KAROLINSKA INSTITUTET February 2001 The Microbiology & Tumor Biology Center
Joakim Dillner, M.D., Ph.D. Associate professor of Virology
POPULATION-BASED TYPE-SPECIFIC PREVALENCE OF HIGH RISK HUMAN
PAPILLOMAVIRUS INFECTION IN MIDDLE-AGED SWEDISH WOMEN
Ola Forslund,1* Annika Antonsson,1 Karin Edlund,3 Adrian J. C. van den Brule, 2 Bengt-Göran
Hansson,1 C.J.L.M. Meijer, 2 Walter Ryd,6 Eva Rylander,5 Anders Strand,4 Göran Wadell,3 Joakim
Dillner,1 and Bo Johansson7.
Department of Medical Microbiology, Lund University, University
Hospital, Malmö,1 Department of Pathology, Section of Molecular Pathology, University Hospital
Vrije Universeit, Amsterdam, The Netherlands,2 Department of Virology, University of Northern
Sweden, Umeå,3 Department of Medicine, Dermatology, and Venereology, University Hospital,
Uppsala,4 Dept of Obstetrics and Gynecology, Karolinska Institute, Danderyd Hospital,5 Department of Dermato-Venereology, Sahlgrenska University Hospital, Göteborg,6 Division of Clinical
Virology, Karolinska Institute, Huddinge University Hospital, Sweden.7
Running title: HR HPV among middle-aged Swedish women
Mailing address Visiting Address Phones Fax E-Mail 171 77 STOCKHOLM Fogdevreten 2 + 46 8 728 6299 + 46 8 304276 [email protected] Sweden SOLNA KAROLINSKA INSTITUTET February 2001 2
ABSTRACT
Objective To determine the prevalence and spectrum of high risk (HR) human papillomavirus (HPV) types in a large real-life population-based cervical screening setting of middle-aged Swedish women, since HPV might be used as a marker for identification of women at risk for development of cervical cancer.
Method Cervical brush samples from 6,125 women, 32- 38 years of age, in a multicenter study were analysed using a general HPV primer (GP5+/6+) PCR-enzyme immunoassay (EIA) combined with reverse dot blot hybridization (RDBH) for confirmation and HPV typing in a single assay.
Results Altogether, 6.6% (402/6,125) were confirmed HR HPV positive. Infections with 13 different HR HPV types were detected of which HPV 16 was the most prevalent type (2.0%; 123/6,125), followed by HPV 31 (1.0%; 63/6,125). Any one of the HPV types 18, 33, 35, 39, 45, 51, 52, 56, 58, 59 or 66 was detected in 3.5% (217/6,125) of the women. Infection with two, three and five types simultaneously was identified in 32, five and one women, respectively.
Conclusion The combination of PCR-EIA as a screening test and RDBH as a confirmatory test, was found to be readily applicable to a real-life population-based cervical screening setting. The women were infected with a heterogeneous group of HPV types of which HPV 16 and 31 were the most frequent types. The HR HPV prevalence of 6.6% suggests that HPV screening may be a favorable strategy to identify middle-aged women at risk for developing cervical cancer. KAROLINSKA INSTITUTET February 2001 3
INTRODUCTION Cancer of the cervix uteri is the second leading cause of mortality among women worldwide and the incidence has been estimated to about 500,000 new cases each year (1). The human papillomavirus
(HPV) has been identified as the major causal agent of the disease (2) and up to 99.7% of cervical cancers have been found to carry the HPV genome (3). HPV types frequently detected in cervical cancers are classified as ‘high-risk’ (HR) viruses, while those rarely or never found in cancer are called
‘low risk’ (LR) types (4). HPV infections are also detected among cytologically healthy women, with a peak prevalence of about 20 – 25% at 20 – 24 years of age, correlating with the onset of sexual activity. However, the infection is transient in most women (5). A decline in HPV prevalence is observed with increasing age and at around 35 years of age the prevalence of HPV infection among cytologically normal women has been reported to be around 5% (6, 7). Persistence of HPV infection is associated with HR HPV types and is more frequent in women older than 30 years of age than among those under 24, indicating that HPV positive older women may represent a subset of women with difficulty to clear the infection (8).
Screening for cervical intraepithelial neoplasia (CIN) has been shown to be an effective method to reduce both incidence and mortality of invasive cervical cancer (9-11). Despite the success of screening using the Papanicolau (Pap) smear the cytological examination manifests a sensitivity of only about 75% (11, 12). Furthermore, the Pap smear screening has shown low sensitivity for adenocarcinomas (13) and large variations of cytological false negative and false positive rates between laboratories (14, 15). These limitations and the fact that almost all cervical cancers are positive for HPV (3) and is preceded by persistent HPV infections (16-19) argue for evaluation of
HPV testing in cervical cancer screening programs. The most appropriate group for HPV screening is women aged 30 years or more, since younger age groups have high HPV prevalences and low cervical cancer incidences (7, 20). Recently, a standardized PCR-EIA test for HR HPV DNA in crude cell suspension has been developed and validated to be reproducible and extremely sensitive for HPV KAROLINSKA INSTITUTET February 2001 4 detection (21, 22). The PCR-EIA could be applicable for cervical cancer screening. However, to identify the exact HPV genotype of a positive PCR-EIA additional analyses have to be performed. The reverse dot blot hybridization (RDBH) assay (23) could be a method of choice for HPV genotyping and confirmation of samples positive in the PCR-EIA.
The aims of this study is to determine the prevalence and spectrum of HR HPV types of cervical samples in a large real-life population-based cervical screening setting of middle-aged Swedish women by the PCR-EIA method combined with the RDBH assay. KAROLINSKA INSTITUTET February 2001 5
MATERIALS AND METHODS
Study group
In the organized program, all women belonging to the age groups eligible for screening are invited for screening by letter at 3-year intervals. Women who have had a Pap smear taken within the previous 3 years are not invited. For the present study, eligible women were defined as women in the age group
32 – 38 years participating in the population-based cervical screening program in five different cities/regions in Sweden (Malmö, Göteborg, Stockholm, Uppsala and Umeå). In total, 12,522 women were enrolled. Of these, 6,320 women were randomized to the testing group, and 6,125 cervical scrapes were positive in the PCR adequacy test.
Polymerase chain reaction
From each woman two cervical scrapes were obtained by the use of a cytobrush. The first sample was used for routine cytological screening, and cells from the second sample were placed in 1 mL 0.9%
NaCl and stored at -20C. Samples from the cities of Malmö, Stockholm and Umeå were analyzed for
HPV at the regional laboratory, respectively, whereas samples from Uppsala and Göteborg were sent frozen to Malmö for analysis. Samples were analyzed by a general HPV primer GP5+/6+ mediated
PCR enzyme immunoassay EIA (21). Prior to analysis the cells were thawed and centrifuged for 10 min at 3,000 x g. The cell pellet was resuspended in 1 mL 10 mM TRIS-HCl (pH 7.5) and frozen at
-20C. Then the samples were thawed and aliquots of 100 uL were boiled for 10 min, and 10 uL was used in a 50 uL reaction mixture containing 200 uM of each dNTP, 3.5 mM MgCl2, 1 U AmpliTaq
DNA polymerase and reaction buffer (Perkin Elmer, Foster City, Ca), 0.5 uM biotinylated GP6+ primer and 0.5 uM GP5+ primer (24). The quality of the sample DNA for amplification was analyzed in separate tubes by using a -globin PCR with biotinylated-BGPC03 and BGPC05 primers (25). KAROLINSKA INSTITUTET February 2001 6
For the PCR, the laboratory of Malmö used a Hybaid OmniGene (Hybaid, Middlesex, UK) automated thermal cycler programmed for block temperature and Umeå used a PTC-200 (MJ Research) with
’calculated control’ mode. For PCR with GP+ primers a denaturation step at 94C for 4 min was followed by 40 cycles of amplification with segments at 94C for 1.5 min, 40C for 1.5 min, 72C for
2 min, and a final step at 72C for 4 min. The laboratory of Stockholm used a GeneAmp 9700 (Perkin
Elmer) with a denaturation step at 94C for 4 min followed by 40 cycles at 94C for 1 min, 38C for 1 min, 71C for 2 min, and a final step at 71C for 4 min. The -globin PCR was performed under the same conditions but the annealing temperature was at 45C.
As positive controls of -globin, input of 1 ng and 10 ng human placental DNA (Sigma) were used. As positive controls of the HPV PCR, ten-fold dilutions of purified DNA from SiHa cells were used, ranging from 10 ng to 100 pg of input DNA in a background of 100 ng human placental DNA (Sigma).
As negative control 10 uL of water was added to the PCR and processed as the samples.
Enzyme immunoassay (EIA)
Amplified DNA was detected by enzyme immunoassay (21). Five uL of biotinylated HPV PCR products were captured on streptavidin coated microtitre plates (Boehringer Mannheim, Mannheim,
Germany) after adding 50 uL hybridization buffer (1 x SSC, 0.5 % Tween 20). The plates were incubated at 37C for 1h. After 3 washings with 200 uL hybridization buffer per well, amplicons were denatured with 100 uL 0.2 M NaOH for 15 min at room temperature. Then the plates were washed 3 times with hybridization buffer, and 50 uL of hybridization buffer containing 10 uM of each HPV specific digoxigenin-11-ddUTP labeled probe was added per well. The probe solution contained a cocktail of 14 oligo probes for the HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68.
After hybridization at 37C for 1h, the plates were washed twice and 50 uL alkaline phosphatase conjugated anti-DIG (75 mU/mL hybridization buffer, Boehringer Mannheim) was added per well. KAROLINSKA INSTITUTET February 2001 7
The plates were incubated at 37C for another 1h, and then washed five times, and 100 uL of pNPP substrate (SIGMA) was added per well. Plates were incubated overnight at 37C and ODs were measured at 405 nM. By using a digoxigenin labeled probe (5’-
AAGAGTCAGGTGCACCATGGTGTCTGTTTG) the same procedure was used for analyzing the amplified DNA from the -globin PCR.
For interpretation of results, cut off was set to three times of the mean OD-value of two negative controls. For each plate, the EIA was approved only if the positive control of 10 pg SiHa DNA was above cut off. The plate for -globin test was approved if the controls with 10 ng human DNA were above cut off, after overnight incubation.
Typing of HPV
Aliquots (20 uL) of PCR solutions from positive EIA samples were sent frozen for typing at a single laboratory (Malmö). HPV types were determined by the use of a non-radioactive reverse dot blot hybridization (RDBH) (23). The membranes for use in the RDBH were prepared as follows.
Recombinant HPV plasmids (100 ng DNA/dot), corresponding to the different HPV types tested for in the EIA were denatured at high pH (0.8 M NaOH, 0.5 mM EDTA) for 20 min and transferred by use of a manifold (Schleicher & Schuell, Dassel, Germany) to a prewetted (6 x SSC) nylon membrane
(Hybond N+, Amersham, Buckinghamshire, England). The membrane was neutralized with 200 uL 20 x SSPE, dried for 30 min at room temperature and baked at 120C for 20 min. Prehybridization of membranes was done for 1h at 46C in 5 mL solution containing 50% deionized formamide, 1% SDS,
10% dextran sulphate, 1 M NaCl and 100 ug/mL of herring sperm DNA in a hybridization oven
(Hybaid). Five uL of PCR solution was added to 50 uL of prehybridization solution, denaturated at KAROLINSKA INSTITUTET February 2001 8
94C for 5 min and transferred to the prehybridization solution. After hybridization overnight, the membrane was rinsed once and then for 3 x 15 min with 2 x SSPE plus 0.1% SDS at 65C and incubated with 5 mL blocking solution at 65C for 1h [3% bovine serum albumin in TBS-Tween (100 mM Tris-HCl, 150 mM NaCl, 0.05% v/v Tween 20, pH 7.5), filtered through a sterile 0.45 uM membrane, (Acrodisc, Gelman Sciences, Ann Arbor, MI)]. Blocking solution was removed and the membrane was incubated at room temperature for 10 min with 5 mL of streptavidin-alkaline phosphatase [Gibco-BRL, diluted 1/3300 in TBS-Tween and filtered through a sterile 0.22 uM membrane (Millipore S. A., Molsheim, France)]. The membrane was washed at room temperature for
2 x 10 min with TBS-Tween and finally with 5 mL washing buffer (100 mM Tris-HCl, 100 mM NaCl,
50 mM MgCl2, pH 9.5) for 1 h. Thereafter, the membrane was dried briefly on a filter paper to remove excess buffer, dipped in detection reagent (Lumi-Phos 530, Lumigen Inc, Southfield, MI) and placed in a transparent folder and incubated for 1.5 h at room temperature. The membrane was exposed to X- ray film (Kodak X-AR, Kodak Rochester, NY) in a cassette with intensifying screens (Du Pont,
Cronex lightning plus, NEN, Boston, MA) for 10 min. An HPV type was considered identified when clear-cut spot of darkening of the film could be distinguished from the background.
The project was approved by the Institutional Review Board of the Karolinska Institute, decision number 96:305. KAROLINSKA INSTITUTET February 2001 9
RESULTS
HPV screening
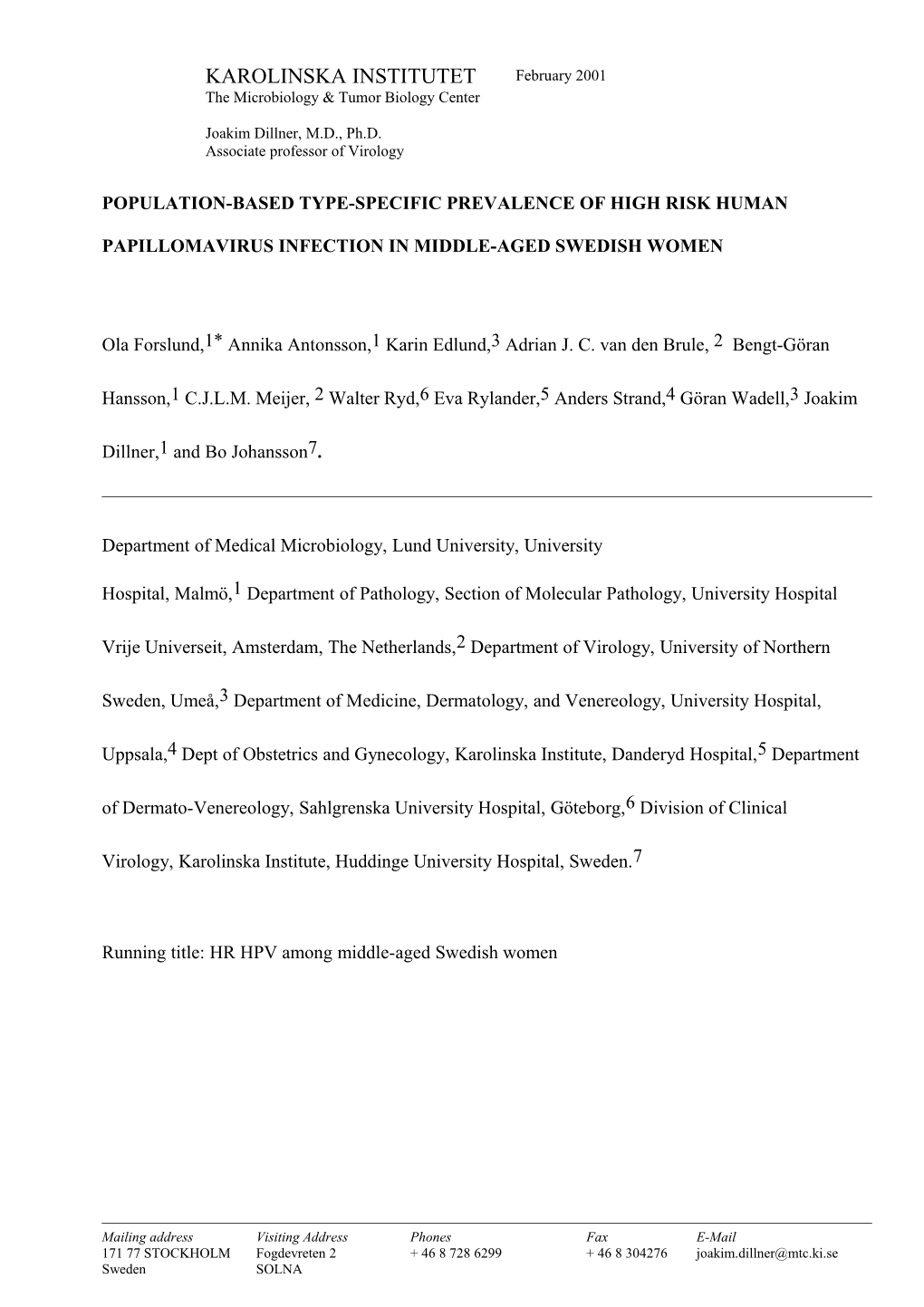
Totally, 6.6% (401/6,125) of the women were found positive for HR HPV DNA after confirmation by RDBH. The range of positivity for the different regions in Sweden was between 5.3 and 8.0% (Table 1). The -globin quality test revealed that 3.1% (195/6,320) of the samples were not amplifiable and that the proportion of -globin negative samples varied between 0.7% and 13% between different regions (Table 2). For 27 of the EIA positive samples no HPV type could be identified by RDBH, but DNA sequencing revealed that two of these samples harbored HPV type 6, two contained HPV 42 and one sample contained HPV 67. Another sample was found to harbor both HPV 42 and 43 by a RDBH for LR HPV types. These four HPV types were not included in the HR HPV probe mix and were therefore not included in the ordinary RDBH either. Of the remaining 21 non-typed samples, 19 samples from Stockholm showed a mean OD-value of 1.6 (SD=0.97) above cut off and two samples from Umeå had values close to cut off (0.010 and 0.019).
HPV type distribution
In total, 13 different HR HPV types were identified among the women (HPV 68 was not identified) (Table 1). HPV 16 was the most prevalent type, found in 2.0% (123/6,125) followed by HPV 31 found in 1.0% (63/6,125), and anyone of the HPV types 18, 33, 35, 39, 45, 51, 52, 56, 58, 59 or 66 were detected in 3.5% (217/6,125) of the women (Figure 1). Infection with two, three and five types simultaneously was identified in 32, five and one women, respectively. By RDBH, HPV was successfully typed in 94% (402/429) of the EIA positive samples. Figure 2 is a representative example of an RDBH analysis of four samples. KAROLINSKA INSTITUTET February 2001 10
DISCUSSION
To the best of our knowledge, this is the largest population based HPV study of middle-aged women showing a HR HPV prevalence of 6.6%. By the confirmatory RDBH method, 13 HR
HPV types were identified of which HPV 16 was the most frequent type followed by HPV 31.
Out of the remaining HPV types 18, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68 contained in the HR probe mixture, HPV 68 was the only type not found in the present material.
The combination of PCR-EIA as a screening test and RDBH as a confirmatory test, that also provides the exact HPV types present in the sample, was found to be readily applicable to a real-life population-based cervical screening setting. Regional HPV screening laboratories sent aliquots of PCR solutions from positive PCR-EIA samples for independent verification and
HPV typing at a national reference laboratory that performed the RDBH analysis. By this approach, most of the EIA positive samples (94%) were confirmed and the HPV type identified.
By using a reverse line blot assay (containing fixed oligonucleotide probes on a strip), allowing identification of 27 HPV types a sensitivity of 88% has been reported for typing of
HPV DNA generated by PCR with MY09 and MY11 primers (26). Also, oligonucleotide based reverse blotting for 37 HPV types has been developed and is currently being evaluated
(Van den Brule et al., unpublished observation).
Our RDBH can easily be combined with the MY09/MY11 PCR system by using a hybridization temperature of 56C in the RDBH (23). However, for 6 of the EIA positive samples that could not be confirmed by RDBH, LR HPV types (HPV types 6, 42, 43 and 67) were identified. In accordance with this finding we have recently found, from another series of KAROLINSKA INSTITUTET February 2001 11 samples, that some samples with high copy numbers of LR HPV types cross-hybridized with the HR probe in the EIA. This cross-hybridization in a few samples can be avoided if hybridization is performed at 55C instead of 37C.
By the -globin sample adequacy test, 3% of the samples showed values below cut-off. In a HPV screening study of Dutch women, using the same technique for sample accuracy (except that visualization was performed by gel electrophoresis), 5% (184/3,489) of the samples were negative for human DNA (7). In our study, the proportion of -globin negative samples varied between 0.7% and
13%. Although the same sampling procedures and the same systems for collection, storage and transportation of samples were used in all regions, it appears that there may have been regional differences in how the samples actually were taken and processed. The nature of these differences is not clear. However, about 1,500 cells (calculated from the used cut-off at 10 ng human placental DNA and that one diploid cell contains about 6 x 109 base pairs) were required for a positive -globin test in the PCR-EIA. This rather low sensitivity of the sample adequacy test is appropriate, since a sample adequacy test should never be more sensitive than the diagnostic test itself.
The prevalence of HR HPV is known to decrease with increasing age, from about 20% among women of 20-30 years to about 5% in women over 30 years of age (25, 27, 28). However, only few population based studies of HR HPV prevalence have been performed of women above 30 years of age. In addition, to our large population based study showing 6.6% HR HPV among women 32-38 years,
Rozendaal et al., report 5.4% (121/2250) HR HPV of women aged 34-54 years of age by PCR-EIA
(29), and Ratnam et al., found 5.0% (27/536) HR HPV of women in the 35-44 age group by Hybrid
Capture assay (30).
Infection with multiple types of HPV has been related to persistency of HPV for more than 6 months
(31) and may therefore be a risk factor for CIN. Only 0.6% (38/6,125) and 0.7% (24/3,351) of our KAROLINSKA INSTITUTET February 2001 12
Swedish and Dutch women 30-39 of age with normal cytology (7), respectively, have been found positive for multiple HR HPV types simultaneously. It is possible that selective amplification of the
PCR reaction of only some of the types present in a sample may have underestimated the true proportion of multiple infections.
In several studies of women with normal cytology or with different grades of CIN, HPV 16 has been found to be the most prevalent HPV type followed by HPV 31 (7, 28, 32). Also in our study HPV 16 and HPV 31 predominated, indicating that the type distribution of HPV infection is rather similar in several different populations. A spectrum of different HPV types was present in Sweden, with 13/14
HR HPV types tested for being found. In a similar Dutch HPV prevalence survey of women with normal cytology, all of the 14 HR types that we tested for were detected. In addition HPV 34 and 70 were detected. Their probe cocktail was extended to contain 19 HR HPV types based on the phylogenetic relatedness (also HPV 26, 34, 53, 70 and 73 apart from the types tested for by us) (7).
There were no HPV 53 isolates in the Dutch study, in spite of the fact that this type was the most prevalent one among American women developing atypical squamous cells of undetermined significance (ASCUS) when another general primer PCR system was used (MY09/MY11) (33). The
GP+ primer system has been reported to have a lower sensitivity for HPV53 (about 3-log) compared to the MY09/11 system (34). Difference in prevalence of HPV 53 might also be due to geographical differences.
The issue of which oncogenic HPV types that should be tested for in primary HPV screening programs is debated. The cost-efficiency of HPV screening will decrease when infections that are very rare or only rarely progress to cancer are screened for, and we therefore decided to evaluate screening only for the 14 major oncogenic HPV types.
In conclusion, a sensitive and simple HPV screening test (PCR-EIA) in combination with an independent confirmatory HPV typing test (RDBH) is useful for field trials of screening for high risk
HPV infection. The HPV prevalences and type distribution in Sweden in this age group are similar to KAROLINSKA INSTITUTET February 2001 13 the figures that have been used in the mathematical modeling studies which indicated that HPV screening could substantially improve cervical screening programs (35) and thus suggest that HPV screening may be a favorable strategy for cervical cancer prevention. We are therefore currently conducting a large population based study of middle aged aged Swedish women to test if HR HPV detection might improve cervical screening.
ACKNOWLEDGMENT
We are grateful to staff involved in the population-based cervical screening program in Sweden for enrolling the women and taking the cervical brush samples.
This work was supported by the Swedish Cancer Society and by Europe against Cancer contract number 96 201748 05 F01 for the enrollment period 1997-01-01 to 1998-06-30 and by contract number 99/CAN/36731; SI2.168540 (2000CVF2-002) for the time period 1999-08-30 to 2000-12-15. KAROLINSKA INSTITUTET February 2001 14
REFERENCES
1. Schoell, W. M., Janicek, M. F., and Mirhashemi, R. Epidemiology and biology of cervical cancer. Semin Surg Oncol, 16: 203-11, 1999.
2. zur Hausen, H. Papillomavirus infections-a major cause of human cancers. Biochim Biophys Acta, 1288: F55-78, 1996.
3. Walboomers, J. M., Jacobs, M. V., Manos, M. M., Bosch, F. X., Kummer, J. A., Shah, K. V., Snijders, P. J., Peto, J., Meijer, C. J., and Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol, 189: 12-19, 1999.
4. Lörincz, A. T., Reid, R., Jenson, A. B., Greenberg, M. D., Lancaster, W., and Kurman, R. J. Human papillomavirus infection of the cervix: relative risk associations of 15 common anogenital types. Obstet Gynecol, 79: 328-37, 1992.
5. Evander, M., Edlund, K., Gustafsson, A., Jonsson, M., Karlsson, R., Rylander, E., and Wadell, G. Human papillomavirus infection is transient in young women: a population-based cohort study. J Infect Dis, 171: 1026-30, 1995.
6. de Villiers, E. M., Wagner, D., Schneider, A., Wesch, H., Munz, F., Miklaw, H., and zur Hausen, H. Human papillomavirus DNA in women without and with cytological abnormalities: results of a 5-year follow-up study. Gynecol Oncol, 44: 33-9, 1992.
7. Jacobs, M. V., Walboomers, J. M., Snijders, P. J., Voorhorst, F. J., Verheijen, R. H., Fransen- Daalmeijer, N., and Meijer, C. J. Distribution of 37 mucosotropic HPV types in women with cytologically normal cervical smears: the age-related patterns for high-risk and low- risk types. Int J Cancer, 87: 221-7, 2000.
8. Hildesheim, A., Schiffman, M. H., Gravitt, P. E., Glass, A. G., Greer, C. E., Zhang, T., Scott, D. R., Rush, B. B., Lawler, P., Sherman, M. E., and et al. Persistence of type-specific human papillomavirus infection among cytologically normal women. J Infect Dis, 169: 235-40, 1994. KAROLINSKA INSTITUTET February 2001 15
9. Läärä, E., Day, N. E., and Hakama, M. Trends in mortality from cervical cancer in the Nordic countries: association with organised screening programmes. Lancet, 1: 1247-9, 1987.
10. Mahlck, C. G., Jonsson, H., and Lenner, P. Pap smear screening and changes in cervical cancer mortality in Sweden. Int J Gynaecol Obstet, 44: 267-72, 1994.
11. Pontén, J., Adami, H. O., Bergstrom, R., Dillner, J., Friberg, L. G., Gustafsson, L., Miller, A. B., Parkin, D. M., Sparen, P., and Trichopoulos, D. Strategies for global control of cervical cancer. Int J Cancer, 60: 1-26, 1995.
12. Boyes, D. A., Morrison, B., Knox, E. G., Draper, G. J., and Miller, A. B. A cohort study of cervical cancer screening in British Columbia. Clin Invest Med, 5: 1-29, 1982.
13. Chamberlain, J. Reasons that some screening programmes fail to control cervical cancer. In: M. Hakama, A. Miller, and N. Day (eds.), Screening for cancer of the uterine cervix. 76, pp. 161-8: IARC, 1986.
14. Yobs, A. R., Swanson, R. A., and Lamotte, L. C., Jr. Laboratory reliability of the Papanicolaou smear. Obstet Gynecol, 65: 235-44, 1985.
15. Falcone, T., and Ferenczy, A. Cervical intraepithelial neoplasia and condyloma: an analysis of diagnostic accuracy of posttreatment follow-up methods. Am J Obstet Gynecol, 154: 260-4, 1986.
16. Remmink, A. J., Walboomers, J. M., Helmerhorst, T. J., Voorhorst, F. J., Rozendaal, L., Risse, E. K., Meijer, C. J., and Kenemans, P. The presence of persistent high-risk HPV genotypes in dysplastic cervical lesions is associated with progressive disease: natural history up to 36 months. Int J Cancer, 61: 306-11, 1995.
17. Schiffman, M. H., and Brinton, L. A. The epidemiology of cervical carcinogenesis. Cancer, 76: 1888-901., 1995. KAROLINSKA INSTITUTET February 2001 16
18. Ho, G. Y., Burk, R. D., Klein, S., Kadish, A. S., Chang, C. J., Palan, P., Basu, J., Tachezy, R., Lewis, R., and Romney, S. Persistent genital human papillomavirus infection as a risk factor for persistent cervical dysplasia. J Natl Cancer Inst, 87: 1365-71., 1995.
19. Nobbenhuis, M. A., Walboomers, J. M., Helmerhorst, T. J., Rozendaal, L., Remmink, A. J., Risse, E. K., van der Linden, H. C., Voorhorst, F. J., Kenemans, P., and Meijer, C. J. Relation of human papillomavirus status to cervical lesions and consequences for cervical-cancer screening: a prospective study. Lancet, 354: 20-5., 1999.
20. Cuzick, J., Sasieni, P., Davies, P., Adams, J., Normand, C., Frater, A., van Ballegooijen, M., and van Den Akker, E. A systematic review of the role of human papillomavirus testing within a cervical screening programme. Health Technol Assess, 3: 1-204, 1999.
21. Jacobs, M. V., Snijders, P. J., van den Brule, A. J., Helmerhorst, T. J., Meijer, C. J., and Walboomers, J. M. A general primer GP5+/GP6(+)-mediated PCR-enzyme immunoassay method for rapid detection of 14 high-risk and 6 low-risk human papillomavirus genotypes in cervical scrapings. J Clin Microbiol, 35: 791-5, 1997.
22. Jacobs, M. V., Snijders, P. J., Voorhorst, F. J., Dillner, J., Forslund, O., Johansson, B., von Knebel Doeberitz, M., Meijer, C. J., Meyer, T., Nindl, I., Pfister, H., Stockfleth, E., Strand, A., Wadell, G., and Walboomers, J. M. Reliable high risk HPV DNA testing by polymerase chain reaction: an intermethod and intramethod comparison [published erratum appears in J Clin Pathol 1999 Oct;52(10):790]. J Clin Pathol, 52: 498-503, 1999.
23. Forslund, O., Hansson, B. G., and Bjerre, B. Typing of human papillomaviruses by consensus polymerase chain reaction and a non-radioactive reverse dot blot hybridization. J Virol Methods, 49: 129-39, 1994.
24. de Roda Husman, A. M., Walboomers, J. M., van den Brule, A. J., Meijer, C. J., and Snijders, P. J. The use of general primers GP5 and GP6 elongated at their 3' ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol, 76: 1057-62, 1995. KAROLINSKA INSTITUTET February 2001 17
25. de Roda Husman, A. M., Walboomers, J. M., Hopman, E., Bleker, O. P., Helmerhorst, T. M., Rozendaal, L., Voorhorst, F. J., and Meijer, C. J. HPV prevalence in cytomorphologically normal cervical scrapes of pregnant women as determined by PCR: the age-related pattern. J Med Virol, 46: 97-102, 1995.
26. Coutlee, F., Gravitt, P., Richardson, H., Hankins, C., Franco, E., Lapointe, N., and Voyer, H. Nonisotopic detection and typing of human papillomavirus DNA in genital samples by the line blot assay. The Canadian Women's HIV study group. J Clin Microbiol, 37: 1852-7, 1999.
27. Melkert, P. W., Hopman, E., van den Brule, A. J., Risse, E. K., van Diest, P. J., Bleker, O. P., Helmerhorst, T., Schipper, M. E., Meijer, C. J., and Walboomers, J. M. Prevalence of HPV in cytomorphologically normal cervical smears, as determined by the polymerase chain reaction, is age- dependent. Int J Cancer, 53: 919-23, 1993.
28. Hansson, B. G., Forslund, O., Bjerre, B., Lindholm, K., and Nordenfelt, E. Human papilloma virus types in routine cytological screening and at colposcopic examinations. Eur J Obstet Gynecol Reprod Biol, 52: 49-55, 1993.
29. Rozendaal, L., Westerga, J., van der Linden, J. C., Walboomers, J. M., Voorhorst, F. J., Risse, E. K., Boon, M. E., and Meijer, C. J. PCR based high risk HPV testing is superior to neural network based screening for predicting incident CIN III in women with normal cytology and borderline changes. J Clin Pathol, 53: 606-11., 2000.
30. Ratnam, S., Franco, E. L., and Ferenczy, A. Human papillomavirus testing for primary screening of cervical cancer precursors. Cancer Epidemiol Biomarkers Prev, 9: 945-51., 2000.
31. Ho, G. Y., Bierman, R., Beardsley, L., Chang, C. J., and Burk, R. D. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med, 338: 423-8, 1998.
32. Nindl, I., Lotz, B., Kuhne-Heid, R., Endisch, U., and Schneider, A. Distribution of 14 high risk HPV types in cervical intraepithelial neoplasia detected by a non-radioactive general primer PCR mediated enzyme immunoassay. J Clin Pathol, 52: 17-22, 1999. KAROLINSKA INSTITUTET February 2001 18
33. Liaw, K. L., Glass, A. G., Manos, M. M., Greer, C. E., Scott, D. R., Sherman, M., Burk, R. D., Kurman, R. J., Wacholder, S., Rush, B. B., Cadell, D. M., Lawler, P., Tabor, D., and Schiffman, M. Detection of human papillomavirus DNA in cytologically normal women and subsequent cervical squamous intraepithelial lesions. J Natl Cancer Inst, 91: 954-60, 1999.
34. Qu, W., Jiang, G., Cruz, Y., Chang, C. J., Ho, G. Y., Klein, R. S., and Burk, R. D. PCR detection of human papillomavirus: comparison between MY09/MY11 and GP5+/GP6+ primer systems. J Clin Microbiol, 35: 1304-10, 1997.
35. van Ballegooijen, M., van den Akker-van Marle, M. E., Warmerdam, P. G., Meijer, C. J., Walboomers, J. M., and Habbema, J. D. Present evidence on the value of HPV testing for cervical cancer screening: a model-based exploration of the (cost-)effectiveness. Br J Cancer, 76: 651-7, 1997. KAROLINSKA INSTITUTET February 2001 19
Legends to figures.
Figure 1. Prevalence of high risk HPV types within population-based cervical screening of Swedish women, 32 to 38 years of age, as determined by PCR-EIA and typing by reverse dot blot hybridization
(RDBH).
Figure 2. Reverse dot blot hybridization (RDBH) of biotinylated amplimers from PCR-EIA with
GP5+/6+ primers: a) Positions of immobilized HPV types. b) Identification of HPV types. Sample 1,
HPV 16; sample 2, HPV 31, 35 and 66; sample 3, HPV 31; sample 4, HPV 51.
2.0 2.0 1.5 1.0 % 1.0 0.6 0.7 0.4 0.3 0.4 0.3 0.5 0.3 0.3 0.5 0.2 0.2 0.0 16 18 31 33 35 39 45 51 52 56 58 59 66 68 HPV types