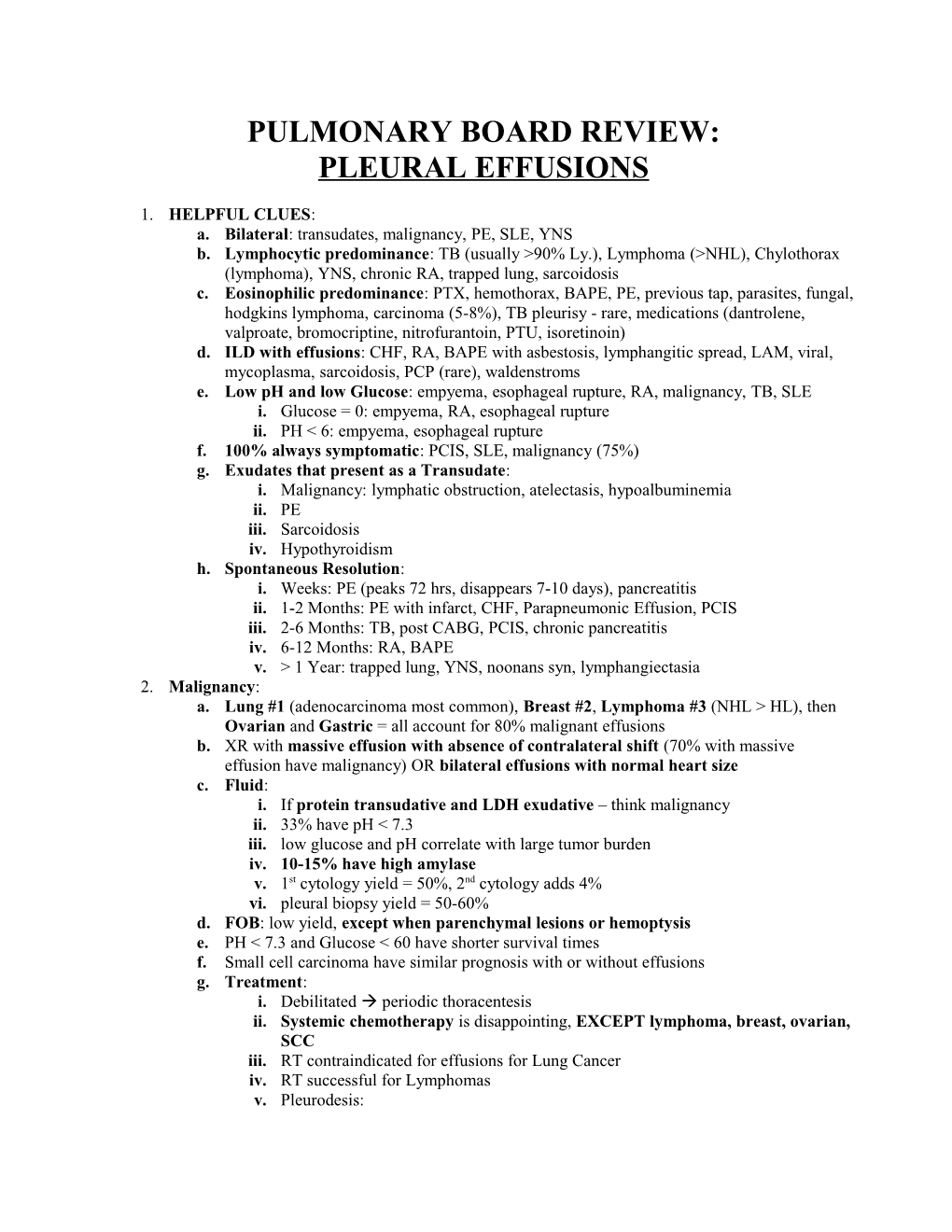
PULMONARY BOARD REVIEW: PLEURAL EFFUSIONS
1. HELPFUL CLUES: a. Bilateral: transudates, malignancy, PE, SLE, YNS b. Lymphocytic predominance: TB (usually >90% Ly.), Lymphoma (>NHL), Chylothorax (lymphoma), YNS, chronic RA, trapped lung, sarcoidosis c. Eosinophilic predominance: PTX, hemothorax, BAPE, PE, previous tap, parasites, fungal, hodgkins lymphoma, carcinoma (5-8%), TB pleurisy - rare, medications (dantrolene, valproate, bromocriptine, nitrofurantoin, PTU, isoretinoin) d. ILD with effusions: CHF, RA, BAPE with asbestosis, lymphangitic spread, LAM, viral, mycoplasma, sarcoidosis, PCP (rare), waldenstroms e. Low pH and low Glucose: empyema, esophageal rupture, RA, malignancy, TB, SLE i. Glucose = 0: empyema, RA, esophageal rupture ii. PH < 6: empyema, esophageal rupture f. 100% always symptomatic: PCIS, SLE, malignancy (75%) g. Exudates that present as a Transudate: i. Malignancy: lymphatic obstruction, atelectasis, hypoalbuminemia ii. PE iii. Sarcoidosis iv. Hypothyroidism h. Spontaneous Resolution: i. Weeks: PE (peaks 72 hrs, disappears 7-10 days), pancreatitis ii. 1-2 Months: PE with infarct, CHF, Parapneumonic Effusion, PCIS iii. 2-6 Months: TB, post CABG, PCIS, chronic pancreatitis iv. 6-12 Months: RA, BAPE v. > 1 Year: trapped lung, YNS, noonans syn, lymphangiectasia 2. Malignancy: a. Lung #1 (adenocarcinoma most common), Breast #2, Lymphoma #3 (NHL > HL), then Ovarian and Gastric = all account for 80% malignant effusions b. XR with massive effusion with absence of contralateral shift (70% with massive effusion have malignancy) OR bilateral effusions with normal heart size c. Fluid: i. If protein transudative and LDH exudative – think malignancy ii. 33% have pH < 7.3 iii. low glucose and pH correlate with large tumor burden iv. 10-15% have high amylase v. 1st cytology yield = 50%, 2nd cytology adds 4% vi. pleural biopsy yield = 50-60% d. FOB: low yield, except when parenchymal lesions or hemoptysis e. PH < 7.3 and Glucose < 60 have shorter survival times f. Small cell carcinoma have similar prognosis with or without effusions g. Treatment: i. Debilitated periodic thoracentesis ii. Systemic chemotherapy is disappointing, EXCEPT lymphoma, breast, ovarian, SCC iii. RT contraindicated for effusions for Lung Cancer iv. RT successful for Lymphomas v. Pleurodesis: 1. NOT if lung cannot fully expand 2. low pH predicts low success (7.15 50%successful pleurodesis) 3. Talc > Bleo, Doxy vi. Pluero-peritoneal shunt: only if intractable and failed all else, OK for chylothorax as it recirculates 3. Pulmonary Embolism: a. Effusions in 40-50% b. Early, unilateral, small (< 1/3 hemithorax) c. Peaks at day 3 then resolves d. If effusion increases in size: think recurrent PE, infected, hemothorax, misdiagnosis e. 20% transudate f. heparin NOT contraindicated 4. TB Pleurisy: a. Unilateral, small b. Setting: post-primary phase (3-6 months after exposure) OR reactivation (anytime) c. Parenchymal disease on CXR in 33% d. Fluid: i. 10% sero-sanguinous (never frankly bloody) ii. 77% protein > 5 iii. classically 90-95% lymphocytes (90% > 60% lymphs) iv. unlikely if > 5% mesos or eosins (unless previous tap or PTX) v. ADA: 1. > 70 in TB, < 40 NOT TB 2. less useful in asians and immunocompromised (falsely lower levels) AND empyema and RA (falsely elevated levels) vi. fluid smear yield = < 5% vii. fluid culture yield = 20-30% viii. pleural biopsy smear yield = 5-18% ix. pleural biopsy culture yield = 60-80% x. without parenchymal infiltrates sputum only positive in 7% xi. > 95% with granuloma on pleura have TB (D/D fungal, sarcoid, tularemia, RA) xii. positive PPD and 90% lymphs and negative work-up: treat as TB! e. Treatment: i. 4 drugs 2 months 2 drugs 4 months ii. moderate symptoms: prednisone 80 mg QOD until acute symptoms subside and then rapidly taper iii. 50% get pleural thickening regardless fluid characteristics iv. NO decortication, NO serial thoracentesis v. If untreated: recurrence rate = 65% over 5 years 5. Parapneumonic Effusions: a. Typical: glu>40 and pH>7.2 and LDH<100 ABx b. Complicated: glu<40 OR pH<7.2 OR LDH>1000 i. Simple: negative GS/Cx ABX, serial taps ii. Complex: positive GS/Cx ABx, small bore CT c. Empyema: pus i. Simple: single pocket ABx, large bore CT if does not drain easily or clinically improve decortication ii. Complex: multi-loculated ABx, VATS decortication 6. Esophageal Perforation: a. Boerhaves vs. iatrogenic (EGD, dilation) b. PTX present in 75% c. 70% on left d. Fluid: PMNs, amylase, low Glu, loe pH, food particles, squamous epi cells e. confirm by gastrograffin f. Treatment: immediate operative intervention, if primary closure within 24 hours then 90% survival 7. Pancreatitis: a. Acute: i. Small, left (60%), high amylase (500-10,000), PMNs predominate ii. pleural fluid:serum amylase ratio >1.0 iii. resolves in 2-3 weeks as inflammation resolves b. Chronic: i. Large, recurrent, unilateral, serous or hemorrhagic ii. Amylase >100,000 iii. Due to pancreatic duct rupture, pseudocyst, or ascites iv. Conservative treatment and if refractory somatostatin, , percutaneous catheter drainage, or surgery 8. Chylothorax: a. Small-large unilateral effusion b. Non-Traumatic Causes (72%): NHL, Retro-peritoneal Carcinoma, LAM, KS, Noonans, Left Subclavian Vein Thrombosis c. Traumatic (28%): surgery d. Fluid: i. > 80% lymphs, glu=serum, pH > 7.4, TGL > 110 ii. TGL 50-110: do lipo-electrophoresis and check chylomicrons e. Treatment: tap for dyspnea i. Reduce chyle formation: increase MC-TGL or TPN ii. Chemical pleurodesis or thoracic duct ligation iii. RT for NHL 9. Rheumatoid Arhtritis: a. Small-moderate, unilateral, 33% with parenchymal disease b. Usually 5-10 years after arthritis (BUT can occur anytime) c. Fluid: i. TRIAD: glu<30, pH=7.0, LDH>1000 ii. Acutely PMNs, chronicly Lymphs iii. Reduced complement, high RF (>1:320) d. Treatment: NSAIDS or Steroids – can develop pleural peel 10. Lupus Pleuritis: a. Small-moderate, bilateral is common, BUT can be anything b. Always symptomatic c. Associated with a flare d. Fluid: PMNs or Monos, Glu<60, ANA >160, LE cells, reduced complement, pleural fluid:serum ration > 1.0 e. Treatment: Steroids, spontaneous resolution does not occur
11. BAPE: a. small, unilateral b. Earliest manifestation of asbestos exposure (within 20 years) c. 50-70% symptomatic d. 20% pleural placques e. Fluid: sero-sanguinous, 25% eosin, glu=serum, pH>7.3 f. Treatment: none, spontaneously resolves 12. Post Cardiac Injury Syndrome: a. Following cardiac surgery or MI b. Immunologic response to cardiac injury Anti-myocardial Ab c. 2-86 days after injury d. left >> bilateral >> right e. Fluid: PMNs early, bloody, pH > 7.3, glu=serum, decreased complement f. Treatment: NSAIDs, Steroids, resolves after 1-3 weeks 13. IMA for CABG: a. Left sided b. Hemorrhagic c. Most resolve over weeks to months, may require CT d. Due to weeping from IMA bed, and accumulation of mediastinal drainage, and atelectasis, and pleurotomy 14. Trapped Lung: a. Small – moderate unilateral effusion b. Lung expansion prevented increase negative intrapleural pressure favors fluid formation in pleural space c. Diagnosis: failure of lung to re-expand on CXR after removal of fluid in absence of bronchial obstruction d. Fluid: Monos, normal Glu, pH > 7.3, borderline trans/exudates e. Treatment: decortication if symptomatic 15. Uremic Pleuritis: a. Small – moderate unilateral, bilateral and massive can occur b. Due to increase pleural permeability from immune complexes? c. On HD for many years, fever, chest pain, cough d. Fluid: serosnaguinous/bloody, lymphocytic predominant, normal Glu, pH>7.3 e. MUST exclude TB pleurisy!!! f. Treatment: HD, spontaneously resolves over weeks 16. Yellow Nail Syndrome: a. TRIAD: yellow nails, lymphedema, respiratory tract disease (recurrent pleural effusions, pneumonias, bronchiectasis, sinusitis) b. Also see chylous ascites and pericardial effusions c. Unilateral or bilateral, small or massive d. Fluid: exudates, protein > 4.0, lymphocytic predominant (~80%), pH>7.4, normal Glu e. Treatment: pleurodesis if symptomatic 17. Others: a. RT: pleuritis, reduced lymphatic drainage due to mediastinal fibrosis b. Hypothyroidism c. Medications d. AIDS