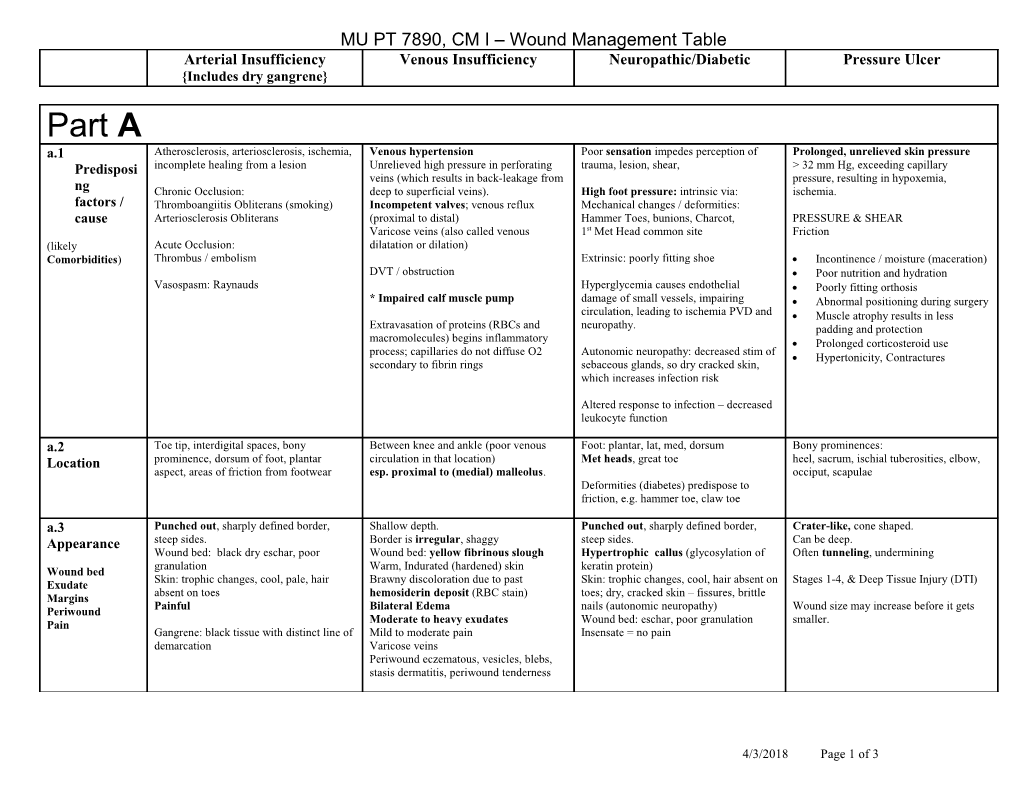
MU PT 7890, CM I – Wound Management Table Arterial Insufficiency Venous Insufficiency Neuropathic/Diabetic Pressure Ulcer {Includes dry gangrene} Part A a.1 Atherosclerosis, arteriosclerosis, ischemia, Venous hypertension Poor sensation impedes perception of Prolonged, unrelieved skin pressure Predisposi incomplete healing from a lesion Unrelieved high pressure in perforating trauma, lesion, shear, > 32 mm Hg, exceeding capillary veins (which results in back-leakage from pressure, resulting in hypoxemia, ng Chronic Occlusion: deep to superficial veins). High foot pressure: intrinsic via: ischemia. factors / Thromboangiitis Obliterans (smoking) Incompetent valves; venous reflux Mechanical changes / deformities: cause Arteriosclerosis Obliterans (proximal to distal) Hammer Toes, bunions, Charcot, PRESSURE & SHEAR Varicose veins (also called venous 1st Met Head common site Friction (likely Acute Occlusion: dilatation or dilation) Comorbidities) Thrombus / embolism Extrinsic: poorly fitting shoe Incontinence / moisture (maceration) DVT / obstruction Poor nutrition and hydration Vasospasm: Raynauds Hyperglycemia causes endothelial Poorly fitting orthosis * Impaired calf muscle pump damage of small vessels, impairing Abnormal positioning during surgery circulation, leading to ischemia PVD and Muscle atrophy results in less Extravasation of proteins (RBCs and neuropathy. padding and protection macromolecules) begins inflammatory Prolonged corticosteroid use process; capillaries do not diffuse O2 Autonomic neuropathy: decreased stim of Hypertonicity, Contractures secondary to fibrin rings sebaceous glands, so dry cracked skin, which increases infection risk
Altered response to infection – decreased leukocyte function a.2 Toe tip, interdigital spaces, bony Between knee and ankle (poor venous Foot: plantar, lat, med, dorsum Bony prominences: Location prominence, dorsum of foot, plantar circulation in that location) Met heads, great toe heel, sacrum, ischial tuberosities, elbow, aspect, areas of friction from footwear esp. proximal to (medial) malleolus. occiput, scapulae Deformities (diabetes) predispose to friction, e.g. hammer toe, claw toe a.3 Punched out, sharply defined border, Shallow depth. Punched out, sharply defined border, Crater-like, cone shaped. Appearance steep sides. Border is irregular, shaggy steep sides. Can be deep. Wound bed: black dry eschar, poor Wound bed: yellow fibrinous slough Hypertrophic callus (glycosylation of Often tunneling, undermining granulation Warm, Indurated (hardened) skin keratin protein) Wound bed Skin: trophic changes, cool, pale, hair Brawny discoloration due to past Skin: trophic changes, cool, hair absent on Stages 1-4, & Deep Tissue Injury (DTI) Exudate absent on toes hemosiderin deposit (RBC stain) toes; dry, cracked skin – fissures, brittle Margins Painful Bilateral Edema nails (autonomic neuropathy) Wound size may increase before it gets Periwound Moderate to heavy exudates Wound bed: eschar, poor granulation smaller. Pain Gangrene: black tissue with distinct line of Mild to moderate pain Insensate = no pain demarcation Varicose veins Periwound eczematous, vesicles, blebs, stasis dermatitis, periwound tenderness
4/3/2018 Page 1 of 3 MU PT 7890, CM I – Wound Management Table Arterial Insufficiency Venous Insufficiency Neuropathic/Diabetic Pressure Ulcer {Includes dry gangrene} a.4 Ability to restore blood flow to area, ie, Must manage edema to heal! Effective diabetic blood sugar mgmt. Prevention of Pressure, shear, friction Prognosis collateral circulation via claudication exercise regimen. Co-morbid CHF, obesity? Skin inspection Increase mobility Probe to bone? Stop smoking Risk of DVT, PE Control HTN Nutrition (protein) / Hydration 90% osteomyelitis risk Control HTN a.5 X-ray, CT, MRI to r/o osteomyelitis and Anticoagulant meds if appropriate Control hyperglycemia Restore hydration. Med need for possible amputation Good nutrition: Ligation of incompetent communicating X-ray, CT, MRI to r/o osteomyelitis and ical, adequate protein Arteriogram: resting leg pain suggests veins need for possible amputation Vit A 25,000 Surgical occlusion at femoral popliteal, or lower Vit C 500 Mgmt. arteries. May need angioplasty, stents Saphenofemoral bypass Arterial bypass: femoral, popliteal or Zn 50 lower Fever: Antibiotics Endarterectomy Valvuloplasty Full or split thickness skin graft or flap Diet: high protein (albumin level) Meds: Vasodilators
Part B b.1 Claudication time (if present) Circumferential measurement Sensation testing w/ Semmes Weinstein Non-blanching erythema (when you PT Tests & Rubor of Dependency: > 30 seconds to monofilaments, 10gm (5.07) indicates press with your finger and take it away it redden in dependent position Edema reduces somewhat with elevation protective sensation. stays red) indicates a Stage 1 ulcer. Measures Venous filling time: > 10-15 seconds for Redness, wamth the arterial circulation to refill the R/O DVT: Vascular studies (Arterial & venous superficial veins in dependent position Well’s Clinical Decision Rule Pressure Ulcer Risk Assessment Scales: conditions may co- (must have intact venous valves) Autar DVT risk assessment scale Wagner Classification Braden, Norton, Gosnell exist) Capillary refill time >3 sec. Press pads of 0 intact skin toes, or soles of feet. Venous filling time: nearly immediate 1 superficial ulcer NPUAP Classification: Stages I – IV ABI < .8 , < .5 = severe 2 deep ulcer Pressure Sore Status Scale, Sussman Tool 3 deep, infected ulcer Auscultation w/ bruits 4 partial foot gangrene Hypertonicity Arterial Flow Doppler (if pulses not 5 full foot gangrene Contractures palpable),
4/3/2018 Page 2 of 3 MU PT 7890, CM I – Wound Management Table Arterial Insufficiency Venous Insufficiency Neuropathic/Diabetic Pressure Ulcer {Includes dry gangrene} b.2 Claudication exercise regimen Compression garment: [when ABI > .8 ] Ambulation Aid when lesion is on plantar Turning schedule q 2 hours Treatment: Semi rigid: Unna’s boot, Circ Aid, surfaces to decrease WB. Ambulation Aid when lesion is on plantar Elastic: long stretch bandage (“Ace”), Weight shift q 15 min in WC. 1) Positioning, surfaces to decrease WB. short stretch bandage, multi-layer Modified footwear to relieve plantar WC push ups 2) Modalities, compression (long + short stretch). pressure zones in wt bearing: WC cushion modifications 3) Assistive Bed Rest (if ABI is very low) and PROM Wear compression garment during waking plastizote insert to disperse pressure, Devices during early healing stage to avoid hours (not at night, when supine) cut outs for pressure zones, 4) Exercise excessive muscle activity that would shunt metatarsal bar/cookie inside shoe, Proper transfer techniques to avoid shear 5) Other blood away from the skin and extremities. Elevate when at rest rocker bottom to decr. toe-off pressures, forces! Reverse Trendelenburg (LE dependent Ankle pumps, standing calf raises, adequate toe box E-Stim - chronic position), HOB elevated 5-7d standing toe curls, resisted ankle PF Never position in full sidelying Warm up –chronic Limb protection Deep Breathing: inhalation creates Total Contact Cast (if not infected) Air flow mattresses negative intrathoracic pressure, which Posterior walking splint (bivalve) Vacuum Assisted Closure helps empty out the vena cavae Podus Boot (suspends heel) (increasing venous circulation) Vacuum Assisted Closure Petroleum jelly for dry skin (avoid alcohol Vacuum Assisted Closure based lotions) Educ: foot inspection, skin and nail care b.3 Cardiovascular disease is Avoid dependent hydrotherapy If WP, cooler temp d/t compromised PLWS 4 – 15 psi, effective for cleansing Wound contraindication for immersion hydro Irrigation, PLWS 4 – 15 psi sensation tunneling Cleansing (impaired heat elimination) Coordinate w/ pain meds Irrigation, PLWS 4 – 15 psi (lower end) VAC Irrigation, PLWS 4 – 15 psi Coordinate w/ pain meds b.4 Sharps (and hydro) contraindicated for Mechanical debridement with gauze Sharps: total excision accelerates healing, Mechanical , Sharps Debridement dry gangrene d/t poor circulation, best to Sharps but caution with lack of protective Methods, let the eschar separate on its own, ie, the Autolytic (semipermeable film is not too sensation / pain response Don’t debride (non infected) heel ulcer! Precautions eschar is a “self - bio occlusive dressing” heavily exudating) (serves as bio occlusive padding) Manage exudate Autolytic; Enzymatic (requires Anti coag therapy contraindicates sharp Anti coagulant therapy contraindicates prescription) to soften dry hard eschar Autolytic (semipermeable film if it is sharp moist enough) Enzymatic (requires prescription) to soften dry, hard eschar b.5 Goal is to moisten: Control Exudate: Maintain moist environment: Packing ribbon/tape for cavity Dressings typically Moderate Iodoform ribbon (briefly if infected) required Hydrogel: Visilon Hydrocolloid: Duoderm Hydrogel: Visilon Hyrdrogel ribbon (function served) Heavy Hydrocolloid: Duoderm Alginates: Algi Derm Hydrocolloid: Duoderm Hydrocolloid: Duoderm Hydrofiber: Aquacell Hydrophilic foam: Tielle
4/3/2018 Page 3 of 3