Digestion
DIGESTION: the process of making food absorbable by changing it and breaking it down into simpler chemical compounds.
The usable parts of food (called nutrients) can’t be used by your body until they are absorbed into the cells & tissues of your body. They can’t be absorbed unless they are small & soluble ---soluble means that they can be dissolved. So the proteins, carbohydrates, & fats in any food have to be digested, i.e. changed into a form that can be absorbed and used by the body.
The main nutrients in food exist as large proteins, fats, & carbohydrates; which must be converted by the body into small amino acids, simple sugars, and fatty acids.
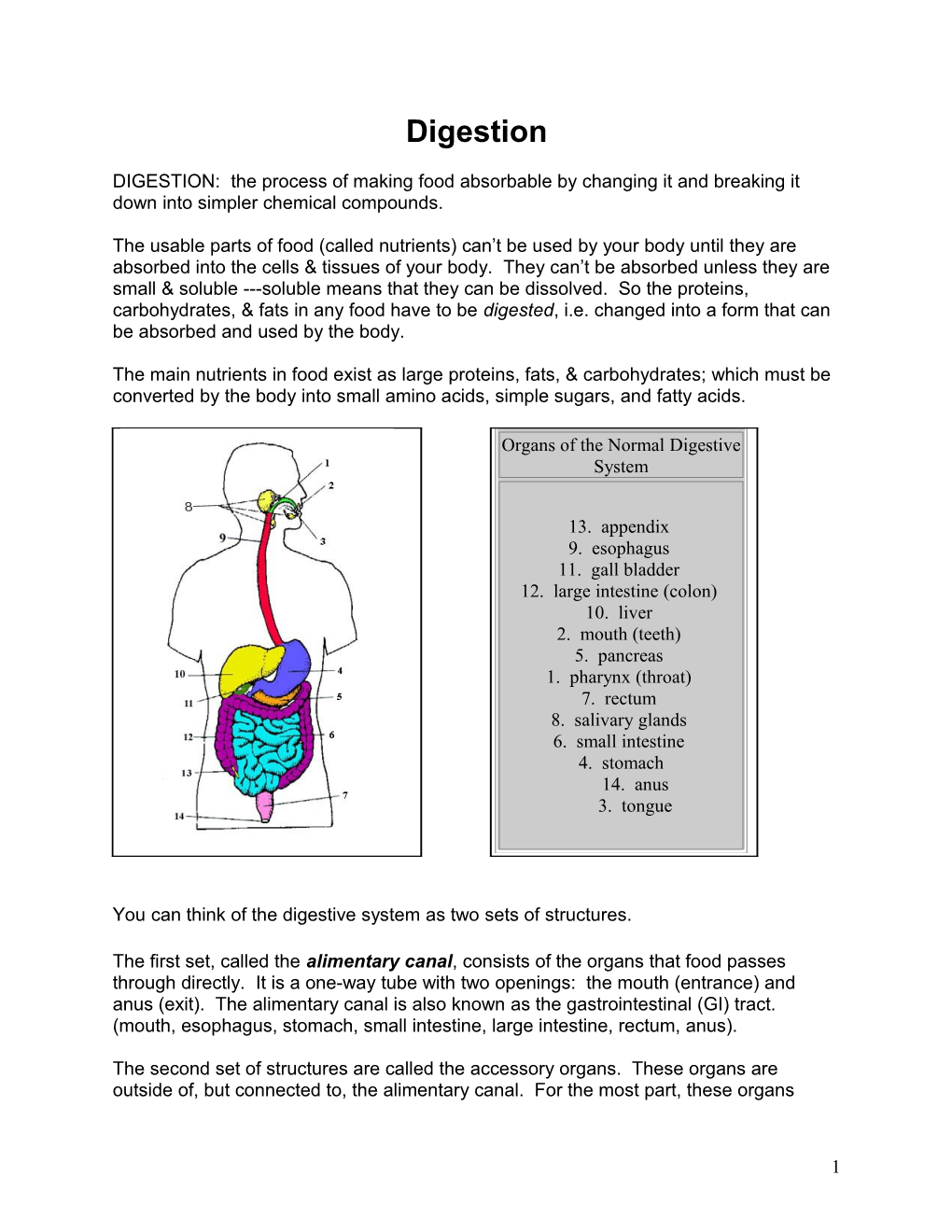
Organs of the Normal Digestive System
13. appendix 9. esophagus 11. gall bladder 12. large intestine (colon) 10. liver 2. mouth (teeth) 5. pancreas 1. pharynx (throat) 7. rectum 8. salivary glands 6. small intestine 4. stomach 14. anus 3. tongue
You can think of the digestive system as two sets of structures.
The first set, called the alimentary canal, consists of the organs that food passes through directly. It is a one-way tube with two openings: the mouth (entrance) and anus (exit). The alimentary canal is also known as the gastrointestinal (GI) tract. (mouth, esophagus, stomach, small intestine, large intestine, rectum, anus).
The second set of structures are called the accessory organs. These organs are outside of, but connected to, the alimentary canal. For the most part, these organs
1 produce chemicals (digestive enzymes) that are used during the process of digestion. Food that is being digested DOES NOT directly enter any of the accessory organs. Instead, the accessory organs/glands produce their chemicals & then the chemicals are released into the alimentary canal where they do their job.
ORGANS OF the ALIMENTARY CANAL Note: The structures are listed in the order in which food passes through them.
Organ Enzymes Present What Happens Here mechanical digestion of all food (teeth amylase (in chewing & grinding) mouth saliva) chemical digestion of carbohydrates begins food passes from mouth through the esophagus none esophagus to the stomach pepsin mechanical digestion of food (churning Stomach gastric juice of stomach walls) (bypassed) hydrochloric acid chemical digestion of proteins begins (HCl )* chemical digestion of carbohydrates, pancreatic juice proteins, & lipids continues & is small intestine intestinal juice completed (partially bypassed) bile* the small, soluble nutrients (sugars, amino acids, fatty acids) are absorbed water is absorbed from unusable, large intestine none indigestible wastes (feces) rectum none feces are temporarily stored feces are eliminated (egested) from the anus none body
As you can see from the chart, there are two types of digestion, chemical & mechanical.
When you read "mechanical digestion", think chewing, churning or grinding. These are physical processes that break food into smaller pieces, but DO NOT change them chemically. The importance of mechanical digestion is that by breaking food into smaller pieces it increases the surface area on which
2 digestive enzymes can react during chemical digestion. Chemical digestion is straight forward: it involves chemicals (digestive enzymes) and the process of hydrolysis. Large chemical nutrients are chemically converted to their smaller subunits.
· The chemicals marked with a "*" are technically NOT enzymes, but they are chemicals that help to break down food. HCl is hydrochloric acid, which is a fairly strong acid. Bile is a liquid that assists in the digestion of lipids (fats). In fancy terms we say that "bile emulsifies fats", which translates as: bile breaks big globs of fat into smaller globs of fat. Enzymes in the small intestine have an easier time digesting small globs of fat.
· Notice that digestion only occurs in three organs: the mouth, stomach, and small intestine. In the gastric bypass patient, most of the stomach, and a great part of the small intestine is bypassed, making digestion of foods less efficient. This is known as malabsorption.
Accessory Organs of the Digestive System
Accessory What it does Organ tongue helps mix food with saliva, assists in swallowing salivary produces saliva (which contains the enzyme amylase) glands amylase chemically digests carbohydrates produces bile liver bile EMULSIFIES fats (lipids) gall bladder stores bile, then releases into small intestine (bypassed) produces pancreatic juice, which is a mixture of digestive enzymes Pancreas (bypassed) pancreatic juice ends up in the small intestine where it assists in completing the digestion of proteins, lipids, & carbohydrates
3 Digestion is the extraction of essential nutrients from ingested food. ● Digestion begins in the mouth by breaking down food by chewing. ● Chewed food moves through the esophagus and into the intestinal tract, where chemical processes complete the digestive process. ● Digestion is completed in the small intestine where most of the nutrients are absorbed. ● Large intestine serves primarily to: Absorb water Absorb electrolytes Eliminate the waste products of digestion ● Indigestible food particles are stored in the sigmoid colon until they are eliminated through the rectum.
4 Stomach ● The function of the stomach is to breakdown the chewed food into a semi-fluid mass of partly digested food, known as chyme.***
● Chyme is then pumped into the duodenum (first section of the small intestine). The rate of movement of the stomach contents (chyme) to the small intestine is balanced with the rate of pancreatic and biliary secretions, to permit efficient extraction of nutrients. ***
***IMPORTANT NOTE: This process which is completed in the stomach, duodenum (beginning of small intestine), and part of the jejunum(farther along part of small intestine), does not happen anymore after a RNY gastric bypass. After RNY the chewed food from the mouth goes into the small pouch that is left, which is then dumped directly into a farther along part of the small intestine. There are no pancreatic and biliary secretions coming into this part of the small intestines anymore. These secretions will not be available until the food reaches the common channel (the lower part of the “Y” connection. This is the malabsorptive part of the Roux en Y gastric bypass procedure.
A “normal” stomach also includes secretion of: ● Acid ● Intrinsic factor ● Pepsin ● Mucus ● Bicarbonate ● These secretions are: Important for digestion. Normally very balanced, a mismatch of these secretions can lead to peptic ulcer disease.
In the RNY gastric bypass patient most of these secretions are no longer available for digestion, as the majority of the stomach has been separated from the pouch.
5 Small Intestine Approx 20 ft in length (although every person is somewhat different) and about 1 inch wide and fills most of the abdomen.
Duodenum = approx 10 inches (connects to the normal stomach) (bypassed in RNY)
Jejunum = approx 8 ft (middle portion) (partially bypassed in RNY)
Ileum = approx 12 ft (connects the to the large intestine)
Function of the Duodenum (bypassed in RNY) ● Neutralize the acid in the food slurry delivered from the stomach. ● Mix the food slurry with the pancreatic and biliary secretions.
Function of the Jejunum (partially bypassed in RNY) ● To absorb nutrients, water, and electrolytes.
Functions of the Ileum ● Provides same functions as jejunum, but has the unique function of absorbing bile acids and intrinsic factor, recycling these chemicals in the body. Inability to reabsorb intrinsic factor causes a major disability in the form of vitamin B12 deficiency, which leads to pernicious anemia. Intrinsic factor isn’t introduced into the RNY small intestine until the connection of the lower limb of the “Y” which is somewhere within the jejunum. Therefore all pancreatic and bile juices are mixed with the food for a much shorter period of time than in the “normal” digestive system. Food moves slowly and “normally” takes 3 – 10 hours to move from stomach through ileum (end of small intestine). This takes a much shorter time in the RNY patient. ● 90% of absorption of nutrients occurs within the small intestine.
NOTE: Whereas the “normal” small intestine is approx 20 ft long, the long- limb RNY gastric bypass patient has only 5 ft of common channel left after bypass. The short-limb has approximately 7 ½ ft of common channel left.
6 Some extra info on internal organs effecting the digestive tract: Liver, Gallbladder and Pancreas ● Produce digestive enzymes and hormones to facilitate the breakdown of food particles.
Liver plays a major role in: ● The portal vein carries recently absorbed nutrients from the stomach and intestine, as well as hormones secreted by the pancreas and GI tract, to the liver for processing. ● Regulates blood levels of fats, protein, and carbohydrate, needed by the muscles, brain, heart, and other organs to fundtion adequately. ● Drug metabolism ● Normal rate of production of red blood cells. ● Vitamin K production, which is necessary for normal blood clotting.
Gall Bladder ● Holds the bile, created by the liver, until it is needed to digest the food in the “normal “stomach.
Spleen ●The function is to filter out foreign substances as well as old degenerating blood cells from the bloodstream.
7 Why protein supplementation? It’s about Absorption
Proteins form the body’s main structural elements and are found in every cell and tissue. Take away the water, and about 75 percent of your weight is protein. Your body uses proteins: ● for growth ● to build and repair bone muscles hair connective tissue skin internal organs blood virtually every other body part or tissue
Besides building cells and repairing tissue, proteins form antibodies to combat invading bacteria & viruses; they build nucleoproteins (RNA & DNA). They make up the enzymes that power many chemical reactions. They also carry oxygen throughout the body and participate in muscle activity.
At least 10,000 different proteins make you what you are and keep you that way.
Hormones, antibodies and enzymes that regulate the body’s chemical reactions are all made of protein. Without the right proteins, blood won’t clot properly and cuts won’t heal.
Each protein is a large complex molecule made up of a string of building blocks called amino acids. The 20 amino acids the body needs can be linked in thousands of different ways to form thousands of different proteins, each with a unique function in the body.
Your body can’t use food protein directly. So after protein is ingested, digestive enzymes break the protein into shorter amino acid chains, and then into individual amino acids. In the gastric bypass patient , this normal digestive process is bypassed. These digestive enzymes are not available until they meet with the food protein in the common channel of the small intestine, and then have only about 5 – 7 ½ ft (compared to 20 ft in a “normal” digestive tract) to do their job. The amino acids then enter the blood stream and travel to the cells where they are incorporated into proteins the body needs.
Nine of the 20 amino acids required by human beings are considered “essential” because they come only from the diet; the other 11 are considered “nonessential” because the body can make them.
8 AMINO ACIDS
1 = Pro Score 100 3 = Sci Fit 5 = Pro Blend 55 7 = Shaklee Energizing Soy 2 = Pure Whey Stack 4 = ProCel 6 = HDT 5+1 1 2 3 4 5 6 7 Amino Acid X X X X X X X TRYPTOPHAN (Essential Amino Acid) A natural relaxant, helps alleviate insomnia by inducing normal sleep; reduces anxiety & depression; helps in the treatment of migraine headaches; helps the immune system; helps reduce the risk of artery & heart spasms; works with Lysine in reducing cholesterol levels. X X X X X X X LYSINE (Essential Amino Acid) Insures the adequate absorption of calcium; helps form collagen (which makes up bone cartilage & connective tissues); aids in the production of antibodies, hormones & enzymes. Recent studies have shown that Lysine may be effective against herpes by improving the balance of nutrients that reduce viral growth. A deficiency may result in tiredness, inability to concentrate, irritability, bloodshot eyes, retarded growth, hair loss, anemia & reproductive problems. X X X X X X X METHIONINE (Essential Amino Acid) Is a principal supplier of sulfur which prevents disorders of the hair, skin and nails; helps lower cholesterol levels by increasing the liver’s production of lecithin; reduces liver fat and protects the kidneys; a natural chelating agent for heavy metals; regulates the formation of ammonia and creates ammonia-free urine which reduces bladder irritation; influences hair follicles and promotes hair growth. X X X X X X X PHENYLALANINE (Essential Amino Acid) Used by the brain to produce Norepinephrine, a chemical that transmits signals between nerve cells and the brain; keeps you awake & alert; reduces hunger pains; functions as an antidepressant and helps improve memory. X X X X X X X THREONINE/THERONINE (Essential Amino Acid) Is an important constituent of collagen, Elastin, and enamel protein; helps prevent fat buildup in the liver; helps the digestive and intestinal tracts function more smoothly; assists metabolism and assimilation.
9 X X X X X X X VALINE (Essential Amino Acid) Promotes mental vigor, muscle coordination and calm emotions. X X X X X X X LEUCINE & ISOLEUCINE (Essential Amino Acids) They provide ingredients for the manufacturing of other essential biochemical components in the body, some of which are utilized for the production of energy, stimulants to the upper brain and helping you to be more alert. X X X X X X ARGININE Studies have shown that it has improved immune responses to bacteria, viruses & tumor cells; promotes wound healing and regeneration of the liver; causes the release of growth hormones; considered crucial for optimal muscle growth and tissue repair. X X X X X TYROSINE Transmits nerve impulses to the brain; helps overcome depression; Improves memory; increases mental alertness; promotes the healthy functioning of the thyroid, adrenal and pituitary glands. X X X X X X GLYCINE Helps trigger the release of oxygen to the energy requiring cell-making process; important in the manufacturing of hormones responsible for a strong immune system. X X X X SERINE A storage source of glucose by the liver and muscles; helps strengthen the immune system by providing antibodies; synthesizes fatty acid sheath around nerve fibers. X X X X X X GLUTAMIC ACID/GLUTAMINE Considered to be nature’s “Brain food” by improving mental capacities; helps speed the healing of ulcers; gives a “lift” from fatigue; helps control alcoholism, schizophrenia and the craving for sugar. X X X X X ASPARTIC ACID Aids in the expulsion of harmful ammonia from the body. When ammonia enters the circulatory system it acts as a highly toxic substance, which can be harmful to the central nervous system. Recent studies have shown that Aspartic Acid may increase resistance to fatigue and increase endurance. X TAURINE Helps stabilize the excitability of membranes which is very important in the control of many biochemical changes that take place in the aging process; aids in the clearing of free radical wastes. X X X X X X CYSTINE Functions as an antioxidant and is a powerful aid to the body in protecting against radiation and pollution. It can help slow down the aging process, deactivate free radicals, neutralize toxins; aids in protein synthesis and prevents cellular change. It is necessary for the formation of the skin, which aids in the recovery from burns and surgical operations. Hair and skin are made up of 10-14% Cystine. X X X X X X X HISTADINE Found abundantly in hemoglobin; has been used in the treatment of rheumatoid arthritis, allergic diseases, ulcers & anemia. Deficiency can cause poor hearing. X X X X X PROLINE Is extremely important for the proper functioning of joints and tendons; also helps maintain and strengthen heart muscles. X X X X X ALANINE Is an important source of energy for muscle tissue, the brain and central nervous system; Strengthens the immune system by producing antibodies; helps in the metabolism of sugars and organic acids.
10 The average*** person (the “normal”, NON-gastric bypass patient) needs 50-65 grams*** of protein each day. Considering malabsorption of at least 50%**, the RNY patient will need 100-140 grams per day minimum, which cannot be eaten as food because of the small size of the pouch. **Note: Depending on the length of bypass, the RNY patient may absorb as little as 25% or less. But it is normally agreed that even a short proximal will not absorb more than 50%. ***Note: Adults need a minimum of 1 gram of protein for every kilogram of body weight per day to keep from slowly breaking down their own tissues. That’s about 8 grams of protein for every 20 lbs. Malnourished, septic, pregnant, injured or burned patients will require more protein, in the order of 1.5-2.0 g/kg daily. Extra protein is also required after surgical procedures and illness.
According to Sally Myers, RD and regular contributor on nutritional issues to the WLS- related newsletter “Beyond Change”: “How to determine grams of protein you need daily when not yet at ideal weight: Subtract 120 from your current weight. Multiply that answer by .25 and add it to 120. Base your protein needs on that number. Extra protein is not needed for fat mass.”
Around the world, millions of people don’t get enough protein. This protein malnutrition leads to the condition known as kwashiorkor. Lack of protein can cause growth failure loss of muscle mass decreased immunity weakening of the heart and respiratory system death
Clinical signs and symptoms of malabsorption and maldigestion
Clinical sign or symptom Deficient nutrient
General Weight loss Calorie Loss of appetite, amenorrhea, decreased libido Protein energy
Skin Psoriasiform rash, eczematous scaling Zinc Pallor Folate, iron, vitamin B12 Follicular hyperkeratosis Vitamin A Perifollicular petechiae Vitamin C Flaking dermatitis Protein energy, niacin, riboflavin, zinc Bruising Vitamin K Pigmentation changes Niacin, protein energy Scrotal dermatosis Riboflavin Thickening and dryness of skin Linoleic acid Head Temporal muscle wasting Protein energy Hair Sparse and thin, dyspigmentation Protein
11 Easy to pull out Eyes History of night blindness Vitamin A Photophobia, blurring, conjunctival inflammation Riboflavin, vitamin A Corneal vascularization Riboflavin Xerosis, Bitot's spots, keratomalacia Vitamin A Mouth Glossitis Riboflavin, niacin, folic acid Bleeding gums Vitamin C, riboflavin Cheilosis Riboflavin Angular stomatitis Riboflavin, iron Hypogeusia Zinc Tongue fissuring Niacin Tongue atrophy Riboflavin, niacin, iron Scarlet and raw tongue Niacin Nasolabial seborrhea Pyridoxine Neck Goiter Iodine Parotid enlargement Protein Thorax Thoracic 'rosary' Vitamin D
Abdomen Diarrhea Niacin, folate, vitamin B12 Distention Protein energy Hepatomegaly Protein energy Extremities Edema Protein, thiamine Softening of bone Vitamin D, calcium, phosphorus Vitamin D Bone tenderness Vitamin C Bone ache, joint pain Protein, calories Muscle wasting and weakness Thiamine Muscle tenderness, muscle pain Thiamine Hyporeflexia Nails Flattening, brittleness, luster loss, spooning Iron Transverse lines Protein Neurologic Tetany Calcium, magnesium Paresthesias Thiamine, vitamin B12 Loss of reflexes, wrist drop, foot drop Thiamine Loss of vibratory and position sense, ataxia Vitamin B12 Dementia, disorientation Niacin
Blood Anemia Iron, vitamin B12, folate Hemolysis Phosphorus
The patient who gives a history of progressive weight loss, polyphagia, excessive flatus, diarrhea, bulky and foul-smelling stools, food particles or fat in the stool, abdominal distention, muscle wasting, bone pain, bleeding, weakness, tetany, paresthesia, glossitis, cheilosis or dermatitis is giving you the "classical" history of severe intestinal malassimilation.
Specific vitamin and mineral deficiencies Vitamin/mineral Clinical manifestation
Vitamin A Eyes Night blindness Xerosis (dry bulbar conjunctiva)
12 Bitot's spots (conjunctiva plaques) Keratomalacia (corneal ulceration) Skin Hyperkeratosis
Vitamin B12 Hematologic, neurologic systems Anemia Nonreversible loss of vibratory and position sense Paresthesia Gastrointestinal Diarrhea Vitamin C Skin Perifollicular papules (brittle hair) Perifollicular hemorrhages Gum bleeding Skin purpura, ecchymosis Vitamin D Bone Bone pain and softening Joint pain Rickets Proximal myopathy Bruising Vitamin K Bleeding
Vitamin B6 Skin Seborrheic dermatitis (Pyridoxine) Cheilosis Glossitis Niacin Dermatitis Diarrhea Dementia Thiamine CVS Congestive heart failure CNS Wernicke's encephalopathy Wernicke-Korsakoff syndrome Zinc Skin Acrodermatitis enteropathica Alopecia Taste Hypogeusia Folate Hematologic, neurologic systems Anemia Reversible loss of position and vibratory sense
CVS = cardiovascular system; CNS = central nervous system
It is not uncommon for the patient to think the toilet is malfunctioning because several flushings are needed to remove the stool. A greasy character and truly rancid odor are indicative of increased stool fat, but are often absent until late. These complaints are often readily passed over by the busy physician. At such time, physical findings are usually absent, but hyperactive bowel sounds may be noted, especially in small intestinal disease. If symptoms are intermittent or if they progress slowly over many years, patients may exhibit vague, seemingly unrelated symptoms such as chronic fatigue and depression, long before the physician considers the possibility of serious organic disease.
Carbohydrate malabsorption will result in symptoms of diarrhea and excessive flatus (gas). Malabsorbed carbohydrates that enter the colon are fermented by colon bacteria into gases. Stools seem to float on the water because of their increased gas content (not because of their fat content). This often happens when the gastric bypass patient
13 begins to eat more carbohydrates, instead of protein. Given sufficient time, fat and muscle will be catabolized. Physical examination may reveal signs of weight loss from both fat stores and lean body mass. The patient will be weak and will easily develop fatigue. Fat loss will generally be noted as sunken cheeks and flat buttocks, with wrinkled or loose skin indicative of loss of subcutaneous fat stores. There may be direct evidence of a reduced metabolic rate. The patient will often be mentally slowed.
Fat malabsorption
Failure to digest or absorb fats results in a variety of clinical symptoms and laboratory abnormalities. These manifestations are the result of both fat malabsorption per se and a deficiency of the fat-soluble vitamins. In general, loss of fat in the stool deprives the body of calories and contributes to weight loss and malnutrition.
Failure to absorb the fat-soluble vitamins A, D, E and K also results in a variety of symptoms. Vitamin K deficiency presents as subcutaneous, urinary, nasal, vaginal and gastrointestinal bleeding. Deficiencies in factors II, VII, IX and X produce defective coagulation. Vitamin A deficiency results in follicular hyperkeratosis. Vitamin E deficiency is destructive to the central nervous system. Malabsorption of vitamin D causes rickets, osteopenia and osteoporosis.
Protein malabsorption
Severe loss of body protein may occur before the development of laboratory abnormalities. Clinically, protein deficiency results in edema and diminished muscle mass. Since the immune system is dependent upon adequate proteins, protein deficiency can manifest as recurrent or severe infections. Protein deficiency in children results in growth retardation, mental apathy and irritability, weakness and muscle atrophy, edema, hair loss, deformity of skeletal bone, anorexia, vomiting and diarrhea. Protein-calorie malnutrition is known as marasmus, whereas protein malnutrition by itself is known as kwashiorkor.
Protein/Energy Malnutrition
Attempts have been made to classify malnutrition into a predominantly protein-depleted (i.e., kwashiorkor) or calorie- (energy-) starved (i.e., marasmus) state. In kwashiorkor, the subject ingests a moderate number of calories, usually as complex carbohydrate (e.g., rice), but very little protein. The liver is therefore supplied with inadequate amino acids. The liver becomes fatty and enlarged. Furthermore, other proteins, including albumin, are inadequately produced by the liver in kwashiorkor, and serum albumin falls, with resulting peripheral edema. With marasmus the subject takes inadequate amounts of protein and calories. The low caloric intake means that only small amounts of carbohydrate are taken; with adequate delivery of amino acids from muscle to the liver for protein production. Fatty liver does not occur, and serum albumin levels tend to be normal, with no peripheral edema. Often patients fall between these two extremes of nutritional states, but there are examples of kwashiorkor and marasmus in Western
14 clinical practice. Anorexia nervosa is a classic example of marasmus. Marked muscle wasting and loss of subcutaneous tissue (adipose tissue) occur with normal-sized nonfatty livers and no peripheral edema. In contrast, the intensive care unit patient who has received intravenous dextrose (glucose) without amino acids for a prolonged period will often show a fatty liver and marked hypoalbuminemia (low albumin levels) and edema.
Clinical features of protein-energy malnutrition vary depending on the severity and duration of nutrient deficiency, age at onset and the presence or absence of other contributing or conditioning factors. With minimal deficiency, abnormalities may be subtle - particularly in adults, in whom there are no growth requirements. In these patients muscle wasting and loss of subcutaneous fat may be present. Weakness and minimal changes in psychomotor function may develop. Nontender parotid enlargement (glands in the face and neck) may occur, sometimes bilaterally. Patchy brown pigmentation, particularly over the malar eminences of the face, may occur. A lackluster appearance with thinning and increased shedding of hair from the sides of the head, particularly on combing or brushing, may develop. Bradycardia may occur. Variable degrees of hepatomegaly may result, sometimes with steatosis. In patients with protein- energy malnutrition following jejunoileal bypass a wide spectrum of histopathologic change has been observed, similar to findings frequently associated with alcoholic liver disease.
In adults with severe protein-energy malnutrition and in growing children, clinical features may be even more significant. Muscle wasting, subcutaneous fat loss, dependent edema and weight loss may be marked. Severe mental apathy and reduced physical activity may occur. Abnormalities in the hair, particularly of children, may be striking. Severe dyspigmentation may develop, especially distally; rarely, alternating strands of light and dark hair are observed. Hair may be removed without pain. Nails may become brittle, with horizontal grooves. An asymmetrical confluent pattern of skin hyperpigmentation may be seen, particularly over perineal and exposed areas, such as the face. Extensive desquamation may occur, leaving depigmented areas of superficial ulcers, particularly on the buttocks and backs of the thighs. Gastrointestinal symptoms are common but variable. These include marked constipation, diarrhea, anorexia or hyperphagia, nausea, vomiting and dehydration. Laboratory features are also variable. Serum proteins may be substantially reduced, including serum albumin and some higher-molecular-weight transfer proteins, such as transferrin, ceruloplasmin, lipoproteins, thyroxin and cortisol binding proteins. Serum amino acid analysis may show a decrease in essential amino acids (i.e., leucine, isoleucine, valine, methionine), and either normal or depressed levels of nonessentials (i.e., glycine, serine, glutamine). The urinary excretion of urea, creatinine and hydroxyproline may decrease. Severe electrolyte abnormalities develop, although serum levels may be normal.
Symptoms of Iron deficiency
Anemia
15 Sometimes accompanying iron deficiency and subsequent anemia may be symptoms of pica and dysphagia.
Pica originally referred to the eating of clay or soil; however the commonest “Pica” in North America is the eating of ice.
Dysphagia: sores on the tongue and esophagus and/or reddened lips with sores. Weakness, fatigue, and edema also can occur. Physical examination often reveals pallor, and brittle, flat or spoon-shaped fingernails.
Calcium, Vitamin D and Magnesium malabsorption
May lead to bone pain, fractures, paresthesias, tetany, Chvostek’s sign and Trousseau’s sign. Vitamin D deficiency principally affects the spine, rib cage and long bones with or without fractures, and may cause extreme pain, particularly in the spine, pelvis and leg bones. Insufficient magnesium may cause seizures and symptoms identical to those of insufficient calcium.
Malabsorption of B-12
The daily requirement for Vitamin B-12 (cobalamin) is 1 mg. The human liver can store approximately 5 mg of B-12 (cobalamin). These large stores account for the delay of several years in the clinical appearance of deficiency after B-12 (cobalamin) malabsorption begins.
Electrolyte and water absorption
Although water and electrolytes are also absorbed in the large intestine, much of this absorbtion and secretion is done in the small intestine. Since the gastric bypass patient has much of the small intestine bypassed, this overall balance is shifted toward secretion. Therefore, dehydration is more prominent in gastric bypass patients, requiring a higher than average intake of water per day.
Short Bowel Syndrome
The severity of symptoms following resections of large segments of the small bowel relates to the extent of the resection, to the specific level of the resected small bowel and to the reason for which the resection was undertaken. The level of resection is important because absorption of nutrients is most effective in the proximal small bowel (iron, folate and calcium). This section is bypassed in gastric bypass surgery. Resection of up to 40% of the intestine is usually tolerated provided the duodenum
16 (bypassed in gastric bypass) and proximal jejunum (bypassed in gastric bypass) and distal half of the ileum and ileocecal valve are spared. Resection of 50% of the small intestine results in significant malabsorption, and resection of 70% or more of the small intestine will result in severe malnutrition sufficient to cause death unless the patient's malnutrition is aggressively treated. Where, exactly, each gastric bypass patients fits in this, is dependant on the type of surgery, and the length of bypass, but all result in a significant amount of malabsorption.
Postgastrectomy Malabsorption
Postgastrectomy malabsorption frequently follows gastric surgery. The small size of the gastric remnant (pouch) causes inadequate mixing of food with digestive juices. With the loss of the pylorus, there may be rapid gastric emptying, poor mixing of bile and pancreatic secretions, and rapid transit down the small intestine. Incoordinated secretion and poor mixing of bile and pancreatic juice leads to fat maldigestion. Gastric surgery that allows food to enter into the upper small intestine without dilution and with minimal digestion may "unmask" mild and subclinical celiac disease, lactase deficiency or pancreatic insufficiency.
17 What kind of protein is the best?
BIOAVAILABILITY OF PROTEIN TYPES
The higher on the list, the better. The numbers are the BV. (Biologic value). This is only how easily the (normal) body can absorb them, not the protein grams in each one. The last few need to be blended to make a complete protein. And remember….gastric bypass patients don’t absorb nutrients from food protein very well.
Protein Source BV Whey Protein Isolate Blends 100-159 Whey Concentrate (Lactalbumin) 104 Whole Egg 100 Cow's Milk 91 Egg White (Albumin) 88 Fish 83 Beef 80 Chicken 79 Casein (a protein from milk) 77 Rice 74 Soy 59 Wheat 54 Beans 49 Peanuts 43
So, because we(gastric bypass patients) don't have a stomach and the stomach acids, etc, anymore, we don't process the undigested proteins properly and malabsorb most of them. The same is for the normal food we eat. We don't absorb most of it. We, therefore, need the more highly absorbed, pre-digested protein supplements.....whey which is pre-digested (aka hydrolized)...in order to get the proper nutrients our bodies need and are no longer able to get from food.
So, whereas whole egg, cow's milk, egg white are near the top of the list of bioavailability for "normal" people, they are not pre-digested (hydrolized), so for us, they are not as high on the list as pre-digested whey protein. Our bioavailability list would be quite different from the "normal" person's list.
So, make sure your protein powder or drink states that it is pre-digested or hydrolized. And the best kind of protein would be a whey blend protein. Second best would be a 100% whey protein. Isolates, though good for a quick acting pick-me-up, are not sufficient alone for the gastric bypass patients on-going maintenance requirements.
18 Whey Protein Isolate Whey Protein Protein Blends (Mixed (WPI) Concentrate (WPC) Protein Sources) **best Whey Protein Isolate powders These products contain Whey Many researchers believe that go through the best filtering Protein Concentrate (generally quick-absorbing proteins like around 75% to 80% protein) or may process to remove fat and also have a small amount of Whey Whey Protein are best carbohydrates. In general, these Protein Isolate blended in. None of immediately after a workout and powders will contain a higher these products contains more Whey first thing in the morning when percentage of protein compared Protein Isolate than Concentrate. your body has extra protein to Whey Protein Concentrate - Whey Protein Concentrate is much needs, but a mixture of various more economical than the Isolates generally around 90% protein. because the process of removing slower-absorbing proteins are These are best utilized most of the carbs and fat is better at other times of the day to immediately after a workout relatively inexpensive compared to spread out the absorption for and first thing in the morning getting the maximal amounts out to several hours. This helps keep when fast-acting protein is isolate the protein. amino acids in the bloodstream needed most. for use by muscle tissue as Designer Protein GEN HumanoPro needed. Below are products Champion Pure Whey Stack containing blends of various Nature's Best IsoPure Protein HDT 5 Plus 1 protein sources - including whey Prolab Whey Protein Isolate Optimum Nutrition 100% Whey protein. These are recommended Worldwide Extreme Pure Protein for general use throughout the day and at bed time.
Champion Nutrition Pro-Score 100 HDT Pro Blend 55 MET-Rx Protein Plus Labrada ProV60 Optimum Nutrition Pro Complex The Biological Value, or BV, of a protein is an indicator of the quality of the protein. It is a measure of a protein's ability to be used by the body (or its bioavailability). It is a percentage (though the scale is skewed resulting in some BV's of greater than 100) of the absorbed protein that your body actually uses. Biological Values are indicators of which proteins are best at aiding nitrogen retention in muscles to help them maintain or grow.
Many of the whey protein powder manufacturers claim that their products have BV values well above regular whey protein by various techniques such as ion-exchange processing, hydrolization, and adding other ingredients such as specific amounts of limiting essential amino acids.
Hydrolyzation is a process breaking large peptides into smaller ones. It is sometimes referred to as "pre- digested".
Regular undigested whey will be broken down into di- and tri-peptides via enzymes in the gut (which gastric bypass patients no longer have). This process takes a while, even in the non-gastric bypass person. Hydrolyzation is useful when protein delivery is needed very quickly so the body doesn't have to require the time and enzymes doing it. The benefit is of having a quickly absorbed protein to ensure muscle tissue is flooded with nutrients in a timely manner.
19 If I drink protein shakes and eat too, won’t I gain weight from the added calories?
Eating a low calorie diet actually slows down your metabolism.
Diets containing more protein can reduce the drop in metabolic rate seen with low calorie diets. To lose fat, you need to cut down on calories, to consume less energy than you expend. But. Here is the problem. Your body responds to this drop in food intake by slowing your metabolic rate, to keep you alive, which makes fat loss increasingly difficult.
Our ancestors had to deal with large variations in the availability of food. Those who survived were the ones whose bodies could adjust to this fluctuation in food availability. Those whose bodies couldn’t adjust, died.
The result?
Our bodies want to hold on to our stores of energy for survival. It thus preserves fat by lowering the metabolic rate whenever food intake drops.
High protein diets reduce the drop in metabolic rate, and also lead to a greater feeling of fullness.
Dr Scott Connelly1 writes in, “Body Rx: pages 18-19….”Why do MASS protein? To escape fat- storage mode, you have to eat more protein. If you want to shut down your metabolism and stay in fat-storage mode permanently, stay on the standard diet prescription- the high-carb, low-protein, low-calorie, low-fat diet. Protein is the key metabolic currency of the body. Your body was designed to run on it. Protein molecules drive all the chemical reactions involved in the breakdown and absorption of food, including carbohydrates and fat. In other words, protein drives virtually all aspects of metabolism. Many studies, including some of my own, show that simply adding protein to your diet turns on your fat-burning/muscle-building switch, even if you make no other lifestyle changes. When I gave one group of body builders extra protein along with their normal diet, they gained two times as much muscle mass as a second group of bodybuilders doing exactly the same workout and eating the same diet but without the extra protein. When you’re stuck in fat-storage mode, you need a powerful protein boost to jump-start your metabolism back into fat-burning mode. In most cases, you cannot easily get enough protein from food alone to do the job. To fill the protein gap, in addition to increasing protein consumption through food, I recommend a daily high- potency protein powder. It is a simple, safe, efficient way to repair your metabolism and build a lean, shapely body.”
1 Dr Scott Connelly has devoted his life to the science of nutrition and fitness, and is considered around the world as a leading expert in the field of human nutrition and metabolism. A summa cum laude graduate in neuro-physiology from Boston University, Dr Connelly has distinguished his career in anesthesiology, internal medicine, intensive care and cardiovascular medicine. During his internship and residency at Harvard Medical School’s prestigious Massachusetts General Hospital, Dr. Connelly began working with critically ill intensive care patients. In order to help his patients maintain their health, he began researching and formulating products to help prevent the loss of muscle mass. What he learned about the effects of nutrients and exercise on human metabolism, body composition, disease prevention and immune system function.
20 Muscle uses more calories to maintain itself than fat. Peole who are more muscular (and have a lower percentage of body fat) are said to have a higher metabolism than others that are less muscular.
Symptoms of slowed metabolism
Fatigue, feeling cold, dry skin, constipation, a slow pulse and low blood pressure. These symptoms could be the result of a medical condition rather than low metabolism – MAKE SURE YOU SEE YOUR DOCTOR to rule out any type of medical problem.
How can I increase my metabolism?
Begin to exercise and stop dieting. You can increase your muscle mass by doing some type of resistance work (i.e. lifting weights, using exertubes, rubberbands, dynabands, hand weights, etc…). You can also decrease your level of body fat by doing some type of aerobic exercise at least 3 days a week for longer than 20 minutes. This is exercise such as walking, jogging, step aerobics, hi/low aerobics, biking, swimming, etc, that will increase your heartrate and keep it there for the duration of the exercise session. You also need to eat! Do not diet, just watch the types of foods you eat, and drink your protein!!
How can I lower my metabolism (but why would you want to)?
If you eat a very low calorie diet, your metabolism will slow down in order for your body to survive (your body thinks it is starving).
Vitamins
Vitamins are substances the body needs in small amounts to support most body functions and prevent disease. Vitamins play a role in energy production and growth; and work with each other and with other nutrients to keep our hearts pumping, our bones and immune system strong, our digestive system moving and our skin and hair healthy.
21 Nutrient Absorption in the Gastrointestinal Tract
Darkened area indicates part of digestive tract that is bypassed in the RNY gastric bypass patient.
22 Vitamin Regimen - BASIC plan (Add to this based on your particular labwork)
30g of protein supplement, made in water, 3 to 6 times per day, no milk, no sugar.
AND 64 oz of water - minimum
This vitamin schedule is just a suggestion. You can take them any way you wish as long as you follow the rules listed below. Since the rules can be complicated, many people wanted a good place to start. That is why this schedule was created.
I find it a good idea to put the vitamins all out in a pill case for the week. Then I can see what I have taken, or if I have missed something. My pill case has sections for 7 days....4 sections for each day......
AM: 2 iron (25 mg each) Ferrous FUMERATE, Carbonyl iron, or elemental iron Vit C (1000mg) ascorbic acid with rosehips
mid-day: Calcium CITRATE (500mg) with Vit D and MAgnesium (250mg) Vit E (400IU E a-alpha tocopheryl sucinate) 1 multi-vitamin (equal to Centrum)
evening: Calcium CITRATE (500mg) with Vit D and MAgnesium (250mg) Zinc (50mg zinc gluconate, chelated) 1 Vit A&D (10,000 IU Vit A & 400 IU Vit D3)
bedtime: Calcium CITRATE (500mg) with Vit D and MAgnesium (250mg) 1 multi-vitamin (equal to Centrum)
1 sublingual B-12 daily (cobalamin concentrate) or monthly B-12 injection
B Complex tabs daily, are also suggested, especially for energy. ------* multi-vitamins: (equal to Centrum) vit A 5000 IU, 25% as beta-carotene, vit C 120mg, vit D 400IU, vit E 60IU, thiamin (B1) 1.5mg, Riboflavin (B2) 1.7mg, Niacin (B3) 20mg, Riboflavin (B6) 2mg, Folate (folic acid) 400mcg, B12 6mcg, biotin 30 mcg, pantothenic acid 10mcg, calcium 162mg, iron 18mg (ferrous
23 fumarate), phosphorus 100mg, iodine 150mg, magnesium 100mg, zinc 22.5mg, copper 3mg, selenium 45mcg, manganese 2.5mg, chromium 120mcg, molybdenum 75mcg, chloride 72mg, potassium 80mg, silicon 2mg, boron 150mcg, tin 10mcg, vanadium 10mcg, nickel 5mcg, lutein 275mcg ------Some rules for vitamin supplements:
IRON...... Take iron (ferrous FUMERATE only, NOT ferrous SULFATE!) Iron is NOT a friendly vitamin. Take iron ALONE, NOT with other meds, juice, dairy products, calcium, etc....ALONE (ok with Vit C only), or it will be useless. We have a VERY hard time absorbing iron, so this is very important!
CALCIUM...... Take Calcium CITRATE, NOT Calcium Carbonate. Not Tums (This is carbonate). We do not absorb the carbonate! There are some other types we do absorb, one is elemental calcium. Remember....do not take it with iron. Calcium also needs Vit D and Magnesium to work. If your calcium does not have these in the tablet, then you must add Magnesium and more Vit D also.
Multi-vitamins..... You should use a multi vitamin that is equivalent to Centrum (See above for a description*). You will need to take 2 of these instead of 1 as we only absorb about 50% at most.
Vitamins A,D,E and zinc and C (and any others you may add)...... use only dry tablets....we do not absorb anything in an oil type gel cap, or ones that are enteric coated, or time-release versions.
B-12 injections....you can get a perscription from your primary doctor for a vial of B-12 that will give you about 30 injections. The B-12 is quite inexpensive. I paid under $4 for the vial, and that was regular price (less than my copay would have been.) If you don't like injections, you can use the B-12 sublinguals. They melt under your tongue like nitroglycerin tabs for heart patients. You can get them many places, including GNC stores. If you choose the sublinguals, you will need to take them daily, whereas the injections are monthly.
Remember, these are the BASICS. If your labwork shows drops in any areas, then these amounts will have to be adjusted.
Some additions..... Problems with hair loss or brittle nails....add Biotin Problems absorbing Calcium...... add Boron Problems absorbing iron...... add Copper
24 LAB TESTS Regularly - for gastric bypass patients*
*Keep track of any levels which are declining from one set of tests to the next, even if not yet in the low range. Make any corrections necessary in your diet before the levels get too low.
* In addition, it is recommended that you get a yearly Dexa bone scan because of the heightened possibility of osteoporosis after gastric bypass surgery.
COMPREHENSIVE METABOLIC PROFILE (sodium, potassium, chloride, glucose, BUN, creatinine, calcium, total protein, albumin, total bilirubin,alkaline phosphatase, aspartate aminotransferase) (Nc,K,C1,CO2,Glu,BUN,Cr,Ca,TP,Alb,Tbili,AP,AST,ALT)
LIPID PROFILE (cholesterol, HDL, LDL, triglycerides, chol/HDL ratio) (Fasting specimen) , Tchol,Trig,HDL,Calc,LDL)
ALT (SPGT)
GGT
LDH
PHOSPHORUS – INORGANIC
URIC ACID
CBC (HEMOGRAM/PLT/DIFF)
B-12 & FOLATE
IRON, TIBC, % SAT
FERRITIN
VITAMIN A & D (25-hydroxy)
THYROID PANEL (T3U, T4, FTI, TSH) Diagnosis: 579.3 post-surgical malabsorption 269.2 hypovitaminosis ZINC 244.9 hypothyroidism 579.3 short bowel syndrome MAGNESIUM 268 vitamin D deficiency 268.2 metabolic bone disease SERUM INTACT PTH 250.0 401.9 PARATHYROID
25 Vitamins: Sources, Amounts and Important Issues
The Food and Nutrition Board of the National Academy of Sciences is the governing body in charge of setting the minimum vitamin levels in order to prevent deficiencies in healthy adults also known as the RDA (recommended daily amounts).
We now know that vitamins are important for maintaining health and preventing disease. No one knows what the RDA is for a gastric bypass patient due to altered anatomy and a low calorie post-operative diet.
We have seen vitamin deficiencies before surgery despite adequate calorie intake but likely due to poor eating habits. For bypass patients, in order to maintain good nutritional status, we have learned from measuring blood levels that a vitamin supplement that exceeds the RDA can provide adequate serum levels.
Vitamin A Vitamin A is a fat-soluble vitamin also known as retinol (fat soluble-animal source) and beta-carotene (water soluble-plant source). It functions in the body; to aid in tissue growth and repair; to improve and maintain normal vision, to maintain healthy skin and mucous membranes, and to fight against infection and boost immunity. If you are deficient in vitamin A possible symptoms could include night blindness, skin type eczema, weight loss, poor bone growth and diarrhea. Toxicity is rare, but if taken in excess, you could experience headaches, hair loss and have anorexia. Common food sources of vitamin A: cod liver oil, beef, liver, eggs, any dark green, red, or orange vegetables like sweet potatoes, pumpkins, broccoli and apricots. For Bypass Patients it is Important to Know Alcohol can decrease vitamin A stores. Drugs that affect the liver such as steroids and Dilantin may effect vitamin A stores. Low vitamin A levels when protein intake is low can correlate with poor nutritional status. Vitamin A stores can be maintained within normal limits if a vitamin supplement is taken. Some deficiencies have been seen if there is excessive fatty stools or the vitamins aren’t taken. Vitamin A levels can decrease transiently after an operation but return to normal after recovery and supplementation. Vitamin A can be lost from foods during cooking, preparation and storage. Olestra can lower vitamin A levels due to fat malabsorption.
Vitamin B-1 (Thiamin) Needed for: Normal function of the heart, nerves, muscle tissue and digestive system; aids in carbohydrate metabolism and energy production. Its functions include maintaining normal function of the central nervous system, muscles and heart, promoting normal growth and development, and is a co-factor in carbohydrate metabolism (by releasing energy). If you are deficient in vitamin B1, you may experience visual changes, an unsteady gait, a loss of appetite, have fatigue or nausea and perhaps some mental confusion. Ingestion of high amounts of thiamine may cause drowsiness. Common food sources of B1 are liver, beans (like navy and black eye peas), peanuts, raisins and whole grain products. For Bypass Patients it is Important to Know Supplementation is suggested since the post-operative diet is low in calories. Antibiotics and oral contraceptive agents can decrease B1 levels. Avoid over cooking meals, since B1 can be destroyed by heat. Excess alcohol increases risk for B1 deficiency. Large amounts of raw fish and shellfish can increase your risk for a B1 deficiency. Eating an excess amount of refined carbohydrates and not taking your vitamin can potentially lead to a sub-therapeutic
26 level of B1 and produce deficiency symptoms.
Vitamin B-2 (Riboflavin) Needed for: Energy production, immune system function, healthy skin.
Vitamin B-3 (Niacin) Needed for: Energy production, healthy skin, and digestive system function. The body can manufacture niacin from the amino acid tryptophan.
Vitamin B6 (Pyrodoxine) Needed for: Energy production, red blood cell formation, immunity, nervous system and hormone function.
Vitamin B-12 Needed for: Energy production, red blood cell production, utilization of folic acid, nervous system function. Vitamin B12 is also known as cobalamin. Cyanocobalamin is the synthetic form. B12 has many functions with the most important being the nerve function. B12 and folate are metabolically interrelated. B12 converts folate to an active form. B12 is responsible for the manufacturing and normal functioning of red blood cells. It also helps metabolize carbohydrates and fats and synthesize proteins. B12 binds to Intrinsic factor, produced in the stomach. This no longer happens in the pouch which is left after gastric bypass, causing B-12 deficiency in many patients. Deficiency symptoms can be manifested as anemia, nerve damage, fatigue, dementia and even coronary artery disease. There have been no reported toxic effects with high does of B12. Vitamin B12 for Bypass Patients Heat and moisture may change the action of the vitamin. Store in a cool dry place. High intake of vitamin B6 reduces B12 absorption. Smoking decreases vitamin B12 metabolism. For improved absorption, take B12 one hour before meals. Colchicine reduces absorption of B12.
Folic Acid Needed for: Energy production, red blood cell formation and growth. Essential for prevention of certain birth defects.
Pantothenic Acid Needed for: Carbohydrate, fat, energy and protein metabolism.
Biotin Needed for: Energy production, fatty acid synthesis and the breakdown of certain amino acids.
Vitamin C (Ascorbid Acid) Needed for: Normal growth, wound healing, disease and infection resistance, bone and teeth formation, more efficient iron absorption. The best and most common sources of vitamin C are fruits and vegetables. Vitamin C is a water-soluble vitamin, that is important if formation of collagen (a protein that gives structure to bones, cartilage, and muscle). It maintains the capillaries and aids in the absorption of iron. Vitamin C is a known antioxidant that prevents cell damage. Eating a variety of fruits and vegetables ensures appropriate intake of the vitamin. If you are deficient in vitamin C, you may experience muscle weakness, loss of teeth, easy
27 bruising, nosebleeds and frequent infections. Vitamin C assists in calcium absorption and can increase iron absorption. Smoking increases requirements for vitamin C.
Vitamin D
Needed for: Normal growth; healthy bones, teeth and nails; proper absorption of calcium and phosphorus.
Vitamin E (tocopherol) Needed for: Cell membrane integrity and protection.
Folate Folate and Folic Acid are interchangeable terms. Folic acid is the synthetic form of folate, which is found naturally in some foods. Folate is primarily known for preventing neural tube defects, a form of spinal cord deformity in newborns, preventable by taking folate. Folate is essential for the synthesis of RNA and DNA, the genetic material of cells. It plays a vital role in growth and development of cells. Folic acid is necessary for aiding in protein metabolism. It also may be protective against heart disease by lowering homocysteine levels. Folic acid is absorbed from the small intestine. Of all vitamins, a folate deficiency is most common due to a diet poor in vegetables, primarily dark green leafy vegetables, increased alcohol consumption, and also contributing is folate increased sensitivity to heat and light. Symptoms of folate deficiency include loss of appetite, inflamed tongue and diarrhea. A folate acid deficiency can damage the lining of the gut and lead to further malnutrition. Folate for Bypass Patients NSAIDS (Motrin, Advil and Aleve) and anticonvulsants elevate folate requirements. Excess alcohol intake can lead to a deficiency. Of vitamins are not taken daily and increased risk for a deficiency exists. Taking additional B vitamins in a daily supplement form rather than through food only ensures proper micronutrient nutritional status. If you are of childbearing age, please take a folic acid supplement to prevent neutral tube defect. Prenatal vitamins contain twice the RDA for folate.
Vitamin K Needed for: Production of proteins required for normal blood clotting.
Note: In addition to their other roles, vitamins C, E and beta-carotene (which the body converts into vitamin A) are known as "antioxidants." Certain minerals and other substances also act as antioxidants. Antioxidants can offset the damage caused by free radicals, the unstable, highly reactive molecules formed during the metabolism of glucose and fatty acids to provide energy. Free radicals are also produced in the body by pollutants, ultraviolet light from the sun and drinking alcohol. Free radicals react with and damage many components of tissues, including cellular DNA, or genetic material. Damage from free radicals may lead to conditions such as cataracts, cancer, heart disease and even aging.
28 Minerals
The minerals we need in our body are those found in rocks, metals, soil and water, though they may be in slightly different forms. While each mineral plays a unique role, collectively they support the body's enzyme systems and keep blood and other body fluids balanced and healthy. Minerals, the major components of bones, also help regulate blood pressure and heart muscle contraction, heal wounds and conduct nerve impulses. The minerals needed in relatively large amounts are: calcium, phosphorus, magnesium, sodium, potassium, chloride and sulfur. Other minerals needed in smaller amounts, called "trace elements," consist of iron, copper, fluorine, iodine, selenium, zinc, chromium, cobalt, manganese and molybdenum. Although the body can't produce any minerals of its own, minerals are found in a large variety of fruits, vegetables, beans and grains.
Calcium Needed for: Healthy bones, nails, muscle tissue; assists in blood clotting and heart and nerve functions. Chromium Needed for: Normal release of energy from glucose. Copper Needed for: Enzyme reactions, iron metabolism Fluoride Needed for: Healthy bones and teeth that are resistant to decay. Iodine Needed for: Regulation of body temperature, thyroid hormone synthesis, metabolic rate, reproduction, growth and nerve and muscle function. Iron Needed for: Formation of healthy red blood cells and prevention of anemia; helps carry oxygen to cells. The recommended iron intake is higher for women between the ages of 11 and 50 to compensate for iron loss during menstruation. Magnesium Needed for: Energy production, normal heart and nerve function and prevention of muscle cramps Phosphorus Needed for: Growth; maintain bone density; assists in energy production; and regulates blood chemistry Potassium Needed for: Regulation and balance of body fluids, promotes normal heart rhythm; prevents muscle cramping Selenium Needed for: Antioxidant properties protect vitamin E and polyunsaturated fats in the body Sodium Needed for: Regulation of body fluids and maintenance of acid-base balance; aids in nerve transmission and muscle contraction Zinc Needed for: Normal appetite and taste, wound healing, healthy skin and normal growth
The Bottom Line: Vitamin and mineral supplementation is a life long commitment for gastric bypass patients. Knowledge is your best armor. Eating a balanced diet and taking your supplements provides the best route to fulfilling your nutritional requirements.
29 Did you know that dietary supplements are taken by more than half of the USA adult population? Sales are going up but which supplements are best and more importantly, are they safe for us to take? The Federal Trade Commission (FTC) regulates the advertising of supplements. The Food and Drug Administration (FDA) has set up DSHA or Dietary Supplements Health and Education Act along with the National Institute of Health (NIH) a framework for supplement regulation and research. Additionally, there is an independently appointed commission who provides reports for the claims for the use of supplements (i.e. vitamins, minerals, herbs, etc.). Dietary supplements have to meet certain criteria. Since March of 1999, manufacturers are required to provide an informative dietary supplement panel on the label, which indicates the following information.
A statement of identity (i.e. Vitamin C
Net quantity of contents (i.e. 90 tablets)
Structure-function claim like “Calcium builds strong bones” and the statement “This statement has been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.”
Directions for use
Supplement fact panel (lists serving size, amount and active ingredients)
Other ingredients in order of predominance
Name and place of business of manufacturer, packer or distributor along with the address to write for more product information
What are vitamins? Vitamins are nutrients that are essential for maintenance of normal metabolic functions. Vitamins are supplements both synthetic and natural and come in many forms. The water-soluble vitamins are Thiamine (B1), Riboflavin (B2), Niacin (B3), Panethanic Acid (B5), Pyridoxine (B6), Biotin, Cobalamin (B12), Folic Acid, and ascorbic acid (Vitamin C). The fat-soluble vitamins are vitamin A, D, E and K.
The water-soluble vitamins are not significantly stored by the body and need to be replaced daily by food or supplement to maintain adequate levels. These vitamins can be rapidly depleted in conditions interfering with intake or absorption. The fat-soluble vitamins are better stored in the body, and if not excreted, toxic levels could occur. For the gastric bypass patient, who malabsorbs fat, fat-soluble vitamins cannot be digested properly, and are excreted without doing their job. Vitamins in dry form only are therefore suggested. If your vitamins are in an oil base, they are doing you no good.
30 References
Harvard School of Public Health Protein:Nutrition Source
USDA Nutrient Database for Standard Reference, Release 14. US Department of Agriculture. accessed on 18 July 2002.
National Science Teachers Association, SCILinks
University of Michigan, Anatomy & Physiology Gastrointestinal (GI) System
InteliHealth: Harvard Medical School’s Consumer Health Information
Beyond Change, Sally Myers, RD
First Principles of Gastroenterology: The Basis of Disease and an Approach to Management, Thomson & Shaffer, Chapter 7 – Section 9
Journal References to Protein Malnutrition following Gastric Bypass:
1. Hsia AW, Hattab EM, Katz JS: Malnutrition-induced myopathy following Roux-en-Y gastric bypass. Muscle Nerve (United States), Dec 2001, 24(12) p1692-4
2. Fobi MA, Lee H, Igwe D, et al.: Revision of failed gastric bypass to distal Roux-en-Y gastric bypass: a review of 65 cases. Obes Surg (Canada), Apr 2001, 11(2) p190-5
3. Kushner R: Managing the obese patient after bariatric surgery: a case report of severe malnutrition and review of the literature. JPEN J Parenter Enteral Nutr (United States), Mar-Apr 2000, 24(2) p126-32
4. Brolin RE, La Marca LB, Kenler HA, et al.: Malabsorptive gastric bypass in patients with Superobesity. J Gastrointest Surg (United States), Mar-Apr 2002, 6(2) p195-203; discussion 204- 5
5. Fobi M, Lee H, Igwe D, et al.: Band erosion: incidence, etiology, management and outcome after banded vertical gastric bypass. Obes Surg (Canada), Dec 2001, 11(6) p699-707
6. Gagner M, Gentileschi P, de Csepel J, et al.:Laparoscopic reoperative bariatric surgery: experience from 27 consecutive patients. Obes Surg (Canada), Apr 2002, 12(2) p254-60
7. Sugerman HJ: Bariatric surgery for severe obesity. J Assoc Acad Minor Phys (United States), Jul 2001, 12(3) p129-36
8. Sugerman HJ, Kellum JM, De Maria EJ: Conversion of Proximal to Distal Gastric Bypass for Failed Gastric Bypass for Superobesity J Gastrointest Surg (United States), Nov 1997, 1(6) p517-525
31 9. Sugerman HJ, Starkey JV, Birkenhauer R: A randomized prospective trail of gastric bypass versus vertical banded gastroplasty for morbid obesity and their effects on sweets versus non- sweets eaters. Ann Surg 1987; 205:613-624
10. Sugarman, Harvey J.: Highlights From the Annual Scientific Assembly: Mechanisms to Stop the Epidemic of Obesity: Surgical Therapy for Obesity South Med J 95(6):657-659, 2002.
11. Mason EE: Starvation injury after gastric reduction for obesity. World J Surg (United States), Sep 1998, 22(9) p1002-7
12. Fox SR, Fox KS, Oh KH:The Gastric Bypass for Failed Bariatric Surgical Procedures Obes Surg (England), Apr 1996, 6(2) p145-150
13. Adami GF, Summa M, Castagnola M, et al.: Malnutrition, nutritional support and total body composition. Ital J Surg Sci (Italy), 1988, 18(1) p63-7
14. Scopinaro N, Adami GF, Marinari GM, et al.: Biliopancreatic diversion. World J Surg (United States), Sep 1998, 22(9) p936-46
15. Scopinaro N; Gianetta E; Adami GF, et al.: Biliopancreatic diversion for obesity at eighteen years. Surgery 1996 Mar;119(3):261-8
16. Forestieri P; De Luca M; Formato A,et al.:Restrictive versus malabsorptive procedures: criteria for patient selection. Obes Surg 1999 Feb;9(1):48-50
17. Byrne TK: Complications of surgery for obesity. Surg Clin North Am 2001 Oct;81(5):1181- 93, vii-viii
18. Breaux CW: Obesity Surgery in Children Obes Surg 1995 Aug;5(3):279-284
32 Glossary
STEATORRHEA - Fecal matter that is frothy, foul-smelling and floats because of a high fat content. A finding that is typical in malabsorption syndromes.
DYSPHAGIA – means difficulty in swallowing. Some patients describe food sticking in the throat page 8 or retrosternally.
Dysphagia can also occur with motor disorders of the esophagus. These conditions include esophageal spasm and achalasia. With motor disorders of the esophagus, the dysphagia may be for both solids and liquids. The dysphagia is intermittent and may have a long history. Sometimes with esophageal spasm the dysphagia may be accompanied by pain (odynophagia), especially with extremely cold or hot liquids. These patients are usually able to wash down impacted particles of food, whereas patients with a mechanical cause (such as a stricture) may need to regurgitate impacted particles of food to obtain relief.
A common cause of intermittent dysphagia is a mucosal ring at the gastroesophageal junction (lower esophageal or Schatzki’s ring). On occasion when a relatively large bolus of food is swallowed the ring can cause mechanical obstruction, producing a dramatic onset of acute dysphagia (sometimes associated with pain). Often such patients will have to leave the table and regurgitate. Patients with a Schatzki’s ring usually have symptoms for many years before they seek medical attention.
A rare cause of upper esophageal dysphagia is the Paterson-Kelly syndrome or Plummer-Vinson syndrome. Here, a chronic iron deficiency anemia is associated with narrowing of the upper esophagus due to a web.
BORBORYGMI - the noises generated as air and fluid gurgle through the gut.
AEROPHAGIA - Adolescents love to shock their elders with voluntary belching. More commonly, aerophagia is an unwanted habit in those who repeatedly belch in response to other gut symptoms.
PICA - Originally referred to the eating of clay or soil; however the commonest “Pica” in North America is the eating of ice.
DYSPHAGIA - Sores on the tongue and esophagus and/or reddened lips with sores. Weakness, fatigue, and edema also can occur. Physical examination often reveals pallor, and brittle, flat or spoon- shaped fingernails.
33