magnetic resonance spectroscopy in schizophrenia research. Pathophysiology of cerebral metabolism of high-energy phosphate and membrane phospholipids. Nervenarzt 71 (5): 354-63, 2000.
41. Sigmundsson T. TBK, Maier M., Williams SCR., Simmons A., Greenwood K., Ron MA. Frontal lobe in vivo proton magnetic resonance spectroscopy in schizophrenic patients with negative symptoms. Schizophrenia Research 24 (1-2): 182, 1997.
Cancer
42. Castillo M, Kwock L. Clinical applications of proton magnetic resonance spectroscopy in the evaluation of common intracranial tumors. Top Magn Reson Imaging 10 (2): 104-13, 1999.
43. Kim SH, Chang KH, Song IC, Han MH, Kim HC, Kang HS, Han MC. Brain abscess and brain tumor: discrimination with in vivo H-1 MR spectroscopy [see comments]. Radiology 204 (1): 239-45, 1997.
44. Leach MO. Introduction to in vivo MRS of cancer: new perspectives and open problems. Anticancer Res 16 (3B): 1503-14, 1996.
45. Negendank W, Li CW, Padavic-Shaller K, Murphy-Boesch J, Brown TR. Phospholipid metabolites in 1H-decoupled 31P MRS in vivo in human cancer: implications for experimental models and clinical studies. Anticancer Res 16 (3B): 1539-44, 1996.
46. Sijens PE, Levendag PC, Vecht CJ, van Dijk P, Oudkerk M. 1H MR spectroscopy detection of lipids and lactate in metastatic brain tumors. NMR Biomed 9 (2): 65-71, 1996.
Multiple sclerosis and ALS
47. Arnold DL, Matthews PM, Francis G, Antel J. Proton magnetic resonance spectroscopy of human brain in vivo in the evaluation of multiple sclerosis: assessment of the load of disease. Magn Reson Med 14 (1): 154-9, 1990.
48. Block W, Karitzky J, Traber F, Pohl C, Keller E, Mundegar RR, Lamerichs R, Rink H, Ries F, Schild HH, Jerusalem F. Proton magnetic resonance spectroscopy of the primary motor cortex in
48 patients with motor neuron disease: subgroup analysis and follow-up measurements. Arch Neurol 55 (7): 931-6, 1998.
49. Leary SM, Brex PA, MacManus DG, Parker GJ, Barker GJ, Miller DH, Thompson AJ. A (1)H magnetic resonance spectroscopy study of aging in parietal white matter: implications for trials in multiple sclerosis. Magn Reson Imaging 18 (4): 455-9, 2000.
50. Rooney WD, Miller RG, Gelinas D, Schuff N, Maudsley AA, Weiner MW. Decreased N- acetylaspartate in motor cortex and corticospinal tract in ALS. Neurology 50 (6): 1800-5, 1998.
51. Sarchielli P, Presciutti O, Tarducci R, Gobbi G, Alberti A, Pelliccioli GP, Orlacchio A, Gallai V. 1H-MRS in patients with multiple sclerosis undergoing treatment with interferon beta-1a: results of a preliminary study. J Neurol Neurosurg Psychiatry 64 (2): 204-12, 1998.
Encephalmyopathy and metabolic diseases
52. Soussi B, Schersten T, Waldenstrom A, Ronquist G. Phosphocreatine turnover and pH balance in forearm muscle of patients with syndrome X [letter]. Lancet 341 (8848): 829-30, 1993.
53. Ronquist G, Soussi B, Frithz G, Schersten T, Waldenstrom A. Disturbed energy balance in skeletal muscle of patients with untreated primary hypertension. J Intern Med 238 (2): 167-74, 1995.
54. Kuhl CK, Layer G, Traber F, Zierz S, Block W, Reiser M. Mitochondrial encephalomyopathy: correlation of P-31 exercise MR spectroscopy with clinical findings. Radiology 192 (1): 223-30, 1994.
55. Mathews PM, Andermann F, Silver K, Karpati G, Arnold DL. Proton MR spectroscopic characterization of differences in regional brain metabolic abnormalities in mitochondrial encephalomyopathies. Neurology 43 (12): 2484-90, 1993.
Alzheimer¥s Disease and Dementia
56. Cuenod CA, Kaplan DB, Michot JL, Jehenson P, Leroy-Willig A, Forette F, Syrota A, Boller F. Phospholipid abnormalities in early Alzheimer's disease. In vivo phosphorus 31 magnetic resonance spectroscopy. Arch Neurol 52 (1): 89-94, 1995.
57. Moats RA, Ernst T, Shonk TK, Ross BD. Abnormal cerebral metabolite concentrations in patients with probable Alzheimer disease. Magn Reson Med 32 (1): 110-5, 1994.
58. Ross BD, Bluml S, Cowan R, Danielsen E, Farrow N, Gruetter R. In vivo magnetic resonance spectroscopy of human brain: the biophysical basis of dementia. Biophys Chem 68 (1-3): 161-72, 1997.
59. Schofield PW, Mosesson RE, Stern Y, Mayeux R. The age at onset of Alzheimer's disease and an intracranial area measurement. A relationship. Arch Neurol 52 (1): 95-8, 1995.
60. Schuff N, Amend D, Ezekiel F, Steinman SK, Tanabe J, Norman D, Jagust W, Kramer JH, Mastrianni JA, Fein G, Weiner MW. Changes of hippocampal N-acetyl aspartate and volume in Alzheimer's disease. A proton MR spectroscopic imaging and MRI study. Neurology 49 (6):
49 1513-21, 1997.
Legends to figures and tables
Figure 1. The free induction decay is converted to a spectrum by a Fourier transformation. The FID signal (= amlitude vs time) is converted to a spectrum (= amplitude vs frequency).
Figure 2. Volume selection and spectral acquisition. A: MRI of normal human brain, illustrating the VOI = 50 x 40 x 50 mm. B: Proton MRS spectrum of the selected volume showing the major proton metabolites. (Reproduced from 47)
Figure 3. In vivo 31P MR spectrum localised from rat brain with ISIS ( VOI = 10 x 10 x 10 mm). Mannetic field strength = 2.35 T. The peaks of the adenosine triphosphates a-, b-, and g-ATP, the phosphocreatine, PCr, the inorganic phosphate Pi as well as the phosphomonoesters PME and the phosphodiesters DPE are assigned.
Figure 4. Improved resolution with improved magnetic field strength. a) In vivo 31P MR spectrum of rat skeletal muscle at 2.35T. b) In vitro 31P high resolution NMR spectrum of skeletal muscle extract acquired at 11.74 T. The peaks of the adenosine triphosphates a-, b-, and g-ATP, the phosphocreatine, PCr, the inorganic phosphate Pi are well resolved. Peaks at 6.3-7.3 ppm are PME including G-6-P at 7.17ppm. The large Pi peak arises from artifactual degradation of PCr.
Figure 5. Localized MRS spectra of of normal human brain illustrating the major metabolites observed. (A) is an ISIS 31P MR spectrum obtained at 2 T (VOI = 100 ml). The adenosine triphosphates a-, b-, and g-ATP, the phosphocreatine, PCr, the inorganic phosphate Pi as well as the phosphomonoesters PME and the phosphodiesters DPE are well resolved. (B) is a proton MR spectrum at 1.5 T obtained with STEAM combined with CHESS to suppress the water signal, (VOI = 8 ml). The assigned proton metabolites are: N-acetylaspartate NAA, glutamate and glutamine GLU-GLN, creatine and phosphocreatine Cr-PCr, choline CHO, inositol INS scyllo-inosito Scy-INS, taurine TAU, glycine GLY and glucose. (Reproduced from 3)
Figure 6. Illustration of the dynamics of cellular energetics by in vivo 31PMRS The potential of MRS in therapy monitoring is also demontrated. The spectra are from a skeletal muscle from a control rat and a rat treated with ascorbate. At rest (A), after 2 h of ischemia (B), after 4 h if ischemia (C) and after 4 h of ischemia + 150 minutes of reperfusion (D). The treated rat showed higher levels of PCr and ATP after reperfusion. Spectra were obtained by accumulating 128 FIDs with a repetition time 1 s at 2.35 T. (Reproduced from 13)
50 Figure 7. 1H MRS illustrating patterns seen in STEAM spectra (a, c) and in PRESS spectra (b, d) from the brain of two children with after birth brain injury. Spectra (a, b) are from a patient with a mild brain injury and show good outcome. Spectra (c, d) are from a patient with a traumatic brain injury and show poor outcome (Note the low NAA signal and the elevated lactate signal).
Figure 8. A proton MRS spectrum from the brain of a normal patient (A) compared with a spectrum of a patient with Alzheimer disease (B). (Reproduced from 58)
Table 1. Major proton metabolites with approximate mean concentrations and corresponding resonance frequencies detected in normal human brain by in vivo MRS.
Table 2. Summary of 31P metabolites in normal human brain obtained by in vivo MRS. Relative mean metabolite ratios are also given.
51 Chapter IV – J.L. Stievenart
Basic principles of Nuclear Medicine in Neurosciences
Jean-Louis STIEVENART, Praticien Hospitalier, Service de Médecine Nucléaire, C.H.U. Hôpital Beaujon, Clichy, France
The aim of this presentation is to draw a broad overview of the functional brain imaging in Nuclear
Medicine. A more in depth description of these techniques and of their applications can be found in a recent reference (1).
All these methods have in common two fundamental steps :
- injection of radioactive substance to a patient at some time during which the status of the brain
activity is known (« basal », seizure free, drug action, etc….) ;
- Tomographic imaging of the radioactive distribution after a delay that is important to monitor.
The radioactive substance is a radiopharmaceutical which has two components : a molecule of biologic interest and a radioactive atom tightly bound to it.
Thus, questions to deal with to get a better understanding of these examinations become self-evident :
What are the available radiopharmaceuticals, and which aspects of brain functions do they allow to explore ?
How can we make an image of a radioactive distribution and what are the spatial and temporal resolutions of the instruments ?
In which clinical situations do these methods give relevant and irreplaceable information ?
The radiopharmaceuticals.
1 the radioactive atoms.
They have an unstable nucleus which spontaneously emits energy to reach a stable state. This transformation is inexorable and its rate is characterized by the half-life, that is the time period during
52 which half of the atoms of a sample have experienced it. The number of these transformations occurring in one second is the activity of the sample (unit of activity : 1 Becquerel (Bq) = 1 decay per second ; equivalence with an older unit the Curie 1 mCi = 37 MBq ).
As far as we are concerned, they fall into two categories :
- the gamma emitters for which the transformation is associated with the emission of a photon of a
precise energy.
- The beta-plus emitters for which the transformation is associated with the emission of a positive
electron or positron of variable energy. Secondary, these positrons will slow down and collide with
electrons of the medium. This event takes place after a travel of about 2 mm. depending on the initial
energy of the positron ( the mean of this travel distance is called the range). A dematerialisation
occurs and the mass of the electron and of the positron transform in energy resulting in an emission of
two photons in two opposite directions, each one with the precise energy of 511 kiloelectron-volts
(keV). Figure 1.
The gamma-emitters are used to perform single photon computed emission tomography (SPECT), the main representative of this class are the technetium 99m (99mTc half-life 6 hours, energy 140 keV), and the iodine 123 (123I, half-life 13 hours, energy 159 keV. In spite of its relatively short half-life 99mTc is the most easily used radionuclide, being available from a 99Mo/99mTc generator. The beta plus emitters are the core of the positron emission tomography (PET). Fluor 18 (18F, half-life 110 minutes) plays a major role in
PET examinations. Other atoms can be used : oxygen 15 (15O half-life 2 minutes), carbon 11 (11C half-life
20 minutes), 13 nitrogen (13N half-life 10 minutes). They can be easily included in molecules of biological interest but their short half-lives require their on site production (cyclotron) and coupling with the other parts of the molecule.
2 the molecules of biological interest.
2.1 perfusion and energetic metabolism
53 Hexa-methyl-propylenamine-oxime-99mTc (HMPAO, Ceretec®) and Ethyl-cysteinate-dimer-99mTc
(ECD, Neurolite®) are the radiopharmaceuticals with which SPECT perfusion brain studies are routinely performed. They are lipophilic molecules that easily go through the blood brain barrier and cellular membranes. Then they become hydrophilic in the cells (neurons and astrocytes) and thus unable to go backward across lipids layers. The involved chemical transformations are for the HMPAO a reaction with glutathione (2) and for the ECD an esterification catalyzed by a primate specific enzyme (3). So, the radioactivity is rapidely trapped in the brain cells, proportionally in first approximation, to the local blood flow. Because of this behavior these molecules are sometimes referred to as « chemical microspheres ».
2-Fluoro-2-deoxy-D-glucose (18FDG ) has been used for more than 20 years as a metabolic tracer of cells functioning. This substance diffuses through the cell membrane, this diffusion being facilitated by glucose transporters. It then undergoes a phosphorylation step by hexokinase and cannot follow further the glucose metabolic pathway. Thus the trapped activity by cells reflects their glucose consumption
201Tl-chloride and 99mTc-metoxyisobitytilisonitrilme (MIBI) are radiopharmaceutical designed to study cardiac perfusion and they reflect another aspect of cell functioning. The Tl+ ion is analogous to K+ and is actively transported across membrane by Na+/K+-ATPase. SestaMIBI (Cardiolite®) has an uptake dependant upon membrane electrical potential and accumulates in mitochondria.
2.2 The dopaminergic pathways.
Since the beginnings of the PET this pathway (figure 2) has received a considerable attention due to its implications in psychiatric symptoms and movements disorders (4). 18F –fluoro-DOPA was used to assess the activity of dopaminergic neurons. The presynaptic components of the synapse have also been studied with ligands for dopamine transporters (DAT) which are tropane derivatives. They were at first labeled with 11C as the [11C]CFT (5). Now, 123I labeled agents are commercially available such as 123I -CIT (6) and
123IFP- -CIT (Ioflupane, DatScan®) (7). Work is in progress to develop 99mTc labeled ligands that would be more convenient for routine clinical use (8). One of them, the 99mTc-TRODAT is already in a Phase I clinical study (9). Numerous ligands for D2 and D3 receptors have been developed, most of them
54 belonging to the benzamides family. The 11C-raclopride has been the first of them (10). More recently this kind of molecules has been labeled with 18F, which is a more appropriate radionuclide for performing kinetic studies, such as fluoropropylbenzamide (11) and with 123I, such as 123I iodobenzamide (IBZM) (12) which opens the possibility to study D2 and D3 dopamine receptors with SPECT.
2.3 other receptors ligands
The benzodiazepine receptors
The central benzodiazepine site is a part of the gamma-aminobutyric acid (GABA) channel receptor –
11 (GABA)A. This site has been thoroughly studied by PET with Cflumazenil (13,14). The equivalent
SPECT radiopharmaceutical is 123Iiomazenil and efforts are currently done to reach a PET-like accuracy for estimation of binding parameters of this tracer (15,16).
Many other ligands have been designed for PET imaging of the serotonine system (17-19), the cholinergic system (20). SPECT tracers are less numerous. Up to now, none of them is available for clinical routine.
2.4 Labeled amino acids
Proteins synthesis is an aspect other than the glucose metabolism by which malignant lesions may be distinguished from the benign ones. Among the different synthesized labeled amino acids the 11C
MethylMethionine (CMET) has had a relatively wide usage. [18F] fluoro- -metyl-tyrosine has also been tried as a tumor marker (21). The SPECT version of this agent, 123I iodo- -methyl-tyrosine is currently under tests (22).
2.5 molecules kinetics modeling.
If the labeled molecules were completely extracted from circulation during the first pass of blood in brain tissue and irreversibly trapped there, the radioactivity distribution would be an image of the local blood flows. Even for the so-called chemical microsphere it is not exactly the case. For neuroreceptors or transporters studies, such a weighting by perfusion conditions would rather be a confounding factor, the parameter of interest being the availability of specific sites for a given ligand. Making the distinction
55 between the delivery and the binding of a molecule and separately measuring both, are the main tasks assigned to tracer kinetic modeling (23). It is usually assumed that the labeled ligand participates to exchanges between several compartments, and that the tissue in which the activity is measured can be modelized as a sum of these exchanging compartments. A sequence of acquisitions is done to give the time course of activity in every voxel of interest. This evolution is compared to other ones in plasma or in some reference organ or region. Fitting to the expected evolutions derived from the model can give access to its parameters. But it must be underlined that with a single injection it is not always possible to estimate all the parameters. For this purpose more sophisticated protocols are needed, such as coinjection of cold ligand or continuous infusion (24).
To present some definitions and techniques let us consider the one-tissue model (figure 3).
Cp(t) is the plasma tracer concentration (activity) at time t (units: kBq.ml-1)
C(t) is the local tracer concentration in brain tissue (kBq.ml-1)
K1 is the rate constant for transfer from plasma to the tissue across the blood brain barrier
-1 -1 (ml(plasma).min .ml (brain))
-1 k2 is the rate constant for transfer from tissue to plasma (min )
The evolutions of radioactive concentrations is ruled by the differential equation: dC(t)/dt = K1.Cp(t) – k2.C(t) (1)
If the system is in a steady-state dC(t)/dt = 0 and K1.Cp(t) = k2.C(t)
Then C(t)/Cp(t) = K1/k2 = cst.
-1 Considering the units of K1 and k2 this ratio is expressed in ml(plasma).ml (brain).
It represents the volume the radioligand would occupy if it were in the brain at the same concentration as in the plasma. It defines the volume of distribution of the radioligand which reflects the binding potential of the brain tissue. To illustrate how these parameters can be estimated let us integrate the equation
[1]
t t C t K . Cp u du k . C(u)du 1 2 0 0
56 Division of both sides of this equation by C(t) and k2 followed by some rearrangements yields t t Cudu Cpudu K 1 0 1 . 0 Ct k 2 Ct k 2
This relation is the basis of Logan’s graphical analysis (25). One disposes of two sets of measurements
Cp(ti) (from blood sampling), C(ti) ( from PET or SPECT acquisitions). Two series of values (expressed in min.)
ti ti Cudu Cpudu 0 , 0 Ct i Ct i can thus be calculated. If the model is valid, the points defined by these couples of values are aligned along a straight line, the slope of which is the distribution volume of the radioligand. Its ordinate at origin is an estimation of 1/k2. Usually, adjunction of a second tissue compartment (the receptor rich compartment), introducing two new rate constants k3 and k4 is needed to improve the fit to the experimental data.
The instrumentation
1 detection of photons.
In both modalities photons have to be detected. This is done by use of scintillating crystal, converting the energy of an incident photon in light photons. These light photons, the number of which depends on incident photon energy, are multiplied by a photomultiplier, detected and, if the energy has a suitable value, the scintillation origin is determined. The main difference between SPECT and PET is that in
SPECT, a single photon does not bear information about its direction when it hits the crystal. Whereas, in
PET, two photons are to be detected simultaneously (or near simultaneously) and thus it is known that the annihilation point is on the line joining the two detected points.
57 2 The gamma camera. the collimator selects photons before they hit the sodium iodide (NaI) crystal. It may be designed with parallel channels or with converging channels in the transverse plane and parallels in the axial ones, resulting in a “fan-beam” geometry (26). Detector and collimator are grouped in a head that orbits around the patient. Most cameras have now 2 or 3 heads arranged for example as shown on figure 4. Only photons travelling accordingly to the direction of collimator channels are detectable. Among those ones, some are scattered and others are absorbed by the patient tissues.
3 the PET scanner.
The collimator is no longer necessary. Yet selecting devices are sometimes used to perform 2D imaging where coincidences are looked for in slices. Due to higher energy of incident photons more dense crystals are used. Critical parameters of these crystals are their energy resolution and the duration of the scintillation after one hit, the shorter being the better in order to get a sharp time resolution to detect true coincidences. Gadolinium oxyorthosilicate (GSO) and lutetium oxyorthosilicate (LSO) are recently developed scintillators for which these parameters are well suited. The coincidences are detected inside a temporal “coincidence window” the length of which is of the order of 8 nanoseconds. Potentially, all the annihilations occurring in the object and emitting in the solid angle encompassed by the camera could be detected. But some phenomena adversely affect this sensitivity: random coincidences causing non existent events to be detected, scatter causing to misposition true events, attenuation in the patient preventing one or two photons of the pair to reach the detector.
Nowadays, PET scanner is frequently coupled to a high quality X-rays scanner. So attenuation correction is simplified and functional and morphologic data can easily be merged.
4 imaging capabilities
What the camera yield is a set of projections of a radioactive distribution. It is the task of the reconstruction algorithm to go back to this volumic distribution (inverse problem). For years, this step was quasi exclusively based on the filtred backprojection algorithm (preceded by a rebinning (rearrangement of projections) in case of fan beam collimator or 3D acquisition). In this method a low pass filter is
58 involved, the properties of which are important to know to achieve an adequate balance between resolution and noise. Recently, iterative methods gains a more widespread usage. They include a more realistic modeling of the acquisition process and rely on the principle of maximum-likelihood expectation maximization (MLEM). That is to say they try to compute the distribution, the acquired projection of which are the most likely the observed ones. This method is implemented for PET and SPECT with a procedure to accelerate its convergence: ordered-subset expectation maximization (OSEM) (27). For direct reconstruction of 3D PET acquisitions an analogous algorithm can be used: row action maximization likelihood (RAMLA) (28).
An important issue is the attenuation correction which can be relatively exact in PET but more problematic in SPECT where the Chang’s method (29) is the most popular.
With 30 min. acquisitions the resolution (axial and transversal FWHM) is about 9 mm. for SPECT and 4-
5 mm. for PET.
For an in depth review of characteristics of current PET systems see reference (30).
When the best temporal and spatial resolutions are researched one must use dedicated brain camera. This is the case for quantitative molecular kinetics studies. In the majority of the described applications this is not mandatory and the tomoscintigraphies can be performed with general purpose systems equipped with an adequate head-holder.
The clinical applications
1 cerebrovascular diseases
In this domain a lot of work was done with PET tracers not detailed in the radiopharmaceutical section as
15 15 15 H2 O, , C O, O2 , which allowed to study and measure perfusion (cerebral blood flow: CBF), blood volume (CBV), oxygen consumption (CMRO2) etc…. It was an extensive research field. Concerning the blood flow, many studies (31,32) reported quantitative approach to measure it in ml.min -1.100g-1 with
59 HMPAO or ECD but no universally accepted quantification method, usable in clinical routine, emerged up to now
Let us simply recall the main results (33-35). Glucose consumption (CMRGlu) and local blood flow are coupled in most of the clinical situations (36), (there may be exception during coma, anesthesia or in post- ictal periods). Face to a decline of perfusion pressure, the first compensating mechanism is an augmentation of local blood volume. When its maximum is reached (autoregulation threshold) the CBF begins to decrease but, due to the second compensation mechanism, the augmentation of the Oxygen extraction fraction (OEF), the CMRO2 is maintained. This phase corresponds to the misery perfusion.
Then the brain tissue enters the true ischemic zone, experiencing first a reversible dysfunction (the penumbra) then an irreversible one (37). The situation of maximum local vasodilatation was termed
« oligemia » by Lassen and is a potentially dangerous one. To recognize it, in complex vascular malformation for example, a pharmacological trial with Acetazolamide
(Diamox®) is proposed. Oligemic regions look like normal in basal examination and like hypoperfused in the examination after Acetazolamide (38). In some circumstances the Acetazolamide reactivity may be normal in a brain territory having a low baseline perfusion. This occurs in patients with occlusive carotid artery diseases and is the sign of a blood supply adapted to a low demand. It suggest possible incomplete infarction (not visible in MRI). This hypothesis is reinforced by a diminution of benzodiazepine receptors ligands binding in these regions (39). This situation is not predictive of a subsequent ischemic stroke.
When an ischemic or already damaged brain tissue is reperfused a luxury perfusion may occur, characterized by a reduction of OEF (40) and thus an oxygen supply in excess of demand. It is considered that this period, if associated with an increased cerebral blood flow, can be visualized by HMPAO, but not by ECD. However this hyperfixation of HMPAO is equivocal and may be due an altered blood-brain barrier (41)
Perfusion SPECT and FDG PET had been, for a time, the only imaging modalities to unveil abnormalities and to allow a prognosis assessment at the very initial phase of stroke (42). Now this is routinely done using MRI and especially diffusion weighted imaging (43). The isotopic methods are used in a secondary
60 period to evidence deafferentation and thus explain deficits which are not clearly related with the site of ischemic lesions (44). The crossed cerebellar diaschisis was the first example of such a phenomenon (45).
Figure 5 shows an example of sub-cortical / cortical deafferentation.
The accumulation of these ischemic lesions, both cortical and sub-cortical, may lead to vascular dementia which is characterized by an heterogeneous aspect of the perfusion. The heterogeneity of the brain perfusion is a frequently observed aspect in normal aging (46) and one must be accustomed to examinations of this population to decide if a perfusion heterogeneity is definitely pathologic or not.
2 dementia
Of particular importance is the distinction between vascular dementia and Alzheimer’s disease (AD).
Numerous studies show that this is possible (47-49). Parietal and temporal hypoperfusion or hypometabolism, more or less symmetric is the major sign of AD. An important negative sign being the sparing of the primary cortex (visual and sensori-motor) figure 6. This pattern can be evidenced with PET or SPECT. In this domain more than anywhere else, the confrontation with clinical presentation and morphological data is mandatory. For example, memory impairment is a prerequisite to evoke the diagnosis. Longitudinal studies are possible to assess the treatment effect (50). Moreover, functional imaging allows one to go further in differential diagnosis of dementia. A first group is the one of the fronto-temporal lobes atrophy, which have different clinical expressions.
The primary progressive aphasia, where language dysfunctions (syntactic and phonologic) are on the foreground. Morphologic imaging shows an atrophy of the left perisylvian region and functional examinations reveal a concordant hypoactivity (51,52).
The fronto temporal dementia. In this complex syndrome, where behavioral problems are typically the initial sign, the morphologic aspect is a frontal atrophy with an enlarged sylvian fissure. PET (53) and
SPECT (54) scans show a frontotemporal decreased metabolism or perfusion. In this context, an isolated posterior hypoactivity excludes the diagnosis.
61 The semantic dementia is characterized by a loss of conceptual knowledges enabling to produce and understand language. This syndrome is associated with atrophy of anterior temporal lobes, usually asymmetric and more marked on the left side. This atrophy relatively spares medial regions such as hippocampus. Functional imaging shows the same pattern (55).
The posterior cortical atrophy.
Here visual functions are altered. According to the main involved region the presentation is different: visual agnosia, color agnosia or prosopagnosia when ventral pathway is concerned, alexia, agraphy,
Balint’s syndrome when it is the dorsal one. The functional aspect is an hypoactivity of the posterior regions associated with a relatively preserved activity on the medial temporal lobes (56).
Dementia with extra-pyramidal signs.
Some pathologies of this neurodegenrative group raise difficult differential diagnosis problems with AD.
At the first rank is the dementia with Lewy bodies (DLB) in which fluctuation of consciousness and visual hallucinations are much more frequent than in AD. Yet, the positive diagnosis is difficult and the nosographic classification is not well established among AD variant with Lewy bodies, pure DLB
( without senile plaques and neurofibrilar degeneration), Parkison’s disease with dementia. For the diagnosis of pure DLB, morphologic imaging does not appear helpfull. In functional imaging, the extent of hypoactivity towards the occipital lobes looks more pronounced than in AD (57-59). Cortico basal degeneration is another circumstance where functional imaging could be useful. In typical cases, the hypoactivity is asymmetric, predominant on posterior frontal and parietal lobes (60-61). The evolution is towards a more widespread involvement of the entire hemisphere including the deep structures: striatum and thalamus (61).
In these 2 latter pathologies the functional study of the dopaminergic pathway is promising. The nigrostriate function assessed by FDOPA or a tracer of the dopamine transporter is more altered in DLB than in AD.
62 Mild cognitive impairment An important issue in the dementia domain is the early diagnosis of AD in a clinical situation termed
“mild cognitive impairment”. More generally it can be assumed that for the involved brain cortex region hypofunction precedes atrophy. To be detected on an individual basis this hypofunction must occurs in region were normal variations are limited. Although it is known that AD begins in the entorhinal cortex, an hypometabolism of this region is difficult to recognize. It appears more reliable to look for an hypometabolism in the posterior cingulate cortex (62,63)
3 movements disorders.
Parkinson’s disease (PD) is the most frequent pathology encountered in this field. But number of neurodegenerative diseases include tremor, rigidity and bradykinesia in their presentation. Since the development of ligands for dopamine membrane transporter and for D2 receptors labeled with 123I or 99m
Tc the study of dopaminergic pathways is more feasible in the clinical setting (64,65). The reduction of the striatal uptake of dopamine transporters tracers is the sign of the nigrostriatal dysfunction. In PD, this reduction is predominant in the putamen and, most of the time, asymmetric (Figure 7). These results reproduce those ones of 18F-DOPA PET explorations (66). Moreover, there is a correlation between the uptake reduction and the disease severity, and the time course of dopaminergic degeneration can be measured (67). In essential tremor, the uptake of such tracers is normal. In multiple system atrophy
(MSA), or in progressive supranuclear palsy (PSP) (71) the reduction is more diffuse in the putamen and the caudate. But it does not seem possible with these examinations to discriminate these pathologies for individual patient. Nevertheless, imaging of dopamine transporter has an impact on management of patients presenting with a possible PD or a supposed drug induced parkinsonism (study on 90 patients)
(68).
Imaging of D2 receptors show a reduced striatum uptake in MSA and PSP whereas it is normal in
Parkinson’s disease (69).
63 Metabolism and perfusion studies are also used to explore these extra-pyramidal syndromes. It is noticeable that the striatal CMRGlu is normal in PD (70). It is diminished in MSA and allows discrimination between PD and nigrostriate degeneration (72).
Current studies focus on relations between severity of the nigrostriatal dysfunction, assessed by the
18FDOPA and the presence of a genetic mutation (73). Possible side-effect of long term treatment by levodopa had been explored by brain blood flow (74) showing an alteration of the response to an acute dose of levodopa in sensori motor and ventrolateral prefrontal cortex. The neuroprotective effect of dopamine receptor agonist had been evaluated by a randomized study using the 123I -CIT (82 patients)
(75).
4 epilepsy
The main issue in medically untractable epilepsy is to correctly localize the epileptogenic zone in order to determine the site and the extent of the cortical resection to be done. For this purpose several methodologies had been developed using ictal and/or inter-ictal functional studies. The general pattern is an hypometabolism in the inter-ictal phase and an hyperperfusion during the ictal period. For temporal lobe epilepsy it is now well established that inter-ictal FDG PET (76) and ictal/interictal perfusion SPECT
(77) have the same efficiency in identifying the epileptogenic zone. The situation is less clear for neocortical epilepsy where subtraction from the ictal examination of the inter-ictal one, both coregistered with Magnetic Resonance Imaging (SISCOM) proved to be helpful to improve the interpretation of the
SPECT data (78,79).
In all these procedures the timing of the radiopharmaceutical injection in relation to the onset of the seizure activity is of paramount importance (80,81). The localizing power of an ictal study is as much greater as the perfusion tracer is injected earlier after the seizure onset. Delayed injection results in spread hyperactivity in which the epileptogenic zone cannot be isolated. Perfusion abnormality can last a long time after the seizure and could be related to psychotic episodes after complex partial seizure (82).
64 The classical pattern is sometimes missing or even inverted. Hypermetabolism during a supposed interictal phase had been thought to occur during discharge of deep epileptic focus not recorded by the surface EEG. On the contrary, hypoperfusion observed during an ictal examination could in fact unveil a
« steal » phenomenon (83).
Repeated seizures can cause subtle lesions that had been evidenced by imaging the benzodiazepine receptors. A diminution of the binding potential in the cerebellum controlateral to the temporal region responsible of partial epilepsy (17 patients), mimicking some kind of « crossed cerebellar diaschisis » has been found (84).
5 tumors
Probably due to the high background activity of the normal brain, the FDG PET does not appear here so effective than in other regions. In a study including 331 patients (85) the relationship between the activity, assessed by visual inspection , and the histologic grading has been established. The FDG uptake was qualitatively measured on a four-value scale – no uptake : 0, uptake less or equal to normal white matter :
1, uptake greater than normal white matter but less than normal grey matter : 2, uptake greater than grey matter : 3. Moreover, the degree of uptake with the survival – 94% of the patients with low uptake (0,1) survived for more than one year ( survival median : 28 months ), whereas only 29% of those ones with high uptake (2,3) did so (survival median 11 months). Yet, it remains many clinical situations where the decision making is difficult. Differentiating tumor recurrence from necrosis or scar, especially in the case of radionecrosis and low-grade tumors, is one of them. This gave impulse for the development of more specific tracers exploring the amino acid transport across the cell membrane. 11C-Methyl-Methionine has been frequently used to study brain tumors (86). With this agent, contrast of the tumor relative to the normal brain tissue is better than with the FDG. It permitted to assess the response of glioma to brachytherapy in 46 patients (87). It seems useful for differential diagnosis of low-grade gliomas (88). To overcome technical difficulties in relation with the short half-life of the 11C, other tracers, labeled with 18F has been proposed as the FluoroTyrosine (89). More recently, tracers suitable for SPECT imaging have
65 been synthesized. For example, the L-3-[123I]iodo- -methyl tyrosine (IMT) gives better results than FDG in some circumstances, such as low-grade recurrences of gliomas (90). It is also better than MIBI to distinguish progressive from non progressive low-grad astrocytomas after irradiation (91). In fact, 201Tl or
99mTc-MIBI had been used since a very long time (92) to make a positive image of brain tumors and assess their malignancy. The physiological uptake of MIBI by choroid plexus may be confusing. A review of
201Tl examinations in 90 patients with various brain tumors or processes concluded to a sensitivity of 72% and a specificity of 81 % for detecting the malignancy (93). In this study, imaging was done 15 minutes after the injection of tracer. More delayed acquisition (3 h.) is useful to further characterize the focal 201Tl accumulation. The kinetic of Tl uptake can be grossly quantified by computing a tumor/non-tumor ratio in two mirror ROIs. A retention index may be defined as the ratio between the delayed and the early tumor/non-tumor ratios (94).
A strategy based upon 201Tl and 123I IMT has been proposed to differentiate brain tumors and was evaluated in 65 patients. (95).
Conclusion
Since a 1995 partial review of the topic (96) a lot of events have occurred:
Clinical PET has become more affordable,
Resolution of SPECT camera steadily improves,
New tracers have been designed and some of them are commercially available,
Functional MRI has gained in maturity,
Spectroscopic MRI shows endless progress but supposes extended physico-chemical knowledge.
In this continuously changing landscape, nuclear techniques still produce effective results, useful in management of dementia, medically untractable epilepsy, complex movements disorders.
The trend is to focus on more specific molecules and to more closely study their kinetics in the human brain.
66 Efforts are also done to better characterize what a “normal” brain distribution of a specific activity is and to quantify the pathologic deviations from it.
Thus, the concept of molecular imaging is emerging, which aims at detecting the pathologic processes before they cause structural modifications, in a period where they are, hopefully, more amenable to treatments.
67 References:
1. Functional Brain Imaging (Part I) and (Part II) Seminars in Nuclear Medicine 2003 XXXIII (1) and (2)
2. Neirinckx R.D., Burke J.F., Harrison R.C., Forster A.M., Andersen A.R., Lassen N.A. The retention mechanism of Technetium-99m-HMPAO : intracellular reaction with glutathione. J Cereb Blood Flow Metab 1988 8 : S4-S12
3. Walovitch R.C., Cheesman E.H., Maheu L.JL, Hall K.M. Studies of the retention mechanism of the brain perfusion imaging agent 99mTc-Bicisate (Tc-ECD). J Cereb Blood Flow Metab 1994 14(suppl.) : S4-S11
4. Volkow N.D., Fowler J.S., Gatley S.J., Logan J., Wang G.J., Ding Y.S., Dewey S. PET evaluation of the dopamine system of the human brain. J Nucl Med 1996 37 : 1242-1253
5. Frost J.J., Rosier A.J., Reich S.G., Smith J.S., Ehlers M.D., Snyder S.H., Ravert H.T., Dannals R.F. Positron emission tomographic imaging of the dopamine transporter with [11C]-WIN 35,428 reveals marked declines in mild Parkinson’s disease. Ann Neurol 1993 34 : 423-431
6. Carroll F.J., Scheffel U., Dannals R.F., Boja J.W., Kuhar M.J. Development of imaging agents for the dopamine transporter. Med Res Rev 1995 15 : 419-444
7. Abi-Dargham A., Gandelman M.S., De Erausquin G.A., Zea-Ponce Y., Zoghbi S.S., Baldwin R.M., Laruelle M., Charney D.S., Hoffer P.B., Neumeyer J.L., Innis R.B. SPECT imaging of dopamine transporters in human brain with iodine-123-fluoroalkyl analogs of beta-CIT. J Nucl Med 1996 37 : 1129-1133
8. Kung H.F. Development of Tc-99m labeled tropanes : TRODAT-1, as a dopamine transporter imaging agent. Nucl Med Biol 2001 ; 28 : 505-508
9. Mozley P.D., Schneider J.S., Acton P.D., Plossl K., Stern M.B., Siderowf A., Leopold N., Li P.Y., Alavi A., Kung H.F. Binding of [99mTc]TRODAT-1 to dopamine transporters in patients with Parkinson’s disease and in healthy volunteers. J Nucl Med 2000; 41 : 584-589
10. Farde L., Ehrin E., Eriksson L., Greitz T., Hall H., Hedstrom C.G., Litton J.E., Sedval G. Substituted benzamides as ligands for visualization of dopamine receptor binding in the human brain by positron emission tomography. Proc Natl Acad Sci USA 1985 82 : 3863-3867
11. Mach R.H., Nader M.A., Ehrenkaufer R.L.E., Line S.W., Smith C.R., Luedtke R.R., Kung M.P., Kung H.F., Lyons D., Morton T.E. Comparison of two fluorine-18 labeled benzamide derivatives that bind reversibly to dopamine D2 receptors : in vitro binding studies and positron emission tomography. Synapse 1996 ; 24 : 322-333
12. Schwarz J., Oertel W.H., Tatsch K.. Iodine-123-idobenzamide binding in parkinsonism : reduction by dopamine agonists but not L-dopa. J Nucl Med 1996 ; 37 : 1112-1115
68 13. Pike V.W., Halldin C., Crouzel C., Barre L., Nutt D.J., Osman S., Shah F., Turton D.R., Waters S.L. Radioligands for PET studies of central benzodiazepine receptors and PK (peripheral benzodiazepine) binding sites – Current status. Nucl Med Biol 1993 ; 20 : 503-525
14. Pappata S., Samson Y., Chavoix C., Prenant C., Maziere M., Baron J.C. Regional specific binding of [11C]RO 15 1788 to central type benzodiazepine receptors in human brain : quantitative evaluation by PET. J Cereb Blood Flow Metab 1988 8 : 304-313
15. Millet P., Graf C., Buck A., Walder B., Westera G., Broggini C., Arigoni M., Slosman D., Bouras C., Ibanez V. Similarity and robustness of PET and SPECT binding parameters for benzodiazepine receptors. J. Cereb. Blood Flow Metab. 2000 ; 20 : 1587-1603
16. Abi-Dargham A., Laruelle M., Seibyl J., Rattner Z., Baldwin R.M., Zoghbi S.S., Zea-Ponce Y et al. SPECT measurement of benzodiazepine receptors in human brain with iodine-123-iomazenil : kinetics and equilibrium paradigms. J Nucl Med 1994 35 : 228-238
17. Pike V.W. Radiologands for PET studies of central 5-HT receptors and reuptake sites – current status. Nuc Med Biol 1995 ; 22 : 1011-1018
18. Proceedings of the Conference on the imaging of brain 5-HT1A receptors in vivo radioligands, clinical application and drug development. Nuc Med Biol 2000 ; 27 (5) Special issue.
19. Houle S., Ginovart N., Hussey D., Meyer J.H., Wilson A.A. Imaging the serotonin transporter with positron emission tomography : initial human studies with [11C]DAPP and [11C)DASB Eur J Nucl Med 2000 ; 11 :1719-1722
20. Volkow N.D., Ding Y-S., Fowler J.S., Gatley S.J. Imaging brain cholinergic activity with positron emission tomography : its role in the evaluation of cholinergic treatments in Alzheimer’s dementia. Biol Psychiatry 2001 49 : 211-220
21. Inoue T.J., Shibasaki T., Oriuchi N., Aoyagi K., Tomiyoshi K., Amano S., Mikuni M., Ida I., Aoki J., Endo K. 18F- -methyl tyrosine PET studies in patients with brain tumors. J Nucl Med 1999 40 : 399- 405
22. Pauleit D., Floeth F., Tellmann L., Hamascher K., Hautzel H., Müller H-W., Coenen H.H., Langen K.J. Comparison of O-(2-18F-Fluoroethyl)-L-Tyrosine PET and 3-123I-Iodo- -Methyl-L-Tyrosine SPECT in brain tumors. J Nucl Med 2004 ; 45 : 374-381
23. Ichise M., Meyer J.H., Yonekura Y. An introduction to PET and SPECT neuroreceptor quantification models. J Nucl Med 2001 ; 42 :755-763
24. Schmidt K.C., Turkheimer F.E. Kinetic modeling in positron tomography. Q J Nucl Med 2002 ; 46 :70-85
25. Logan J. Graphical analysis of PET data applied to revesible and irreversible tracers. Nucl Med Biol 2000 ; 27 : 661-670
26. Vera P, De Dreuille O, Bendriem B, Gardin I, Stievenart J-L, Menard J-F, Pare C, Bourguignon M, Bok B, Syrota A. Advantage of fan beam collimators for contrast recovery of hyperfixation in clinical SPECT.IEEE Trans Nucl Science 1997; 44 1:83-89
69 27. Hudson H.M., Larkin S. accelerated image reconstruction using ordered subsets of projection data. IEEE Trans Med Imaging 1994 13 :601-609
28. Matej S., Lewitt R.M. Practical considerations for 3-D image reconstruction using spherically symmetric volume elements. IEEE Trans Med Imaging 1996 15 :68-78
29. Chang L.T. A method for attenuation correction in radionuclide computed tomography. IEEE Trans Nucl Sci 1978 25 : 638-643
30. Zanzonico P. Positron emission tomography a review of basic principle, scanner design and performance, and current systems. Seminars in Nuclear Medicine 2004 XXXIV (2) : 87-111
31. Toyama H., Takeshita G., Takeuchi A., Anno H., Ejiri K., Maeda H., Katada K., Koga S., Ishiyama N., Kanno T., Yamaoka N. Cerebral hemodynamics in patients with chronic obstructive carotid disease by rCBF, rCBV, and rCBV/rCBF ratio using SPECT. J Nucl Med 1990 ; 31 : 55-60
32. Sabatini U., Celsis P., Viallard G., Rascol A ; Marc-Vergnes J-P. Quantitative assessment of cerebral blood volume by single-photon emission computed tomography. Stroke 1991 ; 22 :324-330
33. Baron J.C., Marchal G. Functional imaging in vascular disorders. in Brain Mapping The disorders (Mazziotta J.C., Toga A.W., Frackowiack R.S.J. Eds.) Academic Press – San Diego 2000 : 299-316
34. Heiss W-D., Herholz K. Assessment of pathophysiology of stroke by positron emission tomography. Eur J Nucl Med 1994 21 : 455-465
35. Mountz J.M., Liu H-G., Deutsch G. Neuroimaging in cerebrovascular disorders : measurement of cerebral physiology after stroke and assessment of stroke recovery. Seminars in Nuclear Medicine 2003 XXXIII (1) : 56-76
36. Baron J.C., Rougemont D., Soussaline F., Bustany P., Crouzel C., Bousser M.G., Comar D. Local interrelationship of cerebral oxygen consumption and glucoze utilisation in normal subjects and in ischemic stroke patients : a positron tomography study. J Cereb Blood Flow Metab 1984 4 : 149-149
37. Frackowiak R.S.J. The pathophysiology of human cerebral ischemia : a new perspective obtained with positron tomography. Q J Med 1985 ; 223 : 713-727
38. Vorstrup S., Brun B., Lassen N.A Evaluation of the cerebral vasodilatory capacity by the acetazolamide test before EC-IC bypass surgery in patient with occlusion of the internal carotid artery. Stroke 1986 ; 17 : 1291-1298
39. Kuroda S., Shiga T., Ishikawa T., Houkin K., Narita T., Katoh C., Tamaki N., Iwasaki Y. Reduced blood flow and preserved vasoreactivity characterize oxygen hypometabolism due to incomplete infarction in occlusive carotid artery diseases. J Nucl Med. 2004 ; 45 :943-949
40. Baron J.C., Bousser M.G., Comar D., Soussaline F., Castaigne P. Noninvasive tomographic study of cerebral blood flow and oxygen metabolism in vivo : Potentials, limitations and clinical applications in cerebral ischemic disorders. Eur Neurol 1981 ; 20 ; 273-284
41. Sperling B., Lassen N.A. Hyperfixation of HMPAO in subacute ischemic stroke leading to spuriously high estimates of cerebral blood flow by SPECT Stroke 1993 ; 24 193-194
70 42. Giubilei F., Lenzi G.L., Di Piero V., Pozolli C., Pantano P., Basttianello S., Argentino C., Fieschi C. Predictive value of brain perfusion Single-Photon Emission Computed Tomography in acute ischemic stroke. Stroke 1990 ;21 :895-900
43. Karonen J.O., Nuutinen J., Kuikka J.T., Vanninen E.J., Vanninen R.L., Partanen K., Vainio P.A., Roivainen R., Sivenius J., Aronen H.J. Combined SPECT and diffusion-weighted MRI as a predictor of infarct growth in acute ischemic stroke. J Nucl Med 2000 ; 41 (5) : 788-794
44. Kuroda S., Houkin K., Abe H., Mitsumori K. Transient ipsilateral blood flow reduction in the thalamus and cerebral cortex after pontine infarction. Neuroradiology 1996 38 : 239-242
45. Baron J.C., Bousser M.G., Comar D., Castaigne P. « Cross cerebelar diaschisis » in human supratentorial brain infarction. Trans Am Neurol Assoc 1980 105 :459-461
46. Waldemar G., Hasselbalch S.G., Andersen A.R., Delecluse F., Petersen P., Johnsen A., Paulson O.B. 99mTc-d,l-HMPAO and SPECT of the brain in normal aging. J Cereb Blood Flow Metab 1991 11 (3) : 508-521
47. Bakchine S., Habert M-O. Imagerie des démences apparentées à l’Alzheimer. in imagerie des démences (Bakchine S. et Semah F. Eds.) Expressions Santé Editions (Labs. Eisai Pfizer) 2002 Paris :47-60
48. Talbot P.R., Lloyd J.J., Snowden J.S., Neary D., Testa H.J. A clinical role for 99mTc-HMPAO SPECT in the investigation of dementia ? J Neurol Neurosurg Psychiatry 1998; 64 : 306-313
49. Read S.L., Miller B.L., Mena I., Kim R., Itabashi H., Darby A. SPECT in dementia : clinical and pathological correlation J Am Geriatr Soc 1995 ; 38 : 1243-1247
50. Nobili F., Koulibaly M., Vitali P., Migneco O., Mariani G., Ebmeier K, Pupi A., Robert P.H., Rodriguez G., Darcourt J. Brain perfusion follow-up in Alzheimer’s patients during treatment with acetylcholinesterase inhibitors. J Nucl Med 2002 ; 43 :983-990
51. Kempler D, Metter E.J., Riege W.H., Jackson C.A., Benson D.F., Hanson W.R. Slowly progressive aphasia : three cases with language, memory, CT and PET data. J Neurol Neurosurg Psychiatry 1990 ; 53 : 987-993
52. Sinnatamby R., Antoun N.,A., Freer C.E., Miles K. A., Hodges J. R. Neuroradiological findings in primary progressive aphasia : CT, MRI and cerebral perfusion SPECT. Neuroradiology 1996 38 : 232- 238
53. Ishii K., Sakamoto S., Sasaki M., Kitagaki H., Yamaji S., Hashimoto M., Imamura T., Shimomura T., Hirono N., Mori E. Cerebral glucose metabolism in patients with frontotemporal dementia. J Nucl Med 1998 ; 39 :1875-1878
54. Sjogren M., Gustafson L., Wikkelso C., Wallin A. Frontotemporal dementia can be distinguished from Alzheimer’s disease and subcortical white matter dementia by an anterior-to-posterior rCBF-SPECT ratio. Dement Geriatr Cogn Disord 2000 ; 11 : 275-285
55. Galton CJ, Patterson K ., Graham K., Lambon-Ralph M.A., Williams C., Antoun N., Sahakian B.J., Hodges J.R.. Differing patterns of temporal atrophy in Alzheimer’s disease and semantic dementia. Neurology 2001 ; 57 :216-225
71 56. Croisile B., Trillet M., Hibert O., Cinotti L., Le Bars D., Mauguiere F., Aimard G. Désordres visuo- constructifs et alexie-agraphie associés à une atrophie corticale postérieure [Visuo-constructional disorders and alexia-agraphia associated with posterior cortical atrophy] Rev Neurol 1991 147 : 138- 143
57. Pasquier J., Michel B.F., Brenot-Rossi I., Hassan-Sebbag N., Sauvan R., Gastaut J-L. Value of 99mTc- ECD SPET for the diagnosis of dementia with Lewy bodies. Eur J Nucl Med 2002 ; 29 :1342-1348
58. Luc J-P., Leduc V., Duhamel A., Lecouffe P., Pasquier F., Lamy-Lhullier C., Steinling M., Destée A. Technetium HMPAO SPECT study in dementia with Lewy bodies, Alzheimer’s disease and idiopathic Parkinson’s disease. J Nucl Med 1999 ; 40 :956-962
59. Lobotesis K., Fenwick J.D., Phipps A., Ryman A., Swann A., Ballard C., McKeith I.G., O’Brien J.T. Occipital hypoperfusion on SPECT in dementia with Lewy body but not AD. Neurology 2001 ; 56 : 649-643
60. Brooks D.J. Functional imaging studies in corticobasal degeneration Adv Neurol 2000 ; 82: 209-215
61. Markus H.S., Lees A.J. Lennox G., Marsden C.D., Costa D.C. Patterns of regional cerebral blood flow in corticobasal degeneration studied using HMPAO SPECT ; comparison with Parkinson’s disease and normal controls. Mov Disord 1995 10 : 179-187
62. Minoshima S., Giordani B., Berent S., Frey K.A., Foster N.L., Kuhl D.E. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer’s disease. Ann Neuro. 1997 42 :85-84
63. Huang C., Waklund L-O., Svensson L., Winblad B., Julin P. Cingulate cortex hypoperfusion predicts Alzheimer’s disease in mild cognitive impairment. BMC Neurol 2002 2 :9
64. Booij J., Tissingh G., Winogrodska A., Van Royen E.A. Imaging of the dopaminergic neurotransmission system using single-photon emission tomography and positron emission tomography in patients with parkinsonism. Eur J Nucl Med 1999 26 : 171-182
65. Remy P. L’imagerie fonctionnelle a-t-elle une place en clinique dans la maladie de Parkinson ? [Is functional imaging useful the clinical evaluation of Parkinson’s disease ] Rev Neurol 2003 159 : 5 pt 2, 3S57-3S61
66. Morrish P.K., Sawle G.V., Brooks D.J. 18F DOPA PET findings in early Parkinson’s disease. J Neuro Neurosurg Psychiatry 1995 ; 59 : 597-600
67. Winogrodzka A., Bergmans P., Booij J., Van Royen E.A., Stoof J.C., Wolters E.C. [123I]b-CIT SPECT is a useful method foe monitoring dopaminergic degeneration in early stage Parkinson’s disease. J Neurol Neurosurg Psychiatru 2003 ; 74 : 294-298
68. Lokkegaard A., Werdelin L., Friberg L. Clinical impact of diagnostic SPET investigations with a dopamine re-uptake ligand. Eur J Nucl Med 2002 ; 29 : 1623-1629
69. Van Royen E., Verhoeff NF, Speelman JD, Wolters EC, Kuiper MA, Janssen AG. Multiple systeme atrophy and progressive supranuclear palsy. Diminished striatal D2 receptor activity demonstrated by 123IBZM single photon emission computed tomography. Arch Neurol 1993 ; 50 : 513-516
72 70. Eidelberg D., Takikawa S., Moeller JR, Moeller J.R., Dhawan V., Redington K., Chaly T., Robeson W., Dahl J.R., Margouleff D., Fazzini E. et al. Striatal hypometabolism distinguishes striatonigral degeneration from Parkinson’s disease. Ann Neurol 1993 ; 33 : 518-527
71. Blin J., Baron J-C., Dubois B., Pillon B., Cambon H., Cambier J., Agid Y. Positron emission tomography study in progressive supranuclear palsy. Brain hypometabolic pattern and clinicometabolic correlations. Arch Neurol 1990 ;47 : 747-752
72. Burn D.J., Sawle G.V., Brooks D.J. Differential diagnosis of Parkinson’s diseaese, multiple system atropthy, and Steel-Richardson-Olszewski syndrome : discriminant analysis of striatal 18F-DOPA PET data. J Neuro Neurosurg Psychiatry 1994 ; 57 : 278-284
73. Thobois S., Robeiro M-J., Lohmann E., Dürr A., Pollak P., Rascol O., Guillouet S., Chapoy E., Costes N., Agid Y., Remy P., Brice A., Broussolle E. Young-onset Parkinson disease with and without Parkin gene mutations. Arch Neurol 2003 ; 60 : 713-718
74. Hershey T., Black K.J., Carl J.,L., McGee-Minnich L., Snyder A.,Z., Perlmutter J.S. Long term treatment and disease severity change brain responses to levodopa in Parkinson’s disease. J Neuro Neurosurg Psychiatry 2003 ; 74 (7) :844-851
75. Parkinson Study Group. Dopamine transporter brain imaging to assess the effect of Pramipexole vs Levopdopa on Parkinson’s disease progression. J A M A 2002 ; 287 :1653-1661
76. Bouilleret V., Valenti P., Hirsch E., Semah F., Namer I. J. Correlation between PET and SISCOM in temporal lobe epilepsy. J Nucl Med 2002 ; 43 : 991-998
77. Van Paesschen W., Dupont P., Van Driel G., Van Billoen H., Maes A. SPECT perfusion changes during complex partial seizures in patients with hippocampal sclerosis. Brain 2003 ; 126 (5) : 1103- 1111
78. Kaiboriboon K., Lowe V.J., Chantarujikapong S.I., Hogan R.E. The usefulness of subtraction ictal SPECT coregistered to MRI in single- and dual-headed SPECT cameras in partial epilepsy. Epilepsia 2002 43(4) : 408-414
79. Vera P., Kaminska A., Cieuta C., Hollo A., Stievenart JL., Gardin I., Ville D., Mangin JF., Plouin P., Dulac O., Chiron C. Use of subtraction ictal SPECT co-registered to MRI for optimizing the localization of seizure foci in children. J Nucl Med 1999 ; 40(5) : 786-792
80. Zubal I.G., Spanaki M.V., Mac Mullan J., Corsi M., Seibyl JP., Spencer S.S. Influence of technetium- 99m-hexamethylpropylene amine oxime injection time on single-photon emission tomography perfusion changes in epilepsy. Eur J Nucl Med 1999 26 (1) : 12-17
81. Calcagni M.L., Giordano A., Bruno I, Parbonetti G., Di Giuda D., De Rossi G., Troncone L., Colicchio G. Ictal brain SPECT during seizures pharmacologically provoked with pentylenetetrazol : a new diagnostic procedure in drug-resistant epileptic patients. Eur J Nucl Med Mol Imaging 2002 29 (10) : 1298-1306
82. Leutmezer F., Podreka I., Asenbaum S., Pietrzyk U., Lucht H., Back C., Benda N., Baumgartner C. Postictal psychosis in temporal lobe epilepsy. Epilepsia 2003 44 : 582-590
73 83. Lee H.W., Hong S.B., Tae W.S. Opposite ictal perfusion patterns of subtracted SPECT. Hyperperfusion and hypoperfusion. Brain 2000 123 (10) : 2150-2159
84. Kuji I., Sumiya H., Tsuji S., Ichikawa A., Tonami N. Asymmetries of benzodiazepine receptor binding potential in the inferior medial temporal lobe and cerebellum detected with 123I-iomazenil SPECT in comparison with 99mTc-HMPAO SPECT in patients with parietal epilepsy. Ann Nucl Med 1998 12 (4) 185-190
85. Padma M.V., Said S., Jacobs M., Hwang D.R., Dunigan K., Satter M., Christian B., Ruppert J., Bernstein T., Krau G., Mantil J.C. Prediction of pathology and survival by FDG-PET in gliomas. J Neurooncol. 2003 64 (3) : 227-237
86. Tsuyuguchi N., Sunada I., Iwai Y., Yamanaka K., Tanaka K., Takami T., Otsuka Y., Sakamoto S., Ohata K., Goto T., Hara M. Methionine positron emission tomography of recurrent metatstatic brain tumor and radiation necrosis after stereotactic radiosurgery : is a differential diagnosis possible ? J Neurosurg 2003 98 (5) : 1056-1064
87. Voges J., Herholz K., Holzer T., Wurker M., Bauer B., Pietrzyk U., Treuer H., Schroder R., Sturm V., Heiss W.D. 11C-methionine and 18F-2fluoro-deoxyglucose positron emission tomography : a tool for diagnosis of cerebral glioma and monitoring after brachytherapy with 125I seeds. Stereotactic Functional Neurosurg 1997 69 : 129-135
88. Herholz K., Holzer T., Bauer B., Schroder R., Voges J., Ernestus R.I., Mendoza G., Weber- Luxenburger G., Lottgen J., Thiel A., Wienhard K., Heiss W.D. 11C-methionine PET for differential diagnosis of low-grade gliomas. Neurology 1998 50 : 1316-1322
89. Wienhard K., Herholz K., Coenen H.H., Rudolf J., Kling P., Stocklin G., Heiss W.D. Increased amino acid transport into brain tumors measured by PET of L-(2-18F)fluorotyrosine J Nucl Med 1991 32 : 1338-1346
90. Bader J.B., Samnick S., Moringlane J-R. Feiden W., Schaefer A., Kremp S., Kirsch C-M. Evaluation of L-3-[123I]iodo- -methyltyrosine SPET and [18F]fluorodeoxyglucose PET in the detection and grading of recurrences in patients retreated for gliomas at follow-up : a comparative study with stereotactic biopsy. Eur J Nucl Med 1999 26 (2) : 144-151
91. Henze M., Mohamed A., Schlemmer H., Herfarth K.K., Mier W., Eisenhut M., Debus J., Haberkorn U. Detection of tumor progression in the follow-up of irradiated low-grade astrocytomas : comparison of 3-[123I]iodo- -methyl-L-tyrosine and 99mTc-MIBI SPECT. Eur J Nucl Med Mol imaging 2002 29 : 1455-1461
92. Ancri D., Basset J-Y., Lonchampt M.F., Etavard C. Diagnosis of cerebral lesions by Thallium 201. Radiology 1978 128 : 417-422
93. Dierckx R.A., Martin J.J., Dobbeleir A., Crols R., Neetens I., De Deyn P.P. Sensitivity and specificity of thallium-201 single photon emission tomography in the functional detection and differential diagnosis of brain tumors. Eur J Nucl Med 1994 21 :621-633
94. Lorberboym M., Mandell L.R., Mosesson R.E., Germano I., Lou W., Da Costa M., Linzer D.G., Machac J. The role of thallium-201 uptake and retention in intracranial tumors after radiotherapy. J Nucl Med 1997 ; 38 : 223-226
74 95. Matheja P., Rickert C., Weckesser M., Palkovic S., Löttgen J., Riemann B., Kopka K., Kuwert T., Wassmann H., Paulus W., Schober O. Sequential scintigraphic strategy for the differentiation of brain tumors. Eur J Nucl Med 2000 27 : 550-558
96. Stievenart J-L., Vera P., Verstichel P., Bok B., Masson M. Applications neurologiques de la tomographie d’emission de simple photon. [Neurological applications of single photon emission tomography] Rev Neurol 1995 151 (11) : 619-633
75 Chapter V – C. Marsault
Résultats de l’utilisation du scanner multibarrettes en neuroradiologie Claude Marsault Professeur des Universités et Chef de Service, Service de Radiologie, Hôpital Tenon, Paris, France
La neuroradiologie a d’emblée profité de l’acquisition spiralée en scanographie, essentiellement dans les explorations vasculaires, comme les artères à destinée encéphalique (vertébrales et surtout carotides) et également en intra-crânien (recherche d’anévrysme ou de malformations artério-veineuses). Par contre, les reconstructions cérébrales multiplanaires n’ont pas été profondément modifiées. Ainsi, l’angioscanner monobarrette était déjà un examen performant pour l’étude des axes vasculaires cervico-encéphaliques (1, 2). Avec l’apparition des multibarrettes, cet examen devient probablement la technique de choix non invasive dans l’exploration des artères cervicales et des vaisseaux encéphaliques. Il permet de plus d’évaluer la perfusion cérébrale. Comparativement au scanner monobarrette, les avantages majeurs du scanner multibarrettes pour l’étude des artères cervicales sont : la possibilité d’obtenir des images en phase artérielle pure grâce à la réduction de la durée d’acquisition et du sens crânio-caudal de l’acquisition ; la nette amélioration de la qualité de l’image reconstruite dans le plan sagittal avec la disparition de l’effet en marche d’escalier par l’obtention de coupes inframillimétriques avec reconstruction chevauchée; la réduction des artéfacts de mouvements et des artéfacts d’origine dentaire par l’amélioration de la résolution temporelle et par une meilleure correction du durcissement du faisceau de rayons X ; l’augmentation de la hauteur d’exploration avec la possibilité de visualiser au cours de la même acquisition tout l’axe artériel cervico-encéphalique. Dans l’étude des sténoses athéromateuses de l’artère carotide interne, ces améliorations permettent à la fois d’apprécier exactement le degré de sténose (3), la morphologie de la plaque athéromateuse (Fig.1) et d’éventuelles lésions associées au niveau des siphons carotidiens et de l’origine des TSA. Dans les dissections artérielles, l’angioscanner multibarrettes permet de préciser la localisation et l’extension lésionnelle, la présence de dissections multiples et l’existence d’un facteur favorisant comme la dysplasie fibro- musculaire. L’étude des vaisseaux encéphaliques a également bénéficiée de cette avancée technologique. La fiabilité de l’angioscanner dans la recherche des anévrysmes intracrâniens se confirme avec l’utilisation des multibarrettes (4). L’augmentation du volume exploré et la meilleure résolution spatiale longitudinale permettent la détection de lésions artérielles sténo-occlusives sur des branches artérielles plus distales (5). D’autre part, nous avons observé une plus grande facilité dans la réalisation de l’examen, au cours des situations d’urgences difficiles où les patients sont confus et agités, grâce à la rapidité d’acquisition de l’examen et à l’absence de contrainte positionnelle de la tête du patient. Pour l’étude des veines encéphaliques le scanner multibarrettes permet de diagnostiquer les thrombophlébites cérébrales à partir d’un examen angioscanographique veineux dédié comme le faisait déjà le scanner monobarrette (6). En revanche, un des avantages du scanner multibarrettes est de pouvoir faire le diagnostic de thrombophlébite cérébrale a posteriori, après une acquisition spiralée banale réalisée sans injection de produit de contraste, car pendant les deux premières semaines, le thrombus endoluminal est spontanément hyperdense, très bien visualisé sur les coupes MPR millimétriques et les reconstructions VRT (Fig.2). L’intérêt du scanner multibarrettes, dans l’étude de la perfusion cérébrale au décours d’un infarctus au stade aigu, permettrait de différencier la zone infarcie, de la pénombre ischémique et donc de sélectionner
76 les patients en vue d’une éventuelle thrombolyse (7, 8). La principale limite est la hauteur d’exploration, 24 mm avec un scanner 16 barrettes, responsable d’une méconnaissance des infarctus situées en dehors de ce volume exploré. Nous avons également observé un manque de sensibilité pour les petits infarctus territoriaux et lacunaires. Cependant, une meilleure couverture volumique est apportée aujourd’hui par les scanners à 64 barrettes (40 mm d’épaisseur en haute résolution) et l’évolution va encore se poursuivre. Quant à l’étude des lésions parenchymateuses, elle bénéficie des possibilités d’excellentes reconstructions tridimensionnelles. Mais, ceci concerne surtout les patients présentant une contre-indication à l’IRM. En conclusion, les améliorations obtenues sont le volume exploré, la réduction des artéfacts de mouvements et métalliques et l’amélioration de la résolution spatiale longitudinale et temporelle. Les améliorations attendues concernent essentiellement la rapidité du post traitement des images, l’amélioration de la résolution spatiale dans les trois plans de l’espace et l’augmentation de la zone de couverture dans la perfusion cérébrale.
1- Randoux B, Marro B, Koskas F et al. Carotid Artery Stenosis: Prospective Comparison of CT,
Three-dimensional Gadolinium-enhanced MR, and Conventional Angiography. Radiology 2001;
220: 179-185.
2- Zouaoui A, Sahel M, Marro B et al. Three-dimensional computed tomographic angiography in
detection of cerebral aneurysms in acute subarachnoid hemorrhage.
Neurosurgery. 1997 Jul; 41(1):125-30.
3- Chen CJ, Lee TH, Hsu HL et al. Multi-Slice CT angiography in diagnosing total versus near
occlusions of the internal carotid artery: comparison with catheter angiography. Stroke. 2004 Jan;
35(1):83-5.
4- Jayaraman MV, Mayo-Smith WW, Tung GA et al. Detection of intracranial aneurysms: multi-
detector row CT angiography compared with DSA.
Radiology. 2004 Feb; 230(2):510-8.
5- Skutta B, Furst G, Eilers J, Ferbert A, Kuhn FP. Intracranial stenoocclusive disease: double-
detector helical CT angiography versus digital subtraction angiography. AJNR Am J Neuroradiol.
1999 May; 20(5):791-9.
77 6- Ozsvath RR, Casey SO, Lustrin ES, Alberico RA, Hassankhani A, Patel M. Cerebral venography:
comparison of CT and MR projection venography. AJR Am J Roentgenol. 1997 Dec;
169(6):1699-707.
7- Eastwood JD, Lev MH, Wintermark M et al. Correlation of early dynamic CT perfusion imaging
with whole-brain MR diffusion and perfusion imaging in acute hemispheric stroke. AJNR Am J
Neuroradiol. 2003 Oct;24(9):1869-75.
8- Wintermark M, Reichhart M, Cuisenaire O et al. Comparison of admission perfusion computed
tomography and qualitative diffusion- and perfusion-weighted magnetic resonance imaging in
acute stroke patients. Stroke. 2002 Aug;33(8):2025-31.
Fig 1a Fig 1b
Fig.1 : Sténose athéromateuse serrée de l’artère carotide interne. Thrombus endoluminal de la pointe du bulbe bien visualisé sur les coupes MPR fines sagittale (a) et axiale (b)
78 Fig 2 : Scanner multibarrettes réalisé sans injection de produit de contraste. Reconstruction VRT.
Thrombophlébite du sinus longitudinal supérieur et des veines corticales adjacentes.
79 Chapter VI – J. Ruscalleda
Infections diseases of the central nervous system
Jordi Ruscalleda, Professor and Director, Servicio de Radiologia-Neuroradiologia, Hospital de la Santa Creu I Sant Pau, President –Elect of the E.S.N.R.. Barcelona, SPAIN
In spite of the great advances in diagnostic imaging as well as in therapeutic availabilities, CNS infections have not decreased their present morbi-mortality. The incidence and characteristics of infectious processes that can affect CNS are very different when we consider those processes in developed or undeveloped countries, when we analyse them from the geographical point of view or as regard to the different periods of life. Many factors are responsible for this different distribution and persistence of CNS infections. 1. - In the last two decades the increasing incidence of AIDS was under the major scope of CNS infections and hopefully nowadays is much better under control. 2. - The present aggressive and different treatments that induce an immunodepressed state are responsible of many CNS infections. 3. - Many viral infections with a not very effective treatment are involved in CNS infections 4. - The expansion of infections is made easier by the large movement of populations. CNS has a limited mechanism of defence represented by skull, meninges and BBB their involvement and failure is the first step in CNS involvement. Present imaging studies, mainly CT and MR, allow a close and prompt diagnosis.
Learning objectives To offer a large overview about the present different infectious processes involving CNS. To learn the different neuradiological patterns and differential diagnosis of this infectious processes To emphasise the progressive replacement of advanced MRI over TC as the method of choice in the approach of CNS infections.
CNS INFECTIONS
Unfortunately CNS infections still represents a significative group of processes with a quite severe dysfunction's in the follow-up of affected patients.
Several ways to present and describe CNS infections from the neuroradiological point of view: Clinical point of view, like neurologist, talking about fever, headache, neck stiffness, and loss of neurological functions or CSF findings. Physio-Pathological aspects of CNS infections, explaining meningeal changes, the abscess process formation, encephalitis or mechanisms of demielinated processes in AIDS. The morphological point of view showing different meningeal thickenings and contrast uptakes, describing round masses, granulomatous processes or focal and diffuse white matter diseases. And other way to explain this topic would be Causal: Traumatic infections
80 Surgical infections Pediatric infections AIDS related infections Facial and petrous infections
In my opinion all the aspects are important and helpful in the management of CNS infections. For all of that I insist on how important is the clinical and phisio-pathological knowledge of CNS infections and diseases. For academic and didactic purposes we classify CNS infections into: Brains Abscess Meningitis and Ventriculitis Encephalitis Parasitosis
MENINGITIS AND VENTRICULITIS. IMAGING
Inflammatory process of the dura matter, leptomeninges (pia and arachnoides) and CSF within the subarachnoid space. Meningoencephalitis represents an extension to the brain parenchyma. Ventriculitis represents an extension to ventricular ependyma. Meningitis needs a prompt diagnosis and specific treatment. Is an emergency because untreated patients have a fatal outcome.
1. - Normal meninges and extra-axial spaces Duramatter (pachymeninx): two layers: Outer or periosteal. Highly vascularized, of not true meningeal origin ending at the foramen magnum. Inner layer, embryiologically derived from the meninx and continuous with the spinal duramatter. Some reflections forms the falx cerebri, falx cerebelli and tentorium cerebelli. Leptomeninges (arachnoid and piamatter) The arachnoid is applied to the inner dura and the piamatter covers the brain.
2. - Clinical and pathophysiological features Signs and symptoms are fever, nuchal rigidity as well as neurological signs and symptoms related to stage of the illness, organism, age, state of previous health. There are four routes of entry infectious agents into the CNS Hematogeneous spread (arterial or venous) the most frequent Direct implantation: traumatic, lumbar puncture or surgery Local extension (air sinuses) Along the peripheral nervous system. Viruses: rabies and herpes simplex.
The most important pathogens: a) Acute Bacterial Meningitis Streptococcus pneumoniae 47% Neisseria meningitides 25% 59% in patients 19 years and older Haemophilus influenzae B 7% (part of human microflora) Listeria monocytogenes 8% Streptococcus group B 12% 45% in infants below 2 years
Meningococcal meningitides (13 different serogroups)
81 Tbc b) Viral meningitis Aseptic meningitis syndrome. LCR with pleocytosis with lymphocitic predominance. Nonpolio enteroviruses Mumps (the most common cause of aseptic meningitis) Arboviruses (Encephalitis) Herpes viruses (Encephalitis) HIV Adenoviruses (infants) Polioviruses types 1,2,3
Meningitis are classified according to inflammatory exudate, CSF exam and clinical evolution. Acute piogenic (bacterial) Aseptic (viral) Chronic (parasitic and fungi)
3. - Role of imaging The first purpose of CT or MRI is to detect possible complications of meningitis: Hydrocephalus and infarction. Gd Contrast enhancement is positive in 55-70% of infectious cases but insensitive in viral meningitis.
4. - Bacterial meningitis Acute bacterial (pyogenic) meningitis Microorganism Neonates escherichia coli and group B streptoccoci Infants, children: Haemophilus influenzae (basal) Adolescents: Neisseria meningitides 80% convexity Elderly: Streptococcus neumoniae. Lysteria monocytogenes immunocompromised : klepsiella. Anaerobic agents. (Ventriculitis) Fungi.(Meningoencephalitis)
CSF cloudy or purulent. Meningeal vessels engorged. Involvement of superficial arteries and veins, responsible of thrombosis and infarction. Two patterns of contrast enhancement Dural enhancement: follows the inner contour of the calvaria Pia-subarachnoid enhancement: extends into the depths of the cerebral and cerebellar sulci and fissures. Differential diagnosis with neoplastic subarachnoid dissemination (carcinomatosis), more irregular and nodular enhancement. b. - Tbc Meningitis Tbc is rising in the last two decades. 2-5% of patients with peripheral tbc have CNS tbc and in 10% of AIDS-related patients. Pattern: diffuse meningoencephalitis with a predominant characteristic of leptomeningeal opacification and thick gelatinous infiltrates in the basal cisterns, sometimes with subarachnoid granulomas and blood vessels involvement (spasm, arteritis, and thrombosis). Mechanisms of CNS infection: Rupture of subependymal or subpial granuloma into de CSF. Hematogeneous spread to the meningeal vessels.
82 c. - Neurosyphilis. Basal predominance with obliterative endoarteritis. d. - Neuroborreliosis (Lyme Disease) Borrelia burgdorferi. Cranial nerve palsy, mild encephalopathy and polyneuropathy. Multiple unspecific foci of brain infarction or borrelia granulomas.
5. - Complications or manifestations of bacterial meningitis a. - Hydrocephalus. Communicating hydrocephalus is the most frequent complication due to a leptomeningeal- ependymal fibrosis secondary to gelatinous exudates are the main cause and block of CSF resorption mainly at the level of the arachnoid villi B- Extra-axial fluid and pus collections. Subdural effusion and hygroma They are sterile collections secondary to irritation of the dura or veins inflammation with an increase of proteins and fluid in the subdural space. Easily detected by imaging. No treatment. Spontaneously resolved. Subdural Empyema 13-20% of intracranial infections. Bacterial and fungal infections of the calvaria and paranasal sinuses can produce and Empyema. The mechanism is a thrombophlebitis via the calvarial emissary veins. They are extra axial collections slightly hiperdense than CSF with a rim of contrast enhancement (inflammatory membranes). Possibility of thrombophlebitis of bridging veins and cerebral infarctions. Epidural empyema c. - Cerebritis and parenchymal abscess formation Spread from contiguous infections of the meninges by retrograde thrombophlebitis or direct extension into the brain via de pia matter or along the penetrating perivascular spaces: early phase of abscess formation. d. - Abscess formation e. - Central nervous system infarction Secondary to inflammatory arterial spasm, o inflammatory infections of the arterial walls: arteritis. Sometimes is difficult to differential infarction secondary to vascular involvement or focal brain encephalitis. (MRA useful).
6. - VENTRICULITIS Serious infectious process involving the cerebral ependyma secondary to meningitis, rupture of a parenchymal abscess, surgery, catheter placement. Imaging: Some degree of ventriculomegalia Subtle areas of periventricular low density Enhancement along ventricular walls IN chronic stages periventricular calcifications may be seen especially in perinatal ventriculitis especially in the so-called TORCH infection: Toxoplasma Other (syphilis, HIV) Rubella Cytomegalovirus Herpesvirus
7. - Acute aseptic (viral) meningitis
83 Clinical syndrome with lymphocitic pleocytosis in the LCR
8. - Cytomegalovirus (CMV) Is a ubiquitous DNA virus belonging to the herpesvirus family. Severe neurological dysfunction. The hallmark in periventricular calcifications detected by CT. CMV has special affinity for the metabolically active neuroblasts of the subependymal matrix and regional vasculature with a result of subependymal degeneration and calcification.
9. - Fungal Meningitis a) Criptococcus neoformans The most frequent fungus that enters the body via the respiratory tract, then spread hematogeneously from the lungs to the CNS. Primary manifested as meningitis, although parenchymal mass lesions can also develop. Highly prevalent in AIDS. Imaging: Meningitis with cystically dilated perivascular spaces filled with mucoid material as a response to the immune system (gelatinous pseudocysts) and parenchymal criptococcomas formation.
10. Parasitic Meningitis Cysticercosis (taenia solium) Ingestion of eggs in contaminated water or food. In the CNS Neurocysticercosis may be parenchymal, leptomeningeal or intraventricular. When the scolex lodges de brain develops a cystic covering around it with a first inflammatory parenchymal reaction with a granulation and connective capsule formation. When the larva dies a secondary inflammation and posterior calcification
11. - Toxoplasmosis (TORCH group). Toxoplasma gondii Congenital: meningitis, chorioretinitis, hydrocephalus and intracranial calcifications.
12. - Non-infectious meningitis Neoplastic meningitis Sarcoidosis Chemical meningitis Cranial hypotension Postsurgical states
ENCEPHALITIS. CEREBRITIS. BRAIN ABSCESS.
Encephalitis Generalised and diffuse infection of the brain. Often as a result of a viral infection due to prevention and treatment of bacterial diseases, increase of immunosuppresed patients (like AIDS) and in the course of transplant and cancer patients. Different types according to the site and tempo of infections. Viruses can lead to: Meningitis Acute infective encephalitis Acute disseminated encephalomielitis Subacute or chronic encephalitis
84 Encephalitis and myelitis Herpes simplex encephalitis (type 2 predominantly in temporal lobe) Enteroviruses and arboviruses encephalitis
Mechanism of CNS viral infection Infections of the CNS by viruses begin with the local growth of virus in nonneural tissue. Spread of viruses to the CNS primarily occurs by the Hematogeneous or neural route. Most of them gains access through the bloodstream (viremia). The viruses protect themselves against the reticuloendotelial system (RES) entering and growing in lymphocytes (measles and mumps). HIViruses enter mononuclear cells that carry the CD4 antigen. Poliovirus infects and grows in the lymphoid tissue of the gut. Arboviruses grow in the spleen and lymph nodes. From there viruses gain the CNS through perivascular spaces traversing the endothelium by pinocytosis or growing into the endothelial cells. Entrance in the CSF is through the epithelial cells of the choroid plexus.
Once in the CNS two major factors affect the general pathologic features: The cell type infected (different susceptibility): specific viral receptors. The host's immune response The tempo leads to a varied appearance of CNS viral infections a) Cells susceptibility Coxsackie, echovirus and mumps rarely infect neurons but frequently meninges. Poliovirus infects neurons (motoneurons) leaving sensory pathways untouched. Rabies infects neurons and much less oligodendrocytes Herpesvirus infects neuron and glial cells: predilection for cell population in limbic system. JC virus attacks only oligodendrocytes leading to demielination
Host immune response Humoral response against the virus Acquired antibody after previous infections or vaccination. Local infections is quelled (sofocada) by IgA in the respiratory tract, tears, saliva or gut. IgA or IgM restricts blood-borne dissemination. Antibodies in tissue spaces prevent spread of infection between cells. Cell-mediated response directed against the infected cell
Pathological features Macroscopic: meningeal opacity, vascular congestion and brain swelling. Microscopically: infiltration of brain by inflammatory cells. Early on by polymorphonuclear cells Later on by lymphocytes, plasma cells and large mononuclear cells. Perivascular cuffing of mononuclear cells in the Virchow-Robin spaces in small venules and thicker cuffs of lymphocytes around larger vessels are characteristic. Microscopic response of host cells: hypertrophy and proliferation of microglial cells (mainly in the cortex and deep grey matter), astrocytosis present when necrosis has occurred), neuronal changes (the result of terminal hypoxia or brain swelling. Cytoplasm vacuolation specific of the spongiform encephalopathy) and presence of inclusion bodies (specific of viral infection)
85 ACUTE INFECTIVE ENCEPHALITIS
Brain damage is the result of viral intracellular growth and the host's inflammatory response. Most common: herpes, rabies, arthropos-borne viruses and enteroviruses (polio). Brain necrosis is frequent either selective or complete brain infarction. Herpes viruses: simplex type 1 and 2 (HSV-1, HSV-2), CMV, Epstein-Barr V., varicella-zoster v., B virus, herpesvirus 6 and 7. Perivascular cuffing and inflammatory infiltrates are key features. Necrosis present in the more aggressive.
HSV-1 is the cause of 95% of all herpetic encephalitis Necrosis of temporal and Occ-frontal lobes. Less frequent in insula, occipital and cingulate gyrus. Putamen frequently spared. Trigeminal ganglion is the site of viral reactivation o a latent infection with spread along his branches. Biopsy is not needed because imaging is quite specific and the non-toxic treatment with acyclovir. Imaging HSV-1. Uptake of technetium pertechentate in various regions mainly in temporal lobe positive in 85% of cases. CT: hypodensity in 75% of cases present in the first 2-3 days. Hemorrhage frequent and highly suggestive but sometimes difficult to be seen by CT. MR study of choice. Temporal and inferior frontal lobes involvement. Basal ganglia spared. Often bilateral involvement. Gyriform enhancement.
ACUTE DISSEMINATED ENCEPHALOMYELITIS (ADEM)
5 days-2 weeks after viral illness or a vaccination. Headache, fever and drowsiness and focal neurological deficits. Pervious demyelination is the hallmark of ADEM with a probably immunologic mechanism. MR study of choice. Scattered plaques throughout the white matter of cerebellar and cerebral hemispheres. No mass effect. Contrast enhancement very variable. Differential diagnosis with ME. High-dose of steroids is the treatment.
SUBACUTE ENCEPHALITIS
Includes: Subacute Sclerosing panencephalitis (measles virus) Progressive Multiphocal Leucoencephalopathy (PML). JC-virus HIC encephalitis Tropical Spastic paraparesis (HTLV-1) CMV encephalitis Creutzfeldt-Jakob disease (proteinaceous particle: the prone)
All of them have and a relatively insidious onset. Creutzfeldt-Jakob disease (proteinaceous particle: the prion) Human spongiform encephalopathy as a result of infection by a slow unconventional virus. The infective prion is a proteinaceous infectious particle that resists activation by procedures that modify nucleic acids. They contain little or no nucleic acid and do not evoke an immune response. 1/1m. Dementia. Poor prognosis. Brain atrophy non-specific. Pathologic changes: neuronal loss, reactive astrocytosis, neuronal vacuolation with spongiform changes. MR: to exclude treatable lesions. Hypersignal T2 in the corpus striatum (frequent). Cortical hyperintensities have been described. Atrophy with rapid progression. MRE, decreased NAA/Cr. PET:
86 decreased perfusion and hypometabolism.
CEREBRITIS ANS ABSCESS
Decline in the incidence and mortality (14%) thanks to the efficient use of antibiotics. Source of infection: local or blood-borne. The first related to trauma or petrous and sinusal infections. The second related to infections in the respiratory tract and in immunocompromised patients. 25% of brain abscess have an unknown origin. Abscess formation follows different stages described by Enzmann: 1) Early cerebritis 2) late cerebritis 3) early capsule formation 4) late capsule formation. The abscess is preceded by focal cerebritis with endothelium swelling of the local capillaries and migration of polymorphs, perivascular infiltration, focal oedema, and petechial hemorrhage displayed on MRI as a focal area of unspecific edema. Progression to abscess occurs when a central zone of necrosis becomes better defined and liquefied with a peripheral collagen capsule. The collagen capsule is usually less well developed on the ventricular side likely related to differences in blood supply a weak point for daughter abscess formation. Abscesses from Hematogeneous origin are mainly located at the grey-white matter junction. MR imaging features of brain abscesses display the capsule as an iso to slightly hyperintense signal on T1 and hypointense on T2 probably due to the presence of paramagnetic free radicals. The capsule enhances with gadolinium. The centre of a mature abscess with necrotic material, displays on T1 a low signal higher than CSF and high signal on T2 similar to CSF or perilesional vasogenic edema.
Thallium-201 scanning may be useful in differentiating an abscess from a necrotic tumour because there is preferential uptake of thallium by tumors particularly of those of higher grade. (Not clear).
Differential diagnosis: Primary brain tumors Metastasis Septic and aseptic infarction Resolving hematoma Thrombosed aneurysms Arterio-venous malformations Tumefactive MS Lymphoma
MRE Abscess cavity with a lack of normal metabolites often contains amino acids and lactate, succinate and acetate that are not present in necrotic tumors.
CNS TUBERCULOSIS Incidence variable in diferent countries and population. 1.5/105/year. Hematogenous spread with small subpial or subependymal cortical focus of infection (Rich focus). When such a focus ruptures it contaminates the subarachnoid spaces and cerebrospinal fluid and spreads along the cereborspinal fluid pathways giving rise to tuberculous meningitis. Other manifestations are: Tuberculomas Tuberculous abscess Tuberculous cerebritis Pachymeningitis Spinal areachnoiditis Intraspinal tuberculoma
87 TBC meningitis Proliferative arachnoiditis and meningeal exudate predominantly in interpeduncular and pontomesencephalic cisterns progressively impeding de CSF circulation (communicanting hydrocephalus) and arteries and veins may become involved (vasculitis). CT and MR imaging, obliteration of basal cisterns and contrast enhancement of basal meninges. Hydrocephalus present in more than 50% of cases Vasculitis by direct invasion of vessel wall may lead to spasm and thrombosis with hemorrhagic infarction mainly at the basal ganglia present in more than 25% of cases. Granulomatous tuberculous meningitis is uncommon with diffuse or circunscribed granulomas in the basal cisterns. A more diffuse chronic leptomeningeal infection is called leptomeningitis. Parechymal tuberculomas is thougth to be secondary to an infective focos elswhere in the body. They can be single or multiple, small or large and can be located enywhere in the cerebrum, brainstem and posterior fossa. Two forms a) noncaseating granulomas with or without contrast enhancement and only abbormal signal on MR or b) Caseating granuloma with a typical ring-enhancing lesion. A target sign with presence of central calcification in a hypodense center of a ring enhancing lesion is characteristic but nor pathognomonic.
Ricketsiosis Gram.negative nonmotile bacteria a) Rocky Monutain Spotted fever Ricketsia rickettsii spreads hematogenously producing vasculitis with damage to the endothelial blood vessels walls of any organ. Cutaneous rash (palms, soles and anterior aspects of distal extremities) and mialgias. Brain lesions: perivascular accumulations of mononuclear cells (typhus nodule) with arterial infarction, cerebral edema and diffuse meningeal enhancement. Epidemic typhus (R. Prowazekii). Inades the endothelial cells of blood vessels. Q fever (Coxiella burnetii)
Spirochetes (gram.negatives organisms) Syphillis Lyme Disease (borrelia burgdorferi) Leptospirosis
PARASITES Cerebral malaria Toxoplasmosis gondii Amebiasis Neurocysticercosis
Amebiasis (entamoeba histolitica). Fecal-oral transmission. Reproduction in the colon. Hematogeneous dissemination can reach the CNS. Brain abscesses caused by E. Histolytica are similar to those produced by bacteria, tuberculosis, nocardia with an hipodense central zone, a ring-enhanced capsule and marked surrounding edema.
Schistosomiasis More than 200 million in Asia, tropics and subtropic areas. Schistosoma haematobium, japonicum and mansoni. Infected water. Skin of humans. Systemic veins and lymphatics and maturation of the larvae in the liver.
88 Brain imaging ara homogeneous or heterogeneous lesions with contrast enhancement and edema. No specific signs.
Toxoplasmosis. Toxoplasma gondii. Intrauterine infection: chorioretinitis, encephalomyelitis, hydrocephalus and microcephaly. AIDS. 28% of patients have toxoplasmosis. Lesions typically located in the corticomedullary junction and in the basal ganglia. CT and MR are useful for diagnosis and follow-up. Lesions dysplay tipical pattern of and abscess. The enhancement of the capsule is in relation to the immunity capacity of inflammatory reaction. Hyperintense masses on T2 represents areas of necrotizing encephalitis in early toxoplasmosis and the isointense masses, seen after treatment, probably represents organizing abscesses. Rapid response to treatment (12-15 days) confirms the diagnosis of toxoplasmosis and failure to respond to antibiotic treatment suggest another diagnosis. Is frequent that two different diesease processes may be occurring simultaneously. In AIDS differential diagnosis is between toxoplasmosis and lymphoma
ToxoplasmosisLymphomaCTHyperdense noncontrast CT Subapendymal spreadSPECT PETNO increased uptakeHypermetabolism, resulting in increased tracer activityMREIncreased lipid and lactate peaks and a deceased in other metabolitesMild-moderate increase in lipid and lactate but a large increase in choline peaks. Hydatidic disease Echinococcus granulosus and E. Multiloculares. Dog and carnivore is the definite host (intestinal). Eggs excreted and eaten by grazing animals and embrio released and through bowell wall go into the portal venous or lymphatic system. Liver the embrio matures into a cyst.
Cerebral hydatidic cyst usually unilocular. CT shows a well-defined, smooth, thin-walled, homogeneous cystic lesions similar in density to CSF. Capsule is difficult to be seen an enhancement in uncommon. Edema rare. With MR the capsule is better seen.
Cysticercosis Wide variety of neurologic syndromes induced by CNS infestation of cysticerci, le larva of Taenia Solium. Endemic in many areas (South America, Africa, Asia. East Europe. The CNS is involved in 60-90% of patients with cystecircosis. Parenchymas lesions of 10mm or less. Central hemisphere and basal ganglia. Subaracnoid lesions: cortical sulci, basal cisterns, intraventricular. ImagingEscobar's Stages 1.- Vesicular stage: the larva is seen as a small marginal nodule into a small cyst containing clear fluid. The parasite may remain in this stage for years. No contrast enhancement. 2.- Colloidal vesicular stage. The larva beguins to degenerate as a result of host's immune response. Scolex shows signs of hyaline degeneration and gradual schrinkage. Fluid becomes turbid and the capsule thicker. Surrounding edema. Contradt enhencement and hiperdense contents. 3.- Granular nodule stage. Capsule thickens and scolex mineralise. Edema regresses. 4.- Nodular calcified stage. Lesion completely mineralized.. No edema.
89 FUNGAL INFECTIONS
Criptococcus neoformans Coccidioidomycosis Histoplasmosis Blastomicosis Candidiasis Aspergillosis Mucormycosis
With The advent of immunosuppressive therapy in organ transplant patients and HIV disease fungal infections has become less rare. Fungi may exist as single cells (yeast) or in colonies (hyphal form) and may coalesce and form micelia. Hematogeneous spread. Yeast forms: blastomyces, Candida, Coccidioides, cryptococcus, histoplasma and torulopsis. Hyphal forms: Aspergillus, mucormycosis, pseudallescheria.
Aspergillosis Aspergillomas are close to the paranasal sinuses, and display abscesses not specific from other causes. 50% cases associated hemorrhage Low density due to the presence ef calcium, magnesium, manganese and iron.and decreased signal intensity on T2w.
Mucormycosis Diabetes high risk. The triade of diabetic ketoacidosis, meningoencephalitis and naso-orbital infection haigly suggest the diagnositc of mucormycosis. Other risk factors: metabolic acidosis: sepsis, severe dehydration, chronic renal failure. Propensity for vascular structures: arteritis, ischemic changes, hemorrhagic infarcts and aneurysms formations. Hystoplasmosis. Candidiasis Coccidioidomycosis Cryptococcal infection: the most common in AIDS patients. Meningitis producing hydrocephalus. Noenhncing lesions in the basal ganglia filling the Virchow-Robin spaces produced by mucoid material.
CNS infections in Pediatric population. Intrauterine and neonatal: malformations Infants: destructive lesions Congenital are infections transmited from the mother. Neonatal the first 4 weeks of life. The immune system is not fully developed. TORCH infections.
90 Chapter VII – J. Ruscalleda
CT and MR of neurocritic patient: diagnostic and prognostic value.
Jordi Ruscalleda Professor and Director, Servicio de Radiologia-Neuroradiologia, Hospital de la Santa Creu I Sant Pau, President - Elect of the E.S.N.R.. Barcelona, SPAIN
All CNS lesions are relevant, however some of them, due to their nature, extension and/or form of presentation, require the vigilance, control and management from part of specially trained medical and nursing personnel, in order to foresee, identify of react to all critical situations that may provoke a permanent brain damage.
Many CNS pathological processes require the assistance and benefit of Neurological Intensive Care Units (NICUs) either from the beginning, or during the pathological course, or as a consequence of the performed therapies. Among them we would like to mention the stroke, the severe cranio-encephalic traumas and the anoxic encephalopaty secundary to cardiorespiratory failure.
The NICUs utilize several monitoring devices to control end record the events that may lead to an irreversible neurological damage, such as the recording of the intracranial pressure (IPC), the evaluation of the cerebral blood flow (Intracranial Doppler) in order to recognize the vascular spasm or obstruction, the EEG monitoring of the cerebral acitivity, the hemodinamic arterial and venous control, and the recording of the somatosensory, motor or auditory evoked potentials. These are some of the present techniques that may be used to maintain a close and effective control of the vital parameters, as well as of the brain parenchyma functions.
The advanced neuroradiological examinations, e.g. CT and MR, when applied with the objective to reach a profound evaluation of the structural and functional alterations of the CNS, constitute an important part in the activity of the NICUs, either as to the comprehension and management of these patients when a life-threatening event related to a neurological cause occurs, or in order to define a short- or middle-term prognosis with a high degree of sensitivity and specificity, or to foresee the degree of neurological impairment that these lesions may provoke.
We present a review of the impact of the CT and MR studies in the management of these patients, either in the diagnostic or the prognostic phase.
91 Chapter X– L. Picard
Middle Cerebral Artery Aneurysm’s. Interest and indications of Endovascular Treatment 187 cases
Luc Picard, Serge Bracard, L.Thuillier René Anxionnat, Ariel Lebedinsky, Stephanos Finitsis, Francesco Ramos, Department of Diagnostic and Interventional Neuroradiology Hôpital Neurologique, Nancy, France
From October 1992 until December 2004, 940 patients who presented with 1120 aneurysms were observed in the Department of Neuroradiology. 238 aneurysms ( 21,2 %) were located on middle cerebral artery. This location concerned 21,5% of the patients. This study is realized on 174 patients ( 187 aneurysms ) with middle or long term follow up; the clinical and angiographic follow up has been realized at 6 months, 1 – 3 and 5 years. 83 patients presented with ruptured aneurysms – 104 aneurysms were unruptured ( fortuitous discovery or neurologic disturbances )
Indications : According to an excellent cooperation between neuroradiological and neurosurgical team, as far it is possible, we first try to treat the intracranial aneurysms by endovascular approach. Consequently 152 aneurysms ( 81,3 % ) were successfully treated by endovascular occlusion : 75 ruptured and 77 unruptured; for 7 patients ( 3,7 % ), the attempt of endovascular occlusion failed.
Anatomical Results in 174 patients ( 187 aneurysms ): 75 ruptured and 77 unruptured aneurysms were treated. Among the ruptured aneurysms, complete occlusion ( 100 % ) was achieved in 22 cases ( 29,3 % ), good occlusion ( > 90 % ) in 38 cases ( 50,7 % ) and partial occlusion ( < 90 % ) in 15 ( 20 % ). For the unruptured aneurysms, the results were a little better : complete occlusion in 24 ( 31,2 % ), good occlusion in ‘é ( 54,5 % ) and partial occlusion in 11 ( 14,3 % ). If we add complete and good occlusion on both ruptured and unruptured aneurysms, good anatomical results ( > 90 % ) were obtained in 126 cases ( 82,9 % ). The late middle term follow up is characterized by 14 recanalizations but only 5 patients needed to be retreated either by neurosurgery or by endovascular approach.
Clinical results : According to the Glasgow Outcome Scale, 134 patients ( 72 % ) are Grade I and 28 ( 15 % ) Grade II what means 87 % of very good clinical outcome. Only six patients ( all ruptured ) were Grade IV/V. When we know the seriousness of the ruptured middle cerebral artery aneurysms, such results can be considered as very interesting.
Incidents and Complications : 26 technical incidents and/or complications were observed on 187 procedures : 17 during the endovascular approach and 9 during the post procedural week.
Among the per procedural complications, we find 3 aneurysmal sac ruptures ( 1,6 % ), 8 thrombo embolic events ( 4,2 % ), 5 strokes and 1 erratic coil migration. It is interesting to emphasize that all the aneurismal sac ruptures were and remained asymptomatic without any worsening.
92 Post procedural complications : 4 rebleedings – 4 ischemic events – 1 hematoma related to the femoral puncture. Among the precocious rebleedings, we observed 2 deaths directly related to this complication.
Learning curve : The analysis of the complication rate shows that the maximum of complications has been observed during the first years of our experience, between 1992 and 1996. This first period was the beginning of the techniques of coiling; now the complication rate is dramatically reduced.
Conclusions :
The evolution of treatment indications of MCA aneurysms is very slow but certainly inescapable. This localization is reputed to be a poor indication of endovascular approach. The tridi angiography has really modified our possibilities allowing us a better understanding of angioarchitecture. Thanks to these technical improvements, the MCA aneurysms can be considered as an excellent indication for coiling allowing excellent anatomical and clinical results.
93 Chapter XI – S. Braccard
Extra and Intracranial dissection: diagnosis and therapy
Serge Bracard, René Anxionnat, Jean Christophe Lacour, Ariel Lebedinsky, Francesco Ramos, Stephanos Finitsis, Luc Picard Department of Diagnostic and Interventional Neuroradiology Hôpital Neurologique, CHU de Nancy, Nancy, France
DISSECTIONS OF CERVICAL ARTERIES
Cervical artery dissection is one of the most frequent causes of stroke. The annual incidence of spontaneous carotid- artery dissection is ranged from 2.5 per 100,000 to 3 per 100,000. Dissections of the carotid and vertebral arteries usually arise from an intimal tear that allows blood to enter the wall of the artery and to form an intramural hematoma. This hematoma is located within the layers of the tunica media, but it may be eccentric. A subintimal dissection tends to result in stenosis of the arterial lumen, whereas a subadventitial dissection may cause aneurismal dilatation of the artery.
Clinical Manifestations Patients with carotid artery dissection typically present unilateral facial and cervical pain accompanied by a partial Horner’s syndrome and followed hours or days later by cerebral or retinal ischemia. Cranial- nerve palsies can be detected in more than 10 percent of patients. The lower cranial nerves are the most commonly affected, particularly the hypoglossal nerve. Patient with vertebral-artery dissection typically present pain in the back of the neck or head. Ischemic symptoms occur in more than 90 percent of patients. Transient ischemic attacks are less frequent after vertebral- artery dissections than after carotid-artery dissections.
Imaging In about 15 to 25% of patients, dissections are detected in two or more vessels, and these multivessel dissections often appear to have occurred at the same time. Magnetic resonance techniques are replacing conventional angiography as the gold standard in the diagnosis of dissections of the carotid and vertebral arteries, for it may display the intramural hematoma itself as a crescentic shape adjacent to the vessel lumen and often spiraling along the artery. Fat- suppression techniques are important to differentiate intramural hematomas from the surrounding soft tissues. Ultrasonographic techniques are useful in the initial assessment, an abnormal pattern of flow is identified in more than 90 percent of patients
Prognosis The reported rate of death from dissections of the carotid and vertebral arteries is less than 5 percent. The local evolution is usually good: about 90 percent of stenosis eventually resolve, two thirds of occlusions are recanalized, and one third of aneurysms decrease in size. This improvement takes place largely within the first two to three months after the dissection and is rare after six months. Persistent extra cranial aneurysms may exceptionally cause thromboembolic complications, but they never rupture. In our French multicentric study (432 patients, mean follow-up of 31 months), the risk of a recurrent dissection is about 1% and the risk of recurrent ischemic stroke is also about 1 percent particularly during the first month.
94 Treatment To prevent thromboembolic complications, anticoagulation with intravenous heparin followed by oral warfarin for three to six months has been recommended for all patients with acute dissections of the carotid or vertebral artery. Endovascular treatment, consisting of percutaneous balloon angioplasty and placement of one or more metallic stents, has supplanted surgery as the initial therapy of choice once medical therapy fails. If needed in emergency, cervical angioplasty may be combined with intra arterial thrombolysis. Later, aneurysms may be treated by covered or uncovered stents, however this treatment is seldom necessary and the long-term results of carotid stenting are unknown.
DISSECTION OF INTRA CRANIAL ARTERIES
The real incidence of SAH due to a dissecting aneurysm rupture is unknown and is probably underestimated. For histologic reasons the great majority of intracranial dissections related to SAH are located in the posterior circulation. Despite the attention paid to this pathology in the past years the published series remain short and there are still no consensus in the management of this group of patients. Several series report a high rate of rebleeding especially in pseudoaneurysmal types. Most of these rebleedings occur in the first few days after the haemorrhage and early treatment is thus recommended. Our study involved a retrospective review of 27 patients with 29 dissections treated over a 16-year period mainly by endovascular treatment (EVT). Endovascular treatment was performed in the acute stage in 12/29 dissections, occlusion was performed using coils at the dissection site in 6 and with proximal balloon occlusion in 6. Wrapping was performed in one case. 16 dissections were not treated mainly for anatomical reasons. In this group, 3 patients died, one of them from rebleeding. Angiographic follow-up performed in the 13 surviving patients demonstrated initially misdiagnosed lesion in 1 and worsening lesions in 5 which led in delayed EVT in 5 and surgical clipping in 1. One of these dissections located on a dominant vertebral artery was treated after a subsequent rupture using a stent and coils to preserve the patency of the parent vessel. Four ischemic complications related to EVT resulted in a moderate disability in 2 patients. No rebleeding occurred after EVT, 1 patient died due to a poor initial clinical status, other patients improved. In the 10 patients conservatively treated, 4 patients died, 3 from a poor initial clinical status, 1 from rebleeding and 6 had a good clinical outcome. Of the 27 patients, 3 had a rebleeding and 1 died from this rebleeding. Seventeen patients (63%) had a good recovery, 6 (22%) had a moderate disability and 4 (15%) died.
Conclusion: EVT provides effective protection against rebleeding. Occlusion with coils at the dissection site, when possible, is the current method of choice. Other options are parent artery occlusion with balloons, while the use of stent may allow to preserve the permeability of the vessel in specific cases.
95 Chapter XII– S. Braccard
Acute and chronic brain ischemia: diagnosis and treatment Serge Bracard, René Anxionnat, Xavier Ducrocq, Ariel Lebedinsky, Stephanos Finitsis, Luc Picard Department of Diagnostic and Interventional Neuroradiology Hôpital Neurologique, CHU de Nancy, Nancy, France
Stroke Therapy The majority of ischemic strokes are due to thromboembolic arterial occlusion. Over the past few years, there have been intensive investigations regarding intravenous therapy for the treatment of acute ischemic stroke. At the present time, tissue plasminogen activator (rt -PA), when administered within the three hours of symptom onset has been shown to be an effective therapy. The benefits were demonstrated in the NINDS trial in 1995. Intra arterial thrombolysis is thought to be more effective than intravenous rt-PA. In PROACT II, patients within 6 hours of symptom onset with ACM occlusion were randomised to receive intra arterial thrombolysis with systemic heparinization versus heparinization alone. A good or excellent score on modified Rankin scale was achieved in 40% in the intra arterial group versus 25% in the control group. Intracerebral hemorrhage rates were increased in the intra arterial group, however no difference in overall mortality was observed. A combined approach that uses the speed of initiation of therapy with IV rtPA and the improved recanalizations efficacy of rapidly administered local IA rt-PA may improve patient outcome from major stroke. In the first studies, combined intravenous – intra arterial thrombolysis seems to be more efficient but need larger studies to be accepted. Further research is being conducted in the use of mechanical devices (like MERCI trial) with good results. The advantages of theses approaches include lack of systemic and hemorrhagic complications.
Carotid stenting Carotid stenosis may cause ischemic events by reducing cerebral blood flow or by acting as a source of thromboemboly. Randomized studies have established carotid endarterectomy to be an effective therapy for patients with significant carotid stenosis. Additionally, CEA may reduce the risk of ischemic events and overall mortality for patients with asymptomatic stenosis. Carotid stenting (CAS) is the less invasive percutaneous procedure that is being investigated as an alternative to CEA. At the present time carotid stenting may be particularly useful for patients who are poor surgical candidates, have received prior radiation or have restenosis or bilateral lesions.
96 In the past few years, evidence is growing that CAS might be an alternative to CEA and some series showed comparable major stroke and deaths rate of CEA and CAS. In order to reduce embolization of plaque fragments to the brain during CAS, cerebral protection devices have been developed. In the French EVA 3S study, the risk of any stroke within 30 days was about 3 times that of patients treated with cerebral protection and the safety committee of EVA3 S recommended to stop unprotected CAS .
Intracranial stenosis Atherosclerotic disease of the intracranial vessels accounts fort approximatively 10% of ischemic stroke. Despite antithrombotic therapy many patients have recurrent ischemic events. In the French GESICA multicentric study 44% of 102 patients who were treated with maximal antithrombotic therapy had ischemic events during the 24 months follow-up period. Studies of intracranial angioplasty and/or stenting have shown high technical success rates of more than 90%. However, compared with extra cranial vessels, angioplasty of intracranial vessels has a higher complication rate. In the GESICA study, 28 angioplasties were performed with 4 complications (14.2%), 2 deaths: 1 arterial rupture, 1 reperfusion haematoma and 2 strokes. During the follow up period (mean follow-up: 19.5 months) only 1 TIA was observed but no stroke.
97 98