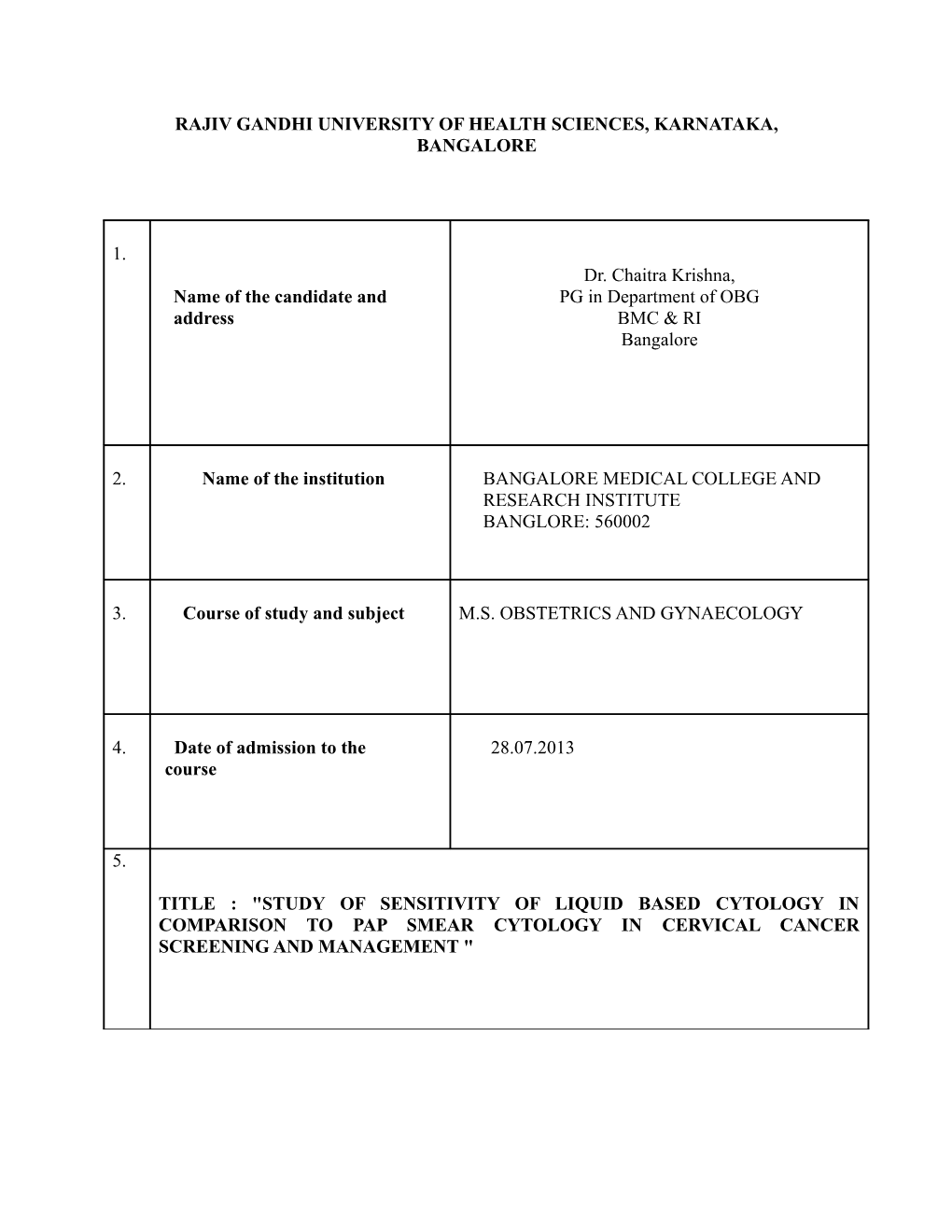
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE
1. Dr. Chaitra Krishna, Name of the candidate and PG in Department of OBG address BMC & RI Bangalore
2. Name of the institution BANGALORE MEDICAL COLLEGE AND RESEARCH INSTITUTE BANGLORE: 560002
3. Course of study and subject M.S. OBSTETRICS AND GYNAECOLOGY
4. Date of admission to the 28.07.2013 course
5.
TITLE : "STUDY OF SENSITIVITY OF LIQUID BASED CYTOLOGY IN COMPARISON TO PAP SMEAR CYTOLOGY IN CERVICAL CANCER SCREENING AND MANAGEMENT " 6. Brief resume of the intended work
6.1 Need for the study: Globally, cervical cancer is the second most common cancer in women and the third most frequent cause of cancer death (IARC,WHO2002) [1]. Cancer of cervix is preventable and yet approximately 4,93,100 new cases and more than 2,73,000 deaths occur among women worldwide [1]. India which accounts for one-sixth of world`s population also bears one-fifth world`s burden of cervical cancer [2].Cervical cancer is a leading form of cancer among women living in low resource regions and often kills them at young age when they are still raising families. Invasive cervical cancer is considered a preventable disease because it has a long pre-invasive state, cervical cytology screening programs are currently available and the treatment of pre-invasive lesions is effective. HPV is considered the primary driving force behind malignant transformation of cervical cells with certain high risk HPV types now labeled as the first ever identified, indisputable, solely infectious cause of a human cancer[3].
Conventional cytology, i.e., the Papanicolaou smear, has been the mainstay of cervical cancer screening since the 1960s and is credited with successfully reducing the incidence and mortality of invasive cervical cancer in many developed countries. Nonetheless, the accuracy of this important screening tool remains controversial, with several large meta-analyses suggesting that both the sensitivity and specificity of cervical cytology is relatively low (30% to 87% sensitivity, 86% to 100% specificity)[4]. As an alternative to conventional cytology, liquid based-cytology (LBC) was introduced in the mid-1990s. The purported advantages of LBC include a possible increase in the detection of high-grade cervical intraepithelial neoplasia (CIN2,3), a reduction in the number of unsatisfactory specimens, and providing residual cellular material for subsequent molecular testing (e.g., testing for ‘‘high-risk’’ types of HPVDNA) [5]. At the moment, the majority of these techniques are using expensive automated devices leading to a significant increase in the price of LBC
6.2 Review of literature
Sampling and preparation errors are responsible for more than 70% of false-negative in Pap smears. When abnormal cells are present on the slide, they may be difficult to identify and interpret in conventional smears because of the obscuring effects of air-drying artifact, excess blood, mucus, and inflammatory debris, or areas of thick cellularity where there may be insufficient permeation of the fixative [6] To address these issues, a new slide preparation method applied to gynecologic specimens was developed. The cervical sample is taken in the routine manner using conventional sampling devices. Instead of smearing the sample onto a glass slide, the collection device is rinsed in a vial containing 20 mL of a buffered alcohol liquid preservative. initial studies suggested a substantial increase in detection of biopsy-confirmed, high-grade cervical abnormalities, ranging from 16% to 100%. The same studies showed a significant decrease in “unsatisfactory” smear reports.
Jung Dal Lee Oh et al, conducted study on Korean women, Comparison of the performance of liquid based cytology with that of conventional smears showed that this system is vastly Superior in terms of the preservation of epithelial cells, staining quality, and the elimination of obscuring artifacts. Likely reasons for this superior performance include the fact LBC preparations are made up of uniformly dispersed cells, with backgrounds free of red blood cells, mucus, and overlapping artifacts [7]
Annie N. Y et al conducted study on Asian women revealed, with liquid based cytology, the unsatisfactory rate was reduced from 0.48% to 0.32%. The detection rates of squamous cell carcinomas, adenocarcinomas, and high-grade squamous intraepithelial lesions (HSIL) were essentially unchanged. There was an increase in the detection of atypical squamous cells of undetermined significance and low-grade Limited biopsy correlation confirmed the increased sensitivity of liquid based cytology. [8]
Scottish Cervical Screening Programme pilot study reported that use of LBC increased detection of HSIL and significantly reduced unsatisfactory smear rates when compared with the conventional smear. LBC was subsequently introduced into the Scottish Cervical Screening Programme. [9]
Similar findings were reported in England after interim clinical assessment of the pilot conducted by the U.K. National Screening Program. This led the National Institute for Clinical Excellence, U.K. (NICE) in 2003 to recommend LBC be used as the primary cervical cancer screening tool in England and Wales. [10]
Ronco et al reported a randomized, controlled comparison of conventional cytology with liquid based cytology in over 45,000 women presenting for primary screening in 9 centers in Europe. Liquid-based cytology showed significantly increased sensitivity for CIN1 but not for CIN3 or invasive cancer. Detection of high-grade disease and invasive cancer was similar in both groups suggesting sensitivity and frequency of false-negative results were also similar. The probability of histologically confirmed CIN after a positive result was lower in the LBC group suggesting lower specificity, lower positive-predictive value and higher false-positive rates. [11]
U.S. Agency for Health Care Policy and Research (AHCPR) assessed the efficiency and cost effectiveness of new cervical cytologic screening technologies based on a metaanalysis of published research. The report indicated an improved sensitivity for LBC as opposed to conventional cytology with reported increased detection of atypical squamous cells of undetermined significance (ASC-US) and low-grade squamous intraepithelial lesions (LSIL). The revised guidelines of the ACS recommended liquid-based cytology as an alternative to conventional smears with screening to be performed every two years. [12] 6.3 Objectives of the study:
1. To compare the efficacy of conventional PAP smear and liquid based cytology for the detection of cervical cancer.
2. To study the Sensitivity and Specificity of conventional PAP smear and liquid based cytology.
3. Management of Cervical lesions
7.1 Materials and methods:
. Two cervical smears are simultaneously prepared from each enrollee, one of which is processed as a Conventional PAP smear and the other used for a Liquid Based Cytology. The samples are obtained with a specially designed Cytobrush. After performing the cervical smear, the Cytobrush is rinsed and the sample is collected in a proprietary preservative vial. Batched samples are then placed on the preparation workstation. Then a series of preparation steps are automatically performed, including cellular dispersion by agitation, epithelial cell enrichment by filtration, cell transfer to glass slides, and staining.
7.2A Study design: Prospective study
7.2B Study period: October 2013 to May 2015
7.2C Study population: Vani Vilas Hospital and Bowring & Lady Curzon Hospital, BMCRI, Bangalore.
7.2D Sample size: 100 patients
7.2E Inclusion criteria: 1. Women visiting gynecology OPD 2. Women in Reproductive age group 3. Women with unhealthy cervix
7.2F Exclusion criteria : 1. Age group between 21 to 24 years 2. Pregnant women 3. Menstruating women 4. Invasive cancer cervix
7.2G Methodology of data collection
Patients attending vani vilas and bowring hospital are selected by random sampling, after fulfilling inclusion and exclusion criteria. Two cervical smears are simultaneously prepared from each enrollee, one of which is processed as a Conventional PAP smear and the other used for an Liquid Based Cytology.
7.2H Statistical analysis
Suitable statistical test will be applied for analysis of data
7.3Does the study require any investigation or intervention to be conducted on patients or other humans or animals? If so please describe briefly. Yes, investigations required are. • Conventional PAP smear cytology • Liquid based cytology
7.4 Has ethical clearance has been obtained from your institution in case of 7.3? No
8. List of references
1. Ferlay J Bray F, Pisani P, et al. GLOBOCAN 2002. Cancer Incidence, Mortality and Prevalence Worldwide International Agency for Research on Cancer. IARC 2002. CA Cancer j Clin. 2005 :74-108.
2. Sankarnarayan R, Buduck AM, Rajkumar R. Effectice screening programmes for cervical cancer in low and middle income developing countries. Bull World Health Organisation 2001; 954-962.
3. Berek and Jonathan S, Berek and Novak`s Gynaecology- 14th edition
4. Nanda K, McCrory DC et al. Accuracy of the Papanicolaou test in screening for and follow-up of cervical cytologic abnormalities: a systematic review. Ann Int Med 2000; 810
5.Sherman ME, Shiffman MH, Lorenz AT, Manos M, Scott DR, Kurman R: Toward objective quality assurance in cervical cytopathology: Correlation of cytopathology diagnosis with liquid based cytology in detection of high risk human papillomavirus types. Am J Clin Path 1994, :182-187.
6 Berek and Hacker's Gynecologic Oncology, 5th Edition, Copyright ©2010, pre invasive disease
7. Jung Dal Lee ,Young-Ha Oh, Seong Ok Lee, Jong Yull Kim: Comparison of Diagnostic Cytomorphology of Atypical Squamous Cells in Liquid-Based Preparations and Conventional Smears
8. Annie N. Y. Cheung, Elaine F. Szeto, Betty S. Y. Leun, Ui-Soon Khoo, Anita W. Y. Ng: Liquid- Based Cytology and Conventional Cervical Smears,a Comparison Study in an Asian Screening Population.
9. Saslow D, Runowicz C, Solomon D, Moscicki AB, Smith RA, Eyre HJ, et al. American Cancer Society cervical cancer screening guidelines 2002. CA Cancer J Clin 2002;:375-376. . 10. National Institute for Clinical Excellence. Guidance on the use of liquid based cytology for cervical screening. London: NICE, 2002. (Technology appraisal guidance No 5.) http://www.nice.org.uk/page.aspx?o=82877
11. Ronco G, Cuzick J, et al. Accuracy of liquid based cytology versus conventional cytology: overall results of the new technologies for cervical screening (NTCC) randomised controlled trial. BMJ 2007:28-31
12. Rockville, Agency for Health Care Policy and Research. Evaluation of cervical cytology: evidence report/technology assessment: AHCPR, January 1999. Online monograph: http://www.ahcpr.gov/clinic/epcsums/cervsumm.htm.
9. Signature of the candidate As the incidence of Cancer Cervix is increasing in our
10. Remarks of the Guide country, we need a better screening test with a greater
sensitivity. This study is carried out to prove the efficacy of
Liquid based cytology over conventional PAP Smear
Dr. Savitha C 11.1 Name and designation of M.D. OBG Professor and Unit Chief Guide Department of Obstetrics and Gynecology Bowring and lady Curzon hospital BMCRI Bangalore
11.2 Signature
12.1 Head of the Department Dr. Malini. K.V. M.D. OBG Professor and H.O.D Department of Obstetrics and Gynecology, BMC & RI Bangalore
12.2 Signature 13.1 Remarks of the, Director cum Dean
13.2 Signature