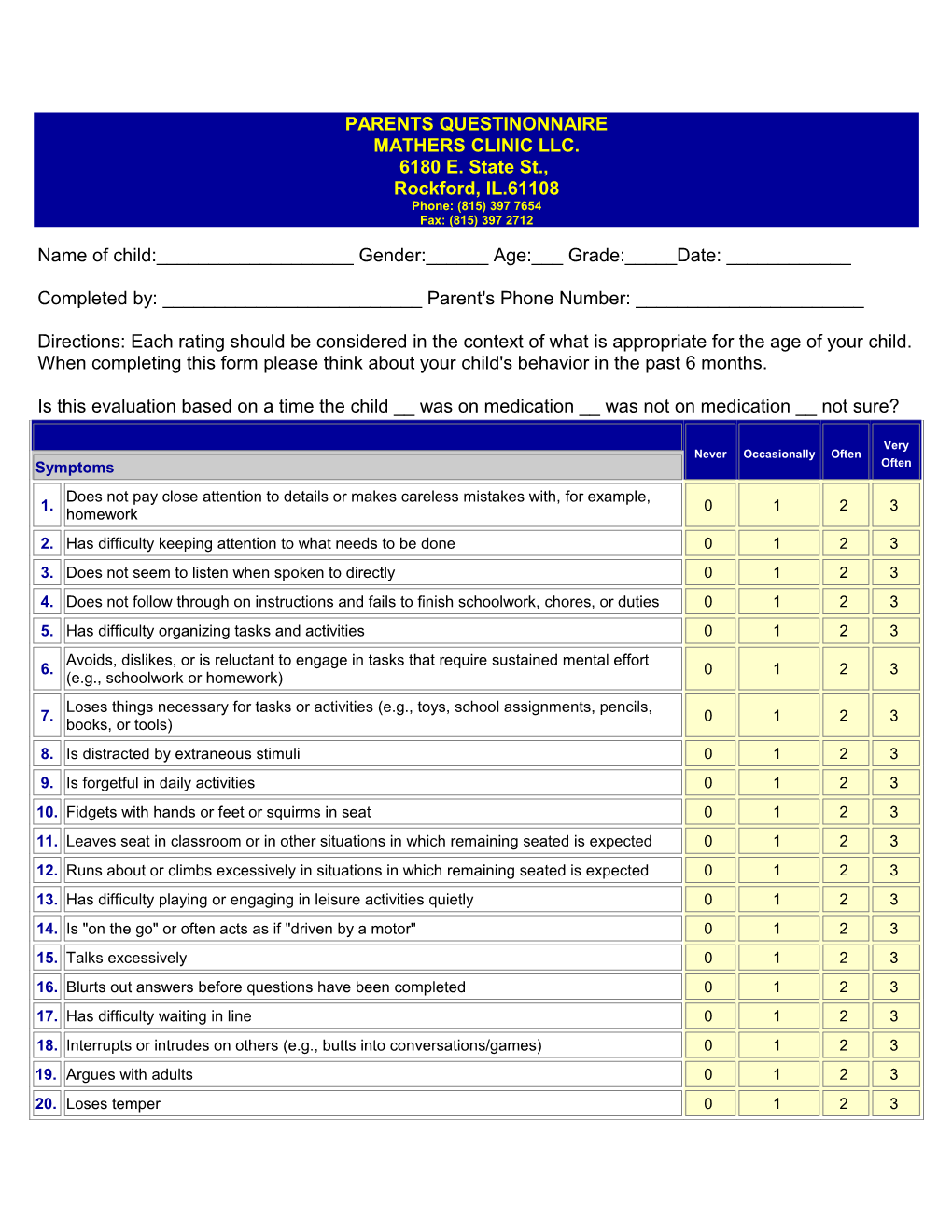
PARENTS QUESTINONNAIRE MATHERS CLINIC LLC. 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712
Name of child:______Gender:______Age:___ Grade:_____Date: ______
Completed by: ______Parent's Phone Number: ______
Directions: Each rating should be considered in the context of what is appropriate for the age of your child. When completing this form please think about your child's behavior in the past 6 months.
Is this evaluation based on a time the child __ was on medication __ was not on medication __ not sure?
Very Never Occasionally Often Symptoms Often Does not pay close attention to details or makes careless mistakes with, for example, 1. 0 1 2 3 homework 2. Has difficulty keeping attention to what needs to be done 0 1 2 3 3. Does not seem to listen when spoken to directly 0 1 2 3 4. Does not follow through on instructions and fails to finish schoolwork, chores, or duties 0 1 2 3 5. Has difficulty organizing tasks and activities 0 1 2 3 Avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort 6. 0 1 2 3 (e.g., schoolwork or homework) Loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, 7. 0 1 2 3 books, or tools) 8. Is distracted by extraneous stimuli 0 1 2 3 9. Is forgetful in daily activities 0 1 2 3 10. Fidgets with hands or feet or squirms in seat 0 1 2 3 11. Leaves seat in classroom or in other situations in which remaining seated is expected 0 1 2 3 12. Runs about or climbs excessively in situations in which remaining seated is expected 0 1 2 3 13. Has difficulty playing or engaging in leisure activities quietly 0 1 2 3 14. Is "on the go" or often acts as if "driven by a motor" 0 1 2 3 15. Talks excessively 0 1 2 3 16. Blurts out answers before questions have been completed 0 1 2 3 17. Has difficulty waiting in line 0 1 2 3 18. Interrupts or intrudes on others (e.g., butts into conversations/games) 0 1 2 3 19. Argues with adults 0 1 2 3 20. Loses temper 0 1 2 3 21. Actively defies or refuses to go along with adult requests or rules 0 1 2 3 22. Deliberately annoys people 0 1 2 3 23. Blames others for his or her mistakes or misbehaviors 0 1 2 3 24. Is touchy or easily annoyed by others 0 1 2 3 25. Is angry or resentful 0 1 2 3 26. Is spiteful and wants to get even 0 1 2 3 27. Bullies, threatens, or intimidates others 0 1 2 3 28. Starts physical fights 0 1 2 3 29. Lies to get out of trouble or to avoid obligations (i.e., "cons" others) 0 1 2 3 30. Is truant from school (skips school) without permission 0 1 2 3 31. Is physically cruel to people 0 1 2 3 32. Has stolen things that have value 0 1 2 3 33. Deliberately destroys others' property 0 1 2 3 34. Has used a weapon that can cause serious harm (bat, knife, brick, gun) 0 1 2 3 35. Is physically cruel to animals 0 1 2 3 36. Has deliberately set fires to cause damage 0 1 2 3 37. Has broken into someone else's home, business or car 0 1 2 3 38. Has stayed out at night without permission 0 1 2 3 39. Has run away from home overnight 0 1 2 3 40. Has forced someone into sexual activity 0 1 2 3 41. Is fearful, anxious, or worried 0 1 2 3 42. Is afraid to try new things for fear of making mistakes 0 1 2 3 43. Feels worthless or inferior 0 1 2 3 44. Blames self for problems, feels guilty 0 1 2 3 45. Feels lonely, unwanted, or unloved; complains that "no one loves him or her" 0 1 2 3 46. Is sad, unhappy, or depressed 0 1 2 3 47. Is self-conscious or easily embarrassed 0 1 2 3
Somewhat Performance Above Excellent Average of a Problematic .. Academic Performance Average Problem 48. Reading 1 2 3 4 5 49. Mathematics 1 2 3 4 5 50. Written expression 1 2 3 4 5 . Classroom Behavioral Performance Excellent Above Average Somewhat Problematic Average of a Problem 51. Relationship with peers 1 2 3 4 5 52. Following directions 1 2 3 4 5 53. Disrupting class 1 2 3 4 5 54. Assignment completion 1 2 3 4 5 55. Organizational skills 1 2 3 4 5
For Office Use Only
Total number of items scored 2 or 3 in items 1-9: _____ (ADHD, predominantly inattentive type—6 or more symptoms)
Total number of items scored 2 or 3 in items 10-18:_____ (ADHD, predominantly hyperactive-impulsive type—6 or more symptoms)
Total number of items scored 2 or 3 for items 1-18:_____ (ADHD, combined type—6 or more symptoms of both types)
Total number of items scored 2 or 3 in items 19-26:_____ (oppositional defiant disorder screen—4 or more symptoms)
Total number of items scored 2 or 3 in items 27-40:_____ (conduct disorder screen—3 or more symptoms)
Total number of items scored 2 or 3 in items 41-47:_____ (anxiety/depression screen—3 or more symptoms)
Scoring Instructions for the Vanderbilt Assessment Scale—Parent Informant
The Vanderbilt Assessment Scale has two components: symptom assessment and impairment of performance.
For the ADHD screen, the symptoms assessment component screens for symptoms that meet the criteria for both inattentive (items 1-9) and hyperactive-impulsive ADHD (items 10-18). To meet DSM-IV criteria for the diagnosis of ADHD, one must have at least 6 responses of "Often" or "Very Often" (scored 2 or 3) to either the 9 inattentive or 9 hyperactive-impulsive items, or both and a score of 4 or 5 on any of the Performance items (48-55). There is a place to record the number of symptoms that meet these criteria in each subgroup.
The Vanderbilt Assessment Scale also contains items that screen for 3 other co-morbidities: oppositional defiant disorder, conduct disorder, and anxiety/depression.
For the oppositional defiant disorder screen there must be a score of 2 or 3 on 4 of the 8 items (19-26) on the subscale and a score of 4 or 5 on any of the Performance items (48-55).
For the conduct disorder screen there must be a score of 2 or 3 on 3 out of the 14 items (27-40) on this subscale and a score of 4 or 5 on any of the Performance items (48-55).
For the anxiety/depression screen there must be a score of 2 or 3 on 3 of the 7 items (41-47) and a score of 4 or 5 on any of the Performance items 48-55).
The Vanderbilt Assessment Scale should NOT be used alone to make a diagnosis. The practitioner must consider information from other sources.
Adapted from the Vanderbilt Rating Scales developed by Mark L. Wolraich, MD. Revised-1102. TEACHERS QUESTIONNAIRE MATHERS CLINIC LLC. 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712
Name of student:______Gender:______Age:___ Grade:_____Date: ______
Completed by: ______Teacher's Phone Number: ______
Directions: Each rating should be considered in the context of what is appropriate for the age of the child and should reflect that child's behavior since the beginning of the school year. Please indicate the number of weeks or months you have been able to evaluate the behaviors: ______
Is this evaluation based on a time the child __ was on medication __ was not on medication __ not sure?
Very Never Occasionally Often Symptoms Often 1. Fails to give attention to details or makes careless mistakes in schoolwork 0 1 2 3
2. Has difficulty sustaining attention to tasks or activities 0 1 2 3
3. Does not seem to listen when spoken to directly 0 1 2 3 Does not follow through on instructions and fails to finish schoolwork 4. 0 1 2 3 (not due to refusal or failure to understand) 5. Has difficulty organizing tasks and activities 0 1 2 3
6. Avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort 0 1 2 3 Loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, 7. 0 1 2 3 or books) 8. Is easily distracted by noises or other stimuli 0 1 2 3
9. Is forgetful in daily activities 0 1 2 3
10. Fidgets with hands or feet or squirms in seat 0 1 2 3
11. Leaves seat in classroom or in other situations in which remaining seated is expected 0 1 2 3
12. Runs about or climbs excessively in situations in which remaining seated is expected 0 1 2 3
13. Has difficulty playing or engaging in leisure activities quietly 0 1 2 3
14. Is "on the go" or often acts as if "driven by a motor" 0 1 2 3
15. Talks excessively 0 1 2 3
16. Blurts out answers before questions have been completed 0 1 2 3
17. Has difficulty waiting in line 0 1 2 3
18. Interrupts or intrudes on others (e.g., butts into conversations/games) 0 1 2 3
19. Loses temper 0 1 2 3
20. Actively defies or refuses to comply with adults' requests or rules 0 1 2 3
21. Is angry or resentful 0 1 2 3
22. Is spiteful and vindictive 0 1 2 3
23. Bullies, threatens, or intimidates others 0 1 2 3
24. Initiates physical fights 0 1 2 3
25. Lies to obtain goods for favors or to avoid obligations (e.g., "cons" others) 0 1 2 3
26. Is physically cruel to people 0 1 2 3
27. Has stolen items of nontrivial value 0 1 2 3
28. Deliberately destroys others' property 0 1 2 3
29. Is fearful, anxious, or worried 0 1 2 3
30. Is self-conscious or easily embarrassed 0 1 2 3
31. Is afraid to try new things for fear of making mistakes 0 1 2 3
32. Feels worthless or inferior 0 1 2 3 33. Blames self for problems; feels guilty 0 1 2 3
34. Feels lonely, unwanted, or unloved; complains that "no one loves him or her" 0 1 2 3
35. Is sad, unhappy, or depressed 0 1 2 3
Somewhat Performance Above Excellent Average of a Problematic .. Academic Performance Average Problem 36. Reading 1 2 3 4 5 37. Mathematics 1 2 3 4 5 38. Written expression 1 2 3 4 5 Somewhat Above . Classroom Behavioral Performance Excellent Average of a Problematic Average Problem 39. Relationship with peers 1 2 3 4 5 40. Following directions 1 2 3 4 5 41. Disrupting class 1 2 3 4 5 42. Assignment completion 1 2 3 4 5 43. Organizational skills 1 2 3 4 5 Comments:
For Office Use Only
Total number of items scored 2 or 3 in items 1-9: ______(ADHD, predominantly inattentive type—6 or more symptoms)
Total number of items scored 2 or 3 in items 10-18:______(ADHD, predominantly hyperactive-impulsive type—6 or more symptoms)
Total number of items scored 2 or 3 for items 1-18:______(ADHD, combined type—6 or more symptoms of both types)
Total number of items scored 2 or 3 in items 19-28:______(oppositional and conduct disorder screen—3 or more symptoms)
Total number of items scored 2 or 3 in items 29-35:______(anxiety/depression screen—3 or more symptoms)
Total number of items scored 2 or 3 in items 36-43:______(academic and classroom behavior symptoms) Scoring Instructions for the Vanderbilt Assessment Scale—Teacher Informant
The Vanderbilt Assessment Scale has two components: symptom assessment and impairment of performance.
For the ADHD screen, the symptoms assessment component screens for symptoms that meet the criteria for both inattentive (items 1-9) and hyperactive-impulsive ADHD (items 10-18). To meet DSM-IV criteria for the diagnosis of ADHD, one must have at least 6 responses of "Often" or "Very Often" (scored 2 or 3) to either the 9 inattentive or 9 hyperactive-impulsive items, or both and a score of 4 or 5 on any of the Performance items (36-43). There is a place to record the number of symptoms that meet these criteria in each subgroup.
The Vanderbilt Assessment Scale also contains items that screen for 3 other co-morbidities: oppositional defiant disorder (items 19-22), conduct disorder (items 23-28), and anxiety/depression (items29-35).
To screen for oppositional defiant disorder/conduct disorder one must have at least 3 responses of "Often" or "Very Often" on items 19- 28 and a score of 4 or 5 on any of the Performance items (36-43).
To screen for anxiety/depression one must have at least 3 responses of "Often" or "Very Often" on items 29-35 and a score of 4 or 5 on any of the Performance items 36-43.
MATHERS CLINIC 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712 SNAP-IV-C Rating Scale
Child's name:______Gender:_____ Age:______Grade:_____Date: ______
Ethnicity (check one which best applies) African-American Asian Caucasian Hispanic Other ______
Completed by:______Type of Class ______Class Size: ______
For each of the 80 items, check the column which best describes this child.
Just a Quite a Very Not at all Items Little Bit Much Often fails to give close attention to details or makes careless mistakes in schoolwork, work, or other 1. activities . . . . Often has difficulty sustaining attention in tasks or play activities 2. . . . . Often does not seem to listen when spoken to directly 3. . . . . Often does not follow through on instructions and fails to finish schoolwork, chores, or duties 4. . . . . Often has difficulty organizing tasks and activities 5. . . . . Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., 6. schoolwork or homework) . . . . Often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, books, or tools) 7. . . . . Often is distracted by extraneous stimuli 8. . . . . Often is forgetful in daily activities 9. . . . . Often has difficulty maintaining alertness, orienting to requests, or executing directions 10. . . . . Often fidgets with hands or feet or squirms in seat 11. . . . . Often leaves seat in classroom or in other situations in which remaining seated is expected 12. . . . . Often runs about or climbs excessively in situations in which it is inappropriate 13. . . . . Often has difficulty playing or engaging in leisure activities quietly 14. . . . . Often is "on the go" or often acts as if "driven by a motor" 15. . . . . Often talks excessively 16. . . . . Often blurts out answers before questions have been completed 17. . . . . Often has difficulty awaiting turn 18. . . . . Often interrupts or intrudes on others (e.g., butts into conversations/games) 19 . . . . Often has difficulty sitting still, being quiet, or inhibiting impulses in the classroom or at home 20. . . . . Often loses temper 21. . . . . Often argues with adults 22. . . . . Often actively defies or refuses adult requests or rules 23. . . . . Often deliberately does things that annoy other people 24. . . . . Often blames others for his or her mistakes or misbehavior 25. . . . . Often touchy or easily annoyed by others 26. . . . . Often is angry and resentful 27. . . . . Often is spiteful or vindictive 28. . . . . Often is negative, defiant, disobedient, or hostile toward authority figures 29. Often teases other children and interferes with their activities 30. Often is aggressive to other children (e.g., picks fights or bullies) 31. . . . . Often is destructive with property of others (e.g., vandalism) 32. . . . . Often is deceitful (e.g., steals, lies, forges, copies the work of others, or "cons") 33. . . . . Often and seriously violates rules (e.g., is truant, runs away, or completely ignores class rules) 34. . . . . Has persistent pattern of violating the basic rights of others or major societal norms 35. . . . . Has episodes of failure to resist aggressive impulses (to assault others or to destroy property) 36. . . . . Has motor or verbal tics (sudden, rapid, recurrent, non-rhythmic motor or verbal activity) 37. . . . . Has repetitive motor behavior (e.g., hand waving, body rocking, or picking at skin) 38. . . . . Has obsessions (a persistent and intrusive inappropriate ideas, thoughts, or impulses) 39. . . . . Has compulsions (repetitive behaviors or mental acts to reduce anxiety or distress) 40. . . . . Often is restless or seems keyed up or on edge 41. . . . . Often is easily fatigued 42. . . . . Often has difficulty concentrating (mind goes blank) 43. . . . . Often is irritable 44. . . . . Often has muscle tension 45. . . . . Often has excessive anxiety and worry (e.g., apprehensive expectations) 46. . . . . Often has daytime sleepiness (unintended sleeping in inappropriate situations) 47. . . . . Often has excessive emotionality and attention-seeking behavior 48. . . . . Often has need for undue admiration, grandiose behavior, or lack of empathy 49. . . . . Often has instability in relationships with others, reactive mood, and impulsivity 50. . . . . Sometimes, for at least a week, has inflated self-esteem or grandiosity 51. . . . . Sometimes, for at least a week, is more talkative than usual or seems pressured to keep talking 52. . . . . Sometimes, for at least a week, has flight of ideas or says that thoughts are racing 53. . . . . Sometimes, for at least a week, has elevated, expansive or euphoric mood 54. . . . . Sometimes, for at least a week, is excessively involved in pleasurable but risky activities 55. . . . . Sometimes, for at least 2 weeks, has depressed mood (sad, hopeless, discouraged) 56. . . . . Sometimes, for at least 2 weeks, has irritable or cranky mood (not just when frustrated) 57. . . . . Sometimes, for at least 2 weeks, has markedly diminished interest or pleasure in most activities 58. . . . . Sometimes, for at least 2 weeks, has psychomotor agitation (even more active than usual) 59. . . . . Sometimes, for at least 2 weeks, has psychomotor retardation (slowed down in most activities) 60. . . . . Sometimes, for at least 2 weeks, is fatigued or has loss of energy 61. . . . . Sometimes, for at least 2 weeks, has feelings of worthlessness or excessive, inappropriate guilt 62. . . . . Sometimes, for at least 2 weeks, has diminished ability to think or concentrate 63. . . . . Chronic low self-esteem most of the time for at least a year 64. . . . . Chronic poor concentration or difficulty making decisions most of the time for at least a year 65. . . . . Chronic feelings of hopelessness most of the time for at least a year 66. . . . . Currently is hyper vigilant (overly watchful or alert) or has exaggerated startle response 67. . . . . Currently is irritable, has anger outbursts, or has difficulty concentrating 68. . . . . Currently has an emotional (e.g., nervous, worried, hopeless, tearful) response to stress 69. . . . . Currently has a behavioral (e.g., fighting, vandalism, truancy) response to stress 70. . . . . Has difficulty getting started on classroom assignments 71. . . . . Has difficulty staying on task for an entire classroom period 72. . . . . Has problems in completion of work on classroom assignments 73. . . . . Has problems in accuracy or neatness of written work in the classroom 74. . . . . Has difficulty attending to a group classroom activity or discussion 75. . . . . Has difficulty making transitions to the next topic or classroom period 76. . . . . Has problems in interactions with peers in the classroom 77. . . . . Has problems in interactions with staff (teacher or aide) 78. . . . . Has difficulty remaining quiet according to classroom rules 79. . . . . Has difficulty staying seated according to classroom rules 80. . . . .
Average Sum of Teacher Rating Per Parent Sections below to be completed by health care provider. Items for 5% Item for 5% Cutoff The following are items that make up various subscales. First four rows provide the cutoffs for ADHD and Each Scale Cutoff ODD subscales. See instructions below for further information. Each Scale Average score for ADHD-Inattention (items 1-9) ______.______2.56 1.78 Average score for ADHD-Hyperactivity-Impulsivity (items 11-19) .______.______1.78 1.44 Average score for ADHD-Combined type (items 1-9 and 11-19) .______.______2.00 1.67 Average score for Oppositional Items (sum of items 21-28) .______.______1.38 1.88 Conduct Disorder (items 31, 32, 33, 34, and 35) .______.______. . Intermittent Explosive Disorder (item 36) .______.______. . Stereotypic Movement Disorder (item 38) .______.______. . Obsessive-Compulsive Disorder (items 39 and 40) .______.______. . Generalized Anxiety Disorder (items 41, 42, 43, 44, 45 and 46) .______.______. . Narcolepsy (item 47) .______.______. . Histrionic Personality Disorder (item 48) .______.______. . Narcissistic Personality Disorder (item 49) .______.______. . Borderline Personality Disorder (item 50) .______.______. . Manic Episode (items 51, 52, 53, 54 and 55) .______.______. . Dysthymic Disorder (items 64, 65, and 66) .______.______. . Posttraumatic Stress Disorder (items 67 and 68) ______.______. . Adjustment Disorder (items 69 and 70) ______.______. . SKAMP Rating Scale (classroom manifestations of core ADHD symptoms) (items 71-80) ______.______
The SNAP-IV-C Rating Scale is a revision of the Swanson, Nolan and Pelham (SNAP) Questionnaire (Swanson et al, 1983). The items from the DSM-IV (1994) criteria for ADHD are included for the two subsets of symptoms: inattention (items # 1-9) and hyperactivity/impulsivity (items # 11-18). Also. Items are included from the DSM-IV criteria for Oppositional Defiant Disorder (items # 21-28) since it often is present in children with ADHD. Items have been added to summarize the Inattention domain (# 10) and the Hyperactivity/Impulsivity domain (# 20) of ADHD. Two other items were added: an item from DSM-III-R (# 29) that was not included in the DSM-IV list for ODD, and an item to summarize the ODD domain (# 30). The 4-point response is scored 0-3 (Not at All=0, Just A Little=1, Quite a Bit=2, and Very Much=3). Subscale scores for the ADHD and ODD subscales on the SNAP-IV are calculated by summing the scores on the items in the specific subset (e.g., Inattention) and dividing by the number of items in the subset (e.g., 9). The score for any subset is expressed as the Average Rating-Per-Item. The 5% cutoff scores for teachers and parents are provided. Compare the Average Rating Per Item score to the cut off score to determine if the score falls within the top 5% of extreme scores. Finally, the SNAP-IV-C includes the 10 items (# 69-78) of the Swanson, Kotkin, Agler, MyInn, and Pelham (SKAMP) Rating Scale. These items are classroom manifestations of inattention, hyperactivity, and impulsivity (i.e., getting started, staying on task, interactions with others, completing work, and shifting activities). The SKAMP may be used to estimate severity of impairment in the classroom.
Adapted from the SNAP-IV-C Rating Scale by James Swanson, UCI, Irvine, CA.
MATHERS CLINIC LLC 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712 ADHD Symptom Checklist—Child and Adolescent Version
Child's Name: ______Age: ____ Grade: ______Gender: ______
Completed by: ______Relationship to child: ______Date: ______
Check the box that describes this child's behavior at home (if you are the child's parent) or at school (if you are the child's teacher) over the past six months. Not at Just a Very Often Inattention Symptoms all little Often 1. fails to give close attention to details or makes careless mistakes in schoolwork, work, or other activities . . . . 2. has difficulty sustaining attention in tasks or play activities . . . . 3. does not seem to listen when spoken to directly . . . . 4. does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions) . . . . 5. has difficulty organizing tasks and activities . . . . 6. avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework) . . . . 7. loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, books, or tools) . . . . 8. is easily distracted by extraneous stimuli . . . . 9. is forgetful in daily activities . . . .
Hyperactivity Symptoms 10. fidgets with hands or feet or squirms in seat . . . . 11. leaves seat in classroom or in situations in which remaining seated is expected . . . . 12. runs about or climbs excessively in situations in which it is inappropriate (in adolescents may be feelings of restlessness) . . . . 13. has difficulty playing or engaging in leisure activities quietly . . . . 14. is “on the go” or often acts as if “driven by a motor” . . . . 15. talks excessively . . . . Impulsivity Symptoms . . . . 16. blurts out answers before questions have been completed . . . . 17. has difficulty awaiting turn . . . . 18. interrupts or intrudes on others (e.g., butts into conversations or games) . . . . At what age did these symptoms first appear? Or when did you notice them? Do these symptoms impair the child’s functioning in two or more settings? (Yes, No, DK) Where is their impairment? Home? School? Work? (list all) Scoring Instructions for the ADHD Symptom Checklist To meet DSM-IV criteria for ADHD, one must have at least 6 responses of "Often" or "Very Often" (scored 2 or 3) to either the 9 inattentive items (1- 9) or 9 hyperactive-impulsive items (10-18), or both. In addition, symptoms must have occurred in childhood, they must impair the child's functioning in two or more settings and they must not be primarily due to any other factors or conditions. MATHERS CLINIC 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712 Childhood Disorders Checklist
Child's name: ______Age: _____ Grade: ______Gender: ____ Date ______
Completed by: ______Relationship to child: ______
Below are lists of behaviors or reactions that describe disorders that may be seen in children and adolescents. Read each list and check the box to the left of the item to indicate whether your child has displayed any of these behaviors or reactions during the period noted for each list.
A. Oppositional Defiant Disorder List Indicate if your child has displayed any of the behaviors listed below within the past six months.
. Often loses temper
. Often argues with adults
. Often defies or refuses to do what you tell him/her
. Often does things to deliberately annoy others
. Often blames others for his/her own mistakes or misbehavior
. Often is touchy or is easily annoyed by others
. Often is angry or resentful
. Often takes anger out on others or tries to get even
Does your child show four or more of these behaviors?
Have these behaviors been exhibited for at least the past six months?
At what age did these behaviors first cause problems for your child? ______(yrs)
Have these behaviors been the cause of problems for your child in any of the following areas? ___Home ___School ___Workplace ___Community
B. Conduct Disorder List Indicate if your child has displayed any of the behaviors listed below within the past six months.
. Often bullies, threatens, or intimidates others
. Often starts physical fights
.. Has used a weapon when fighting (bat, brick, bottle, etc.)
. Has been physically cruel to people
. Has stolen things from others using physical force
. Has stolen things when others were not looking
. Has forced someone into sexual activity
. Has destroyed others’ property (other than by fire setting) . Has broken into someone else’s house, building, or car
. Has not come home overnight at least twice while living in parent’s home, foster care, or group home? If so, how many times?
Is often truant from school? Did this occur before age 13? _____ . If so, at what age? ____ (yrs)
Does your child show three or more of the above behaviors?
Have three of these behaviors occurred during the past 12 months?
Has at least one of these behaviors occurred during the past six months?
Did any of these behaviors occur prior to age ten years?
Have these characteristics been the cause of problems for your child in any of the following areas? ___Home ___School ___Workplace ___Community
C. Attention-Deficit/Hyperactivity Disorder List Indicate if your child has displayed any of the behaviors listed below within the past six months.
Inattention List
Often fails to give close attention to details or makes careless mistakes in schoolwork, . work, or other activities
. Often has difficulty sustaining attention in tasks or play activities
. Often does not seem to listen when spoken to directly
Often does not follow through on instructions and fails to finish schoolwork, . chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions)
. Often has difficulty organizing tasks and activities
Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental . effort (such as schoolwork or homework)
Often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, . books, or tools)
. Is often easily distracted by extraneous stimuli
Is often forgetful in daily activities
Hyperactivity-Impulsivity List
. Often fidgets with hands or feet or squirms in seat
. Often leaves seat in classroom or in other situations in which remaining seated is expected
Often runs about or climbs excessively in situations in which it is inappropriate (in . adolescents or adults, may be limited to subjective feelings of restlessness)
. Often has difficulty playing or engaging in leisure activities quietly
. Is often “on the go” or often acts as if “driven by a motor”
. Often talks excessively
. Often blurts out answers before questions have been completed
. Often has difficulty awaiting turn
. Often interrupts or intrudes on others (e.g., butts into conversations or games) . Does your child show six or more of the behaviors on the inattention list?
. Does your child show six or more of the behaviors on the hyperactive-impulsive list?
At what age did these behaviors first cause problems for this child? ______yrs of age
Have these behaviors existed for at least the past six months? _____ Yes _____ No
Have these behaviors been the cause of problems for your child in any of the following areas? ___Home ___ School ___Workplace ___Community
D. Learning Problems List or Academic Skills Disorder List Indicate if your child has displayed any of the following problems in learning or academic performance compared to other children of his or her age or grade level.
. Recognizing unfamiliar words when reading
. Comprehending the meaning of what he/she reads
. Spelling
. Expressing ideas in writing
. Expressing ideas orally
. Memory
. Handwriting
. Arithmetic computation
. Arithmetic problem solving (word problems)
. Organizing work and homework
. Completing homework on his/her own and in a timely manner
. Excessive absences from school
. Little effort made to achieve up to his/her potential
E. Asperger’s Disorder List Indicate if your child has exhibited any of the following patterns of behavior.
Problems in social interaction as manifested by at least two of the following:
Marked impairment in the use of multiple nonverbal behaviors such as eye-to-eye gaze, . facial expression, body postures, gestures to regulate social interaction
. Failure to develop peer relationships appropriate to developmental level
. Marked impairment in the ability to express pleasure at other people’s happiness
. Lack of social or emotional reciprocity
In addition, which of the following patterns of behavior are exhibited?
. Restricted, repetitive, and stereotyped patterns of behavior, interests, and activities
. Lack of any significant delay in language
Lack of any significant delay in cognitive development. Has age-appropriate self-help skills, adaptive behavior and curiosity about the environment
F. Tourette’s Disorder List Indicate whether your child has exhibited the following tics. A tic is an involuntary, sudden, rapid, recurrent, non-rhythmic, motor movement or vocalization.
. Both multiple motor and one or more vocal tics (not necessarily at the same time)
The tics occur many times a day (usually in bouts), nearly every day or intermittently . throughout a period of more than one year and never stop for more than two months at a time
Describe the tic(s)
G. Chronic Motor or Vocal Tic Disorder List Indicate whether your child has exhibited the following tics.
. Either vocal or motor tics but not both
The tics occur many times a day (usually in bouts), nearly every day or intermittently throughout . a period of more than one year and never stop for more than two months at a time
Describe the tic(s)
H. Transient Tic Disorder List Indicate whether your child has exhibited the following tics. . Single or multiple motor or vocal tics
The tics occur many times a day, nearly every day for at least four weeks, for no longer than . 12 consecutive months
Describe the tic(s)
I. Specific Phobia List Indicate whether your child has exhibited each of the behaviors in this list within the past six months.
Persistent, excessive and unreasonable fear triggered by the presence of, or the anticipation . of, a specific object or situation. For example, in response to, or anticipation of, certain animals, heights, being in the dark, receiving an injection, seeing blood, etc.
Exposure to the feared situation or object almost always produces immediate anxiety. In . children this may be expressed by crying, tantrums, freezing, or clinging
. The fearful situation or object is avoided or else endured with extreme anxiety or distress
Avoidance or anxious anticipation or distress in the feared situation interferes significantly with the child’s normal routine and affects academic functioning, social activities, or relationships with others
Has this fearful or anxious reaction to a situation or object persisted for at least the past 6 months?
Describe the specific situation or object that your child exhibits anxiety to.
J. Separation Anxiety List Indicate whether your child has exhibited each of the behaviors in this list.
Persistent and excessive worry about losing a major attachment figure (e.g., parent, . grandparent, guardian) or of possible harm befalling a major attachment figure Extreme worry that something will occur that will lead to separation from a major attachment . figure (e.g., getting lost or being kidnapped) . Persistent reluctance or refusal to go to school or elsewhere due to fear of separation
. Persistent reluctance to be alone or without major attachment figures at home or in other settings
. Persistent reluctance or refusal to go to sleep without being near a major attachment figure or to sleep away from home
. Re-occurring nightmares having to do with the theme of separation . Repeated complaints of physical symptoms (e.g., headaches, stomachaches, nausea, or vomiting) when separated from a major attachment figure or when separation is anticipated . Re-occurring distress when separation from home or major attachment figures takes place or is anticipated
K. Generalized Anxiety Disorder List Indicate whether your child has exhibited any of the following behaviors or reactions.
. Excessive anxiety and worry occurring more often than not for at least six months
. Child finds it difficult to control the worry
Anxiety and worry are associated with at least three of the following six symptoms:
. Restlessness or feeling keyed up or on edge
. Being easily fatigued
. Trouble with concentration
. Irritability
. Muscle tension
. Trouble falling asleep or staying asleep or restless sleep
L. Obsessive Compulsive Disorder List Indicate whether your child has exhibited any of the following obsessions or compulsions.
Obsessions
Recurrent and persistent thoughts, impulses, or images that are experienced as intrusive and . inappropriate and cause marked anxiety and distress
. The thoughts, impulses or images are not simply excessive worries about real-life problems
The child attempts to ignore or suppress these thoughts or impulses or to “neutralize” them . with some other thought or action
. The child recognizes that the obsessional thoughts, impulses, or images are a product of his/her own mind
Compulsions
Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, . counting, repeating words silently) that the child feels driven to perform in response to an obsession, or according to rules that must be applied rigidly The behaviors or mental acts have the goal of preventing or reducing distress or preventing . some dreaded event or situation; however, these acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive Does the child realize that the obsessions or compulsions are excessive or unreasonable?
Do the obsessions or compulsions cause marked distress; are they time-consuming; or do they significantly interfere with the person’s normal routine or social relationships with others?
M. Dysthymic Disorder List Indicate whether your child has exhibited any of the following reactions.
. Exhibits depressed mood or irritability for most of the day, for more days than not, for at least one year
Presence, while depressed, of at least three of the following:
. Low self-esteem, low self-confidence, or feelings of inadequacy . Feelings of pessimism, hopelessness, or despair
. General loss of interest or pleasure in activities that others of his/her age enjoy
. Little interest in social activities
. Persistent state of fatigue or tiredness
. Feelings of guilt, brooding about the past
. Subjective feelings of irritability or excessive anger
. Decreased activity, drive, or productivity
. Difficulty concentrating, poor memory, or indecisiveness
If your child has exhibited signs of depressed mood, has this created distress for your child or
impairment in any of the following areas? Home School Workplace Community
N. Major Depressive Disorder List Indicate whether your child has exhibited any of the following reactions for at least a two-week period of time.
Depressed or irritable mood most of the day, nearly every day, as indicated by complaints of . feeling sad or appears to be sad or irritable.
. Diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
. Significant weight loss or weight gain when not dieting
. Trouble falling asleep or staying asleep, or excessive sleeping
. Agitated or lethargic (slow moving) nearly every day
. Fatigue or loss of energy nearly every day
. Feelings of worthlessness or excessive or inappropriate guilt nearly every day
. Diminished ability to concentrate or cannot make a decision nearly every day
Repeated thoughts of death (not just fear of dying), repeated suicidal thoughts without a . specific plan or with a plan
O. Bipolar Disorder: Manic Episode List Indicate if your child has ever experienced the following reactions for a period of time that lasted at least one week.
. Mood was abnormally and persistently elevated (he/she felt abnormally happy, giddy, ecstatic)
Mood was abnormally and persistently expansive (he/she felt able to accomplish everything . he/she decided to do and had no limits on his/her abilities to accomplish things)
Mood was abnormally and persistently irritable (he/she was very touchy, easily given to . outbursts of anger or temper, easily annoyed by minor events or by others, or abnormally cranky
If your child exhibited any of the above during the week or more that your child showed this abnormal and persistent mood, mark which of the following behaviors were exhibited? ... Inflated self-esteem or grandiosity
. Decreased need for sleep (e.g., feels rested after only three hours of sleep)
. More talkative than usual or pressure to keep talking
. Thoughts seem to be racing
. Easily distracted (i.e., attention drawn away by unimportant external stimuli) . Increased goal-directed activity; he/she became unusually focused and productive toward one or more tasks
Becomes highly involved in pleasurable activities without regard for negative consequences (e.g., spending excessively, taking risks, etc.) .
Were at least three of the behaviors listed above present? .
Was this disturbance in your child’s mood significant enough to cause marked impairment in social relationships, academic performance, or other . important activities?
Did your child’s abnormal mood result in him/her being hospitalized? .
Did your child have hallucinations or bizarre ideas or feel or act paranoid? .
Explain in more detail. MATHERS CLINIC LLC. 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712 Child and Adolescent Developmental History Form
INSTRUCTIONS:
Please complete the following information about your child and family. If any questions do not apply to your child, simply write “DNA” (does not apply) in the space provided or leave the space blank. It is best if this form is completed by all parents or primary caretakers. This information will be helpful to your child’s doctor or other professionals to better understand your child and your family.
Child’s name: ______Informant: ______Date: ______
Address: ______
Informant’s relationship to child: ______
Child’s age: ______Child’s date of birth: ______Gender: ______
School: ______Grade: ______Phone # of school: ______
Current teacher(s):
______
______
______I. Family Composition Is this child your: biological child, adopted child or foster child? ______Other? ______
With whom does this child live? ______
Who has legal custody of this child? ______
Names and ages of this child’s brothers and sisters or other children in the family:
______
______
II. Current Concerns
What are you most concerned about regarding your child that has led you to complete this history form?
______
______
______
______
______III. Developmental and Medical Information Pregnancy Indicate any complications during pregnancy.
_____ Excessive vomiting. Was hospitalization required? ______
_____ Excessive staining/blood loss? Any infection(s)? Specify ______
_____ Toxemia? Other illnesses? ______
_____ Smoking during pregnancy? # cigarettes smoked per day ______
_____ Alcohol consumption during pregnancy (if beyond an occasional drink)? ______
_____ Other drug use during pregnancy? ______Delivery Type of labor: _____ Spontaneous _____ Induced Duration (hours) ______
Type of delivery: _____ Normal _____ Breech _____ Caesarean
Complications: _____ Cord around neck _____ Hemorrhage _____ Infant injured during delivery
Other: ______Birth weight: ______lbs. ______oz. Post Delivery Period _____ Jaundice _____ Cyanosis (turned blue) _____ Incubator care
Infection (specify) ______Infancy Period Were any of the following presents to a significant degree during the first few years of life? If so, describe: _____ Did not enjoy cuddling______
_____ Was not calmed by being held or stroked ______
_____ Difficult to comfort ______
_____ Colic ______
_____ Excessive restlessness ______
_____ Excessively irritable ______
_____ Diminished sleep ______
_____ Frequent head banging ______
_____ Difficulty nursing ______
_____ Constantly into everything ______
Developmental Milestones Indicate below whether this child achieved the following developmental milestones at a normal age, early, or later than others his/her age.
Smiled: _____ early _____ normal age _____ later than normal
Sat without support: _____ early _____ normal age _____ later than normal
Crawled: _____ early _____ normal age _____ later than normal
Stood without support: _____ early _____ normal age _____ later than normal
Spoke first words: _____early _____normal age _____ later than normal
Said phrases: _____ early _____ normal age _____ later than normal
Said sentences: _____ early _____ normal age _____ later than normal
Bladder trained, all day: _____ early _____ normal age _____ later than normal
Bladder trained, at night: _____ early _____ normal age _____ later than normal
Bowel trained: _____ early _____ normal age _____ later than normal Rode tricycle: _____ early _____ normal age _____ later than normal
Rode bicycle (without training wheels): _____ early _____ normal age _____ later than normal
Buttoned clothing: _____ early _____ normal age _____ later than normal
Tied shoelaces: _____ early _____ normal age _____ later than normal
Named colors: _____ early _____ normal age _____ later than normal
Recited alphabet in order: _____ early _____ normal age _____ later than normal
Began to read: _____ early _____ normal age _____ later than normal Medical History If your child’s medical history includes any of the following, please note the age when the incident or illness occurred and any other pertinent information.
Childhood diseases (age and complications if any) ______
______
______
Operations ______
Hospitalizations ______
Head injuries ______
Convulsions with fever ______without fever ______
Coma ______
Vision problems ______Hearing problems ______
Allergies or asthma ______
Poisoning ______Sleep problems ______
Appetite ______Growth problems ______
Other medical information that is relevant ______
______
Height ______Weight ______Present illnesses for which the child is being treated:
______
______
Psychotropic medications (stimulants, medications for ADHD, mood, anxiety medications) child has been taking or is currently taking. Include name of medication and dosing. a. current medications:______b. previous medications: ______
Describe any benefit from these medications or adverse effects: ______
______
______
Has your child ever received treatment by a mental health professional? If so, who provided this treatment, when, and what was the purpose of the treatment?
______
______
______IV. Family Information
Use the checklists below to describe any family history of psychiatric and learning problems (in child’s parents, grandparents, or siblings).
Aggressiveness, defiance: ___not a problem ___a problem (specify who)______
Difficulties with attention/hyperactivity as a child: ___not a problem ___a problem (specify who)______
Learning problems: ___not a problem ___a problem (specify who)______
Failed to graduate from high school: ___not a problem ___a problem (specify who)______
Mental retardation: ___not a problem ___a problem (specify who)______
Psychosis or schizophrenia: ___not a problem ___a problem (specify who)______
Depression: ___not a problem ___a problem (specify who)______
Anxiety: ___not a problem ___a problem (specify who)______
Tics or Tourette’s syndrome: ___not a problem ___a problem (specify who)______
Alcohol abuse/substance abuse: ___not a problem ___a problem (specify who)______
Antisocial behavior (assaults, thefts, etc.): ___not a problem ___a problem (specify who)______Arrests: ___not a problem ___a problem (specify who)______
Physical abuse/sexual abuse: ___not a problem ___a problem (specify who)______V. School Information
List the name of each school your child has attended from preschool on. kg______7th ______
1st______8th______
2nd ______9th ______
3rd ______10th ______
4th______11th ______
5th______12th______
6th______After 12th______
In general, describe your child's performance during elementary school. Go grade by grade, if necessary, and list any outstanding strengths or problems.
______
______
______
______
______
Describe your child's performance during middle school and high school. Again, go grade by grade, if necessary, and list any outstanding strengths or problems. ______
______
______
______
______
Has your child ever had to repeat a grade? ______If so, which grade? ______
Has your child ever received special education services? ______If so, what grades? ______
Does your child currently have an IEP from his/her school? ______
Does your child currently have a 504 Plan at school? ______Describe the main focus of your child’s IEP or 504 Plan (note accommodations your child is currently receiving).
______
______
______
______
Indicate if your child’s teacher(s) describe any of the following as significant classroom problems.
____ Doesn’t sit still in his or her seat
____ Frequently gets up and walks around the classroom
____ Shouts out. Does not wait his/her turn to be called on
____ Does not cooperate well in group activities
____ Typically does better in a one to one relationship
____ Does not respect the rights of others
____ Does not pay attention during lessons
____ Fails to finish assigned class work
____ Fails to finish assigned homework
____ Bullies other children
____ Is not sought out by others to play or work together
____ Describe any problems your child may have in school with learning.
____ Describe any problems your child may have with homework (e.g., forgets, does not return it to school, etc.)
VI. Child Management Techniques
When your child is disruptive or misbehaves, what steps are you likely to take to deal with the problem and how well do they work?
______
______
______
______
Describe any differences or similarities between each parent's management styles in handling disruptive behavior.
______
______
______
______
Describe what steps you might take to improve your management style in handling disruptive behavior.
______
______
______
______
VII. Strengths and Accomplishments
We realize that we have focused largely on problems that your child may be having. However, we are also quite interested in understanding your child’s strengths, talents, skills, and accomplishments. Please use the space below to describe these assets and use additional pages if necessary.
______
______
______
______
______
______
______
______MATHERS CLINIC LLC 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654Fax: (815) 397 2712 Novotni Social Skills Checklist—Self-Report
Name:______Age:______Date:______
TRAITS: How many of the following traits of highly likeable people are descriptive of you? Circle all that apply. Put a check by the ones you would like to work on.
sincere honest understanding loyal responsible friendly
truthful trustworthy intelligent warm unselfish trustful
thoughtful considerate reliable kind humorous cheerful Not a Problem Needs SKILLS: Use the following checklist to identify strengths as well as areas to work on. Improvement .. .. I. BASIC Manners: The ability to do the following in social interactions. . . Use mannerly words like please, thank you, and you’re welcome . . Express appreciation . . Receive compliments without discounting . . Give compliments regularly to others . . Apologize . . Accept the apology of others . . Introduce yourself . . Introduce others . . Use appropriate greetings . . Use appropriate ending comments . . Phone manners . . Mealtime behaviors (follow lead of host/hostess, chew with mouth closed, not open . . Ask to have items passed, use napkins, elbows off the table, ask to be excused . . Making others feel comfortable in your home—hosting . . Offer to help others . . II. VERBAL COMMUNICATION SKILLS: In conversation with others the ability to: . . Join a conversation without disruption . . Check—repeat what you heard and ask if you heard it right . . Identify and reflect content of conversation—tracking . . Identify and reflect feelings of others . . Reflect content + feelings in conversations . . Use minimal encouragers to let others know you are following the conversation . . Use open questions to keep conversations going . . Ask for help when needed or desired . . III.NONVERBAL COMMUNICATION SKILLS: Looking attentive when listening. When talking with others do you: . . Keep an open posture . . Face the person . . Lean forward . . Maintain appropriate eye contact . . Look relaxed . . IV.COMMUNICATION ROADBLOCKS . . Miss pieces of information—”blinks” . . Use closed or naked questions . . Voice too loud or too soft . . Speak too quickly . . Interrupt others . . Too quiet—rarely speaking in conversations . . Talk excessively . . Order or boss others . . Criticize—judge or evaluate others . . Minimize or not be considerate . . V.ORGANIZATIONAL SKILLS—TRUSTWORTHY . . Difficulty with deadlines . . Difficulty being on time for meetings and appointments . . Difficulty remembering special occasions . . Too organized, rigid . . Difficulty managing money, bills, bank accounts, etc. . . Difficulty organizing your stuff . . Do what you agree to do . . Finish projects . . VI.SELF CONTROL . . Take turns/wait . . Ability to handle . . Effectively manage conflict, negotiate, and compromise . . Effectively manage anger . . Refrain from aggressive behavior . . Assertiveness . . Impulsive spending . . Impulsive decision-making . . Filter thoughts avoiding impulsive words—blurting out things that hurt people . . Inappropriate touching of others . . Difficulty relaxing . . Excessive physical activity (trouble staying seated, fidgeting, feeling restless) . . VII. KNOWLEDGE . . Understand attribution theory’s role in social relationships . . Understand the importance of social exchange theory—give and take in relationships . . Understand the subtle cues that you give others with your body language . . Ability to pick up the subtext—socially perceptive . . Understand context . . VIII. RELATIONSHIPS . . Sensitive to the needs of others . . Patient . . Creative . . Fun to be with . . Flexible—able to go with the flow . . Respect boundaries of others . . Treat others with respect . . Tolerance to differences of others . . Initiate invitations to others . . Difficulty with intimacy . . Have at least three close friends .. .. IX.SELF CARE . . Ability to nurture yourself . . Appearance—clean, neat, and appropriate for situations . Ability to identify and express your feelings . . Self-esteem . . Participate in support groups . . Sense of humor . . Positive outlook—hope .. SKILL AREAS TO WORK ON: Check the box to the left of each skill area that you want to work on. . Basic Manners . Verbal Communication Skills . Nonverbal Communication Skills . Communication Roadblocks . Organizational Skills . Self-control . Knowledge . Relationships
MATHERS CLINIC LLC. Novotni Social Skills Checklist-Observer Version
Name of Rater:______Name of Person Rated: ______Date:______
TRAITS: How many of the following traits of highly likeable people are descriptive of the person being rated? Circle all that apply. Put a check by the ones you would like to see him/her work on.
sincere honest understanding loyal responsible friendly
truthful trustworthy intelligent warm unselfish trustful
thoughtful considerate reliable kind humorous cheerful Not a Needs SKILLS: Use the following checklist to identify strengths as well as Problem Improvement areas to work on that you have observed. Leave blank if not observed. . . I. Basic Manners: The ability to do the following in social interactions. . . Uses mannerly words like please, thank you, and you’re welcome . . Expresses appreciation . . Receives compliments without discounting . . Gives compliments regularly to others . . Apologizes . . Accepts the apology of others . . Introduces him/herself . . Introduces others . . Uses appropriate greetings . . Uses appropriate ending comments . . Phone manners . . Mealtime behaviors (follows lead of host/hostess, chews with mouth closed not open) . . Asks to have items passed, use napkins, elbows off the table, ask to be excused . . Makes others feel comfortable in their home—hosting . . Offers to help others . . II. VERBAL COMMUNICATION SKILLS: In conversation with others the ability to: . . Joins a conversation without disruption . . Checks—repeats what they heard and asks if they heard it right . . Identifies and reflects content of conversation—tracking . . Identifies and reflects feelings of others . . Reflects content + feelings in conversations . . Uses minimal encouragers to let others know they are following the conversation . . Uses open questions to keep conversations going . . Asks for help when needed or desired III.NONVERBAL COMMUNICATION SKILLS: Looking attentive when . . listening. When talking with others do you: . . Keeps an open posture . . Faces the person . . Leans forward . . Maintains appropriate eye contact . . Looks relaxed . . IV.COMMUNICATION ROADBLOCKS . . Misses pieces of information—”blinks” . . Uses closed or naked questions . . Voice too loud or too soft . . Speaks too quickly . . Interrupts others . . Too quiet—rarely speaking in conversations . . Talks excessively . . Orders or bosses others . . Criticizes—judges or evaluates others . . Minimizes or is not considerate . . V.ORGANIZATIONAL SKILLS—TRUSTWORTHY . . Difficulty with deadlines . . Difficulty being on time for meetings and appointments . . Difficulty remembering special occasions . . Too organized, rigid . . Difficulty managing money, bills, bank accounts, etc. . . Difficulty organizing their stuff . . Does what they agree to do . . Finishes projects . . VI.SELF CONTROL . . Take turns/wait . . Ability to handle . . Effectively manage conflict, negotiate and compromise . . Effectively manage anger . . Refrains from aggressive behavior . . Assertiveness . . Impulsive spending . . Impulsive decision-making . . Filters thoughts avoiding impulsive words—blurting things that hurt people . . Inappropriate touch of others . . Difficulty relaxing . . Excessive physical activity (trouble staying seated, fidget, feeling restless) . . VII. KNOWLEDGE . . Understands attribution theory’s role in social relationships . . Understands the importance of social exchange theory—give and take in relationships . . Understands the subtle cues that they give others with their body language . Ability to pick up the subtext—socially perceptive . Understands context . . VIII. RELATIONSHIPS . . Sensitive to the needs of other . . Patient . . Creative . . Fun to be with . . Flexible—able to go with the flow . . Respects boundaries of others . . Treats others with respect . . Tolerance to differences of others . . Initiates invitations to others . . Difficulty with intimacy . . Has at least three close friends . . IX.SELF CARE . . Ability to nurture themselves . . Appearance—clean, neat, and appropriate for situations . . Ability to identify and express their feelings . . Self-esteem . . Participates in support groups . . Sense of humor . . Positive outlook—hope SKILL AREAS TO WORK ON: Check the box to the left of each skill area that you think is important . for this person to work on. . Basic Manners . Verbal Communication Skills . Nonverbal Communication Skills . Communication Roadblocks . Organizational Skills . Self-control . Knowledge . Relationships . Self-care
MATHERS CLINIC LLC. 6180 e. State St., Rockford, IL.61108 Phone: (815) 397 7654Fax: (815) 397 2712 Weekly ADHD Monitoring Form
Child's name: ______Teacher:______Date:______
Teacher: Please answer the items below on your observations of this child during the past week. Note that for items 1-12, high scores indicate problems while for items 13-15, low scores indicate problems. Not at Just a Very Weekly ADHD Monitoring Form Often all little Often
1. fidgets with hands or feet and squirms in seat . . . .
2. difficulty remaining seated . . . .
3. difficulty awaiting turn . . . .
4. always "up and on the go" or acts as if "driven by a motor" . . . .
5. talks excessively . . . .
6. interrupts or intrudes on others . . . .
7. easily distracted . . . .
8. fails to finish assigned tasks . . . .
9. difficulty sustaining attention . . . . 10. careless or messy work . . . .
11. does not seem to listen when spoken to . . . .
12. difficulty following directions . . . .
13. follows class rules . . . .
14. gets along with peers . . . .
15. seems happy and in a good mood . . . .
16. Indicate how the behaviors rated on the other side compared during the morning and afternoon times during the prior week by checking one of the choices below. (Note: If you only have this child in class during morning or afternoon this does not apply) ___morning better than afternoon ___no clear difference ___afternoon better than morning
17. Indicate the approximate percentage of assigned class work that this child completed during the past week: ______0% 20% 40% 60% 80% 100%
18. The general quality of work completed by this child this week was: ___ very poor ___poor ___satisfactory ___good ___very good
19. If the quality of this child's work varied significantly between subjects, please indicate this below.
20. Did this child turn in all assigned homework? If not, please indicate the assignments that were missing.
21. Please include any other comments or observations that you believe are important.
MATHERS CLINIC LLC 6180 E. State St., Rockford, IL.61108 Phone: (815) 397 7654 Fax: (815) 397 2712
ADHD MONITORING SYSTEM A Systematic Guide to Monitoring School Progress for Children with ADHD David L. Rabiner, Ph.D.
Welcome to the ADHD Monitoring System One of the most important things you can do to help promote your child’s healthy development is to carefully monitor how he or she is doing at school. The ADHD Monitoring System will help make it easy for you to do this. By using this program, you will be able to carefully track how your child is doing in school, and will be alerted to when any adjustments or modifications to your child’s treatment need to be discussed with your child’s doctor.
This packet contains a sample monitoring form and the instructions you need to interpret the information this form provides. You may make as many copies of this form as you need for your own use. Thus, you will be able to use this program to monitor and track your child’s progress over the entire course of his or her schooling. It is recommended that you make a number of copies and give them to your child’s teacher so they are readily available for him or her to complete. If your child has multiple teachers, copies should be provided to each of them.
In my own experience, I have found that this program works best with elementary school children who have only a single teacher. This program can also be quite helpful for children who are in middle school or high school, although teachers in these grades may not spend enough time with a student to provide ratings that are as reliable. You will have to see how this works in your own situation.
I want to stress that by using this program to keep careful track of how your child is performing at school, you will be in excellent position to help promote your child’s success. Many times in my own practice, I have spoken with parents who are frustrated by the lack of communication from their child’s teacher, and with not learning about problems until weeks after they begin. Using this system will prevent this from happening to you, and will provide you and your child’s physician with information that can be essential in planning and modifying your child’s treatment.
Instructions for Using the ADHD Monitoring System The ADHD Monitoring System provides an easy and systematic way to monitor how a child with ADHD is doing each week at school in several important areas. By using this system you will be alerted to difficulties that may develop so that adjustments to your child’s treatment can be made in a timely manner. The program will also help you to evaluate the effectiveness of any such adjustments that are made. Guidelines for using this program effectively are presented below.
For this system to be of the greatest benefit to your child, the cooperation and support of your child’s teacher is ESSENTIAL.
You will be asking your child’s teacher to complete the weekly rating form contained in this packet at the end of each week, and should provide the teacher with a sufficient number of copies. Completing this form should not require more than 10-15 minutes of the teacher’s time, and you should discuss this with him or her to make sure the teacher understands the importance of the information they will be providing. Rather than just having your child gives the forms to the teacher along with a note, it is suggested that you discuss this with the teacher on the phone or in person.
The teacher needs to understand that the information he or she provides will help to determine when any changes/additions to treatment need to be made, and that without this input, it will be extremely difficult to know how well your child’s ADHD symptoms are being managed.
NOTE: If your child has multiple teachers, you can provide copies to each teacher who spends a significant amount of time with your child each week.
In discussing this program with the teacher, be sure that arrangements are clearly made to insure that you will be getting the completed form each week. The information won’t do you or your child any good if it sits in the classroom for weeks before you receive it.
What Information is Provided? The ADHD Monitoring System is designed to provide you with information on: • how well your child’s ADHD symptoms are being managed; • your child’s behavioral, social, and emotional functioning at school; • your child’s weekly academic performance. Please refer to the Weekly Monitoring Form when reviewing the information below.
How well are ADHD symptoms being managed? Questions 1-12 deal specifically with symptoms of ADHD. Items 1-6 ask for teacher ratings of hyperactive/impulsive symptoms and items 7-12 provide information on inattentive symptoms.
For children without ADHD, the vast majority of the ratings on these items will be either 0 or 1. For a child with ADHD whose symptoms are being managed effectively—via medication or some other means—you would also expect to see a majority of 0’s and 1’s being circled. NOTE: Not all children with ADHD display both inattentive symptoms and hyperactive/impulsive symptoms. For example, children diagnosed with ADHD Predominantly Inattentive Type display primarily problems with attention (i.e. items 7-12) and do not show many of the hyperactive/impulsive characteristics (i.e. items 1-6). Conversely, children with ADHD, Predominantly Hyperactive/Impulsive Type show the reverse pattern. Thus, should your child have one of these subtypes of ADHD, rather than the Combined subtype in which both sets of symptoms are present, you would look specifically at the appropriate symptom group to determine how well the difficulties are being managed.
Behavioral, social, and emotional functioning Items 13-15 provide a simple screening for behavioral, social, or emotional difficulties. In addition to seeing mostly low scores for items 1-12, you want to see high scores (i.e. 3’s or 4’s) for these items. If your child receives low scores (i.e. 0’s or 1’s) on any or all of these items, you will want to contact the teacher to obtain more detailed information about the difficulties that were observed.
NOTE: It is important to emphasize that these items provide only a simple screen for behavioral, social, and emotional difficulties and are not intended to provide a comprehensive assessment. Although teachers are generally in an excellent position to comment on how a child is following classroom rules (i.e. item 13), they can be less aware of how a child is doing socially (i.e. item 14) or how a child is feeling (i.e. item 15). Thus your child’s teacher may report that your child is doing well in these areas when this is not necessarily the case. Learning about these areas in a comprehensive way requires feedback from your child as well.
Academic performance The reverse side of the rating form provides important information on your child’s academic performance during the prior school week. Information is provided on the amount of assigned work completed, the general quality of the work completed (and whether this varies by subject), and also alerts you to homework assignments that may not have been turned in. Obviously, the ideal is for your child to be completing all assigned work, for it to be of good to very good quality, and for no homework assignments to have been missing.
Suggested guidelines for using the information The information contained in the weekly monitoring form is designed to provide you and your child’s physician with the data you need to make informed decisions about the effectiveness of your child’s treatment and when any treatment modifications appear necessary.
In reviewing this data, it is important to stress that any child can have an occasional bad week. If your child has been doing well, and then has a week where the teacher’s ratings indicate difficulties in one or more areas, this should not necessarily cause alarm nor indicate the need for treatment changes. In general, treatment modifications for a child who has been doing well would not be suggested unless the problems persist for several weeks in succession. (When this occurs, changes in the child’s environment that may be related to a sudden increase in difficulties also need to be considered.) You should also consider modifying treatment if troublesome weeks start to occur with increased frequency (i.e. instead of one bad week every couple of months you start to see several bad weeks each month).
With this important caution in mind, a simple and reasonable framework for evaluating the information contained in the Weekly Monitoring Form is to consider the ADHD symptom ratings (i.e. items 1-12) and the other information separately. When done in this way, several different combinations are possible. These are discussed below.
Everything going well This is what you hope to see each week. In this scenario, ratings of ADHD symptoms (items 1-12) are primarily or exclusively 0’s and 1’s, ratings for items 12-15 indicate that your child is following rules, getting along with peers, and appearing happy. In addition, academic ratings would show that your child is completing all or almost all assigned work and the work is of good quality.
When this is the case, it indicates that your child is doing a great job at school, and that whatever treatments and/or support are in place are working well. No changes or adjustments are indicated.
Everything going poorly At the other extreme is a situation where nothing is going well. Ratings of ADHD symptoms are high, problems with behavior, peer relations, and/or mood are also evident, and both the quantity and quality of assigned work being completed is problematic.
In almost all cases, this indicates a situation where changes and adjustments (i.e. to medication, behavioral plan, etc.) need to be implemented. The only exception would be if, as noted above, your child has been doing consistently well and then has a bad week. If this is the case, it is still important to speak with your child and his or her teacher to try and learn what may have accounted for the difficult week. Should things get back to normal the following week, there is probably no need to change anything. If the difficulties persist, however, it will be important to consider modifications that may be necessary. Consulting with your child’s physician and/or a child mental health professional about the most appropriate steps to pursue is strongly recommended.
ADHD symptoms under control, but problems with behavior, peer relations, mood, or academics. This would be indicated when ratings of ADHD symptoms on items 1-12 are fine (i.e. mostly 0’s and 1’s) but problems are indicated in one or more of these other areas. When ADHD symptom ratings are low, these other problems are unlikely to be direct results of ADHD, but may reflect additional difficulties. Such difficulties can occur for a variety of reasons and it is very important to learn what factors are contributing to the difficulties your child is having. Once again, consulting with your child’s physician and/or a child mental health professional is recommended.
NOTE: When children are in middle school or high school and have multiple teachers, teachers often do not spend enough time with the child to observe problems with regards to ADHD symptoms. In these grades, it is more common for ADHD symptom ratings to look okay, but for the difficulties to show up in academic performance and/or behavior. It is important to be aware of this because the teachers’ ratings may suggest that primary ADHD symptoms are being managed well when this is not the case. If this is true, efforts to manage the inattentive and/or hyperactive/impulsive symptoms more effectively will often be an important first step to take.
Other areas look good but ratings of ADHD symptoms are high. This would be indicated when ratings on items 1-12 include multiple 2’s and 3’s but significant problems with behavior, peer relations, mood, or academics are reported. This is probably the most unusual combination because when a child’s ADHD symptoms are not being managed well, significant problems in behavioral, emotional, social, and/or academic functioning are usually also evident.
Should this pattern persist for more than one week, some adjustment in the treatment being used to manage primary ADHD symptoms is likely to be necessary (i.e. medication adjustment, revising behavior plan). Of course, if a child continues to do well academically, socially, and behaviorally at school, despite high levels of ADHD symptoms, it may not be necessary to change anything. Generally, however, one would expect problems in these areas to emerge if ADHD symptoms are not being managed well for a sustained period. Again consulting with your child’s physician is strongly recommended.
NOTE: The first question on side 2 of the Weekly Monitoring Form asks for the teacher’s impression of how morning and afternoon periods compared. If your child is taking medication, and is receiving a longer acting stimulant or is taking a second dose during the day at school, morning and afternoon behavior would not be expected to differ.
If your child is receiving only a single dose in the morning, however, and the teacher’s ratings indicate that mornings are consistently better than the afternoons, it may indicate that the medication is wearing off during the day and that a single dose is not sufficient. If this pattern emerges in the teacher’s ratings, you should discuss this issue with your child’s physician. There can be other reasons, of course, for why a child’s behavior and schoolwork can vary between mornings and afternoon. For example, it may be that the type of classes and/or activities are consistently different during these periods, and your child has a much easier time with one set of activities/classes than the other. Once again, the important task will be to try and learn why your child is having a harder time with one part of the day than the other, and then determine what type(s) of assistance may be necessary to help with the more difficult time.
How to Reevaluate a Child’s Need for Medication
If your child is taking medication as part of his or her treatment, it is important to be aware that a child’s need for medication can change over time. Because of this, it is generally recommended that this be reevaluated on an annual basis. This should be done at a time when a child’s symptoms appear to be under good control, and things have been stable and going reasonably well for a sustained period. It should not be done at the very beginning of a new school year because children generally require a month or so to settle in to a new classroom. In addition, the teacher needs some time to get to know your child.
To use the monitoring program to reevaluate your child’s need for medication, you simply need to pick a week where your child does not receive any medication for the week, and then compare the teacher’s ratings for this week with the ratings your child had been receiving when on medication. (Note: Prior to doing this it is important that you discuss this with your child’s physician.)
For children who continue to require medication, you would expect to see a clear increase in ADHD symptom ratings (i.e. instead of mostly 0’s and 1’s you would see more 2’s and 3’s for the week without medication). Problems with following class rules may be reported and the amount and quality of assigned work completed would also be expected to show a decline.
NOTE: When you do this reevaluation, it is generally better if your child’s teacher does not know that your child is not receiving medication during the week. This is because if the teacher is aware of this, he or she may “expect” to see problems, and have a hard time providing objective ratings as a result.
If your child is not receiving a second dose during the school day, keeping the teacher “blind” to the medication holiday is not a problem. (Just ask your child not to tell the teacher that he or she is not getting medication that week. Alternatively, you can speak with your child’s doctor about using a “placebo”—i.e. something that looks like medication but is really not—for this week.) If your child receives a second dose during the day, however, it can be a good idea for this dose to continue during the reevaluation week. In this case, the teacher should be instructed to base the ratings for this week during the morning periods only—the time when your child would not be on the medication.
IMPORTANT: If your child appears to do quite well during the week without medication (i.e. no clear change in the ratings provided by the teacher), he or she may not need to continue taking it. This decision should be made in consultation with your child’s physician and it is recommended that you do not discontinue medication or change the dose that your child receives without the doctor’s approval.
Even if you and your child’s physician elect to discontinue medication because your child did well without it, it is very important to continue to use the Weekly Monitoring Form to keep careful track of how your child is doing each week. It is not uncommon, for example, for a child to do fairly well during a one-week break from medication, but to have a difficult time sustaining this good performance. Thus, do not be surprised if you see symptoms reemerge after a short period of time. Should this occur, it may be necessary to resume medication that your child had been taking and this should be discussed with your child’s physician. The important point is that a single good week without medication in no way means that medication may not be necessary again at some point later on and that carefully monitoring how your child does on a weekly basis is essential. Conclusion
I hope that the instructions above have provided you with a good understanding about how to use the ADHD Monitoring System to carefully follow how your child is performing at school. If you enlist the cooperation of your child’s teacher(s), and use this program as outlined above, you will be in a much better position to make well informed decisions about the effectiveness of your child’s treatment, and to know when changes and adjustments are indicated.
The ADHD Monitoring System by David Rabiner, Ph.D.