Infertility Testing and Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Efficacy of Texture and Color Enhancement Imaging In
www.nature.com/scientificreports OPEN Efcacy of Texture and Color Enhancement Imaging in visualizing gastric mucosal atrophy and gastric neoplasms Tsubasa Ishikawa1, Tomoaki Matsumura1*, Kenichiro Okimoto1, Ariki Nagashima1, Wataru Shiratori1, Tatsuya Kaneko1, Hirotaka Oura1, Mamoru Tokunaga1, Naoki Akizue1, Yuki Ohta1, Keiko Saito1, Makoto Arai1,2, Jun Kato1 & Naoya Kato1 In 2020, Olympus Medical Systems Corporation introduced the Texture and Color Enhancement Imaging (TXI) as a new image-enhanced endoscopy. This study aimed to evaluate the visibility of neoplasms and mucosal atrophy in the upper gastrointestinal tract through TXI. We evaluated 72 and 60 images of 12 gastric neoplasms and 20 gastric atrophic/nonatrophic mucosa, respectively. The visibility of gastric mucosal atrophy and gastric neoplasm was assessed by six endoscopists using a previously reported visibility scale (1 = poor to 4 = excellent). Color diferences between gastric mucosal atrophy and nonatrophic mucosa and between gastric neoplasm and adjacent areas were assessed using the International Commission on Illumination L*a*b* color space system. The visibility of mucosal atrophy and gastric neoplasm was signifcantly improved in TXI mode 1 compared with that in white-light imaging (WLI) (visibility score: 3.8 ± 0.5 vs. 2.8 ± 0.9, p < 0.01 for mucosal atrophy; visibility score: 2.8 ± 1.0 vs. 2.0 ± 0.9, p < 0.01 for gastric neoplasm). Regarding gastric atrophic and nonatrophic mucosae, TXI mode 1 had a signifcantly greater color diference than WLI (color diferences: 14.2 ± 8.0 vs. 8.7 ± 4.2, respectively, p < 0.01). TXI may be a useful observation modality in the endoscopic screening of the upper gastrointestinal tract. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Impact of Infection on the Secretory Capacity of the Male Accessory Glands
Clinical�������������� Urolo�y Infection and Secretory Capacity of Male Accessory Glands International Braz J Urol Vol. 35 (3): 299-309, May - June, 2009 Impact of Infection on the Secretory Capacity of the Male Accessory Glands M. Marconi, A. Pilatz, F. Wagenlehner, T. Diemer, W. Weidner Department of Urology and Pediatric Urology, University of Giessen, Giessen, Germany ABSTRACT Introduction: Studies that compare the impact of different infectious entities of the male reproductive tract (MRT) on the male accessory gland function are controversial. Materials and Methods: Semen analyses of 71 patients with proven infections of the MRT were compared with the results of 40 healthy non-infected volunteers. Patients were divided into 3 groups according to their diagnosis: chronic prostatitis NIH type II (n = 38), chronic epididymitis (n = 12), and chronic urethritis (n = 21). Results: The bacteriological analysis revealed 9 different types of microorganisms, considered to be the etiological agents, isolated in different secretions, including: urine, expressed prostatic secretions, semen and urethral smears: E. Coli (n = 20), Klebsiella (n = 2), Proteus spp. (n = 1), Enterococcus (n = 20), Staphylococcus spp. (n = 1), M. tuberculosis (n = 2), N. gonorrhea (n = 8), Chlamydia tr. (n = 16) and, Ureaplasma urealyticum (n = 1). The infection group had significantly (p < 0.05) lower: semen volume, alpha-glucosidase, fructose, and zinc in seminal plasma and, higher pH than the control group. None of these parameters was sufficiently accurate in the ROC analysis to discriminate between infected and non- infected men. Conclusion: Proven bacterial infections of the MRT impact negatively on all the accessory gland function parameters evaluated in semen, suggesting impairment of the secretory capacity of the epididymis, seminal vesicles and prostate. -
CUA Guideline: the Workup and Management of Azoospermic Males
Originalcua guideline research CUA Guideline: The workup and management of azoospermic males Keith Jarvi, MD, FRCSC;* Kirk Lo, MD, FRCSC;* Ethan Grober, MD;* Victor Mak, MD, FRCSC;* Anthony Fischer, MD, FRCSC;¥ John Grantmyre, MD, FRCSC;± Armand Zini, MD, FRCSC;+ Peter Chan, MD, FRCSC;+ Genevieve Patry, MD, FRCSC;£ Victor Chow, MD, FRCSC;§ Trustin Domes, MD, FRCSC# *Department of Urology, Mount Sinai Hospital, University of Toronto, Toronto, ON; ¥Division of Urology, McMaster University, Hamilton, ON; ±Department of Urology, Dalhousie University, Halifax, NS; +Division of Urology, McGill University Health Centre, Montreal, QC; £Hôtel-Dieu De Lévis, Lévis, QC; §Department of Urologic Sciences, University of British Columbia, Vancouver, BC; #Saskatoon Health Region, Saskatoon, SK Cite as: Can Urol Assoc J 2015;9(7-8):229-35. http://dx.doi.org/10.5489/cuaj.3209 A further group of men have a failure to ejaculate. These Published online August 10, 2015. may be men with spinal cord injury, psychogenic failure to ejaculate, or neurological damage (sympathetic nerve committee was established at the request of the damage from, for example, a retroperitoneal lymph node Canadian Urological Association to develop guide- dissection). A lines for the investigation and management of azo- To understand the management of azoospermia, it is ospermia. Members of the committee, all of whom have important to also understand the role of assisted reproduc- special expertise in the investigation and management of tive technologies (ARTs) (i.e., in-vitro fertilization) in the male infertility, were chosen from different communities treatment of azoospermia. Since the 1970s, breakthroughs across Canada. The members represent different practices in the ARTs have allowed us to offer potentially successful in different communities. -

Microrna-125B Controls Growth of Ovarian Granulosa Cells in Polycystic Ovarian Syndrome by Modulating Cyclin B1 Expression
Basic research MicroRNA-125b controls growth of ovarian granulosa cells in polycystic ovarian syndrome by modulating cyclin B1 expression Jie Deng, Chanyu Li, Jianbo Luo, Jiaqiong Xie, Cong Peng, Xiaoyang Deng Department of Gynecology, the First Affiliated Hospital of Chengdu Medical College, Corresponding author: Chengdu, Sichuan, China Xiaoyang Deng Department Submitted: 7 January 2019 of Gynecology Accepted: 27 April 2019 The First Affiliated Hospital of Chengdu Arch Med Sci Medical College DOI: https://doi.org/10.5114/aoms.2019.85809 Chengdu, Sichuan Copyright © 2019 Termedia & Banach China 610500 Phone/fax: +86 028-83016137 Abstract E-mail: pingli2865@yahoo. com Introduction: There is a lot of evidence that suggests that microRNAs (miRs) play an imperative role in the pathogenesis of polycystic ovary syndrome (PCOS). This study was designed to decipher the role of miR-125b in PCOS pathogenesis. Material and methods: Expression analysis of miR-125b was determined by real-time quantitative polymerase chain reaction and the KGN ovarian granulosa cell viability was examined by CCK-8 assay. DAPI assay and flow cytometry were carried out for the detection of apoptosis and cell cycle dis- tribution respectively. Protein levels were checked by immunoblotting. Results: The miR-125b transcript levels were considerably high in polycystic ovaries and ovarian granulosa KGN cells. The inhibition of miR-125b expres- sion decreased the viability of the KGN cells by arresting the cells at the G2/M check point. Target Scan analysis revealed cyclin B1 as the target of miR-125b and suppression of miR-125b caused considerable up-regulation of cyclin B1 expression. Like miR-125b inhibition, cyclin B1 silencing also inhibited the KGN cell viability via G2/M arrest. -
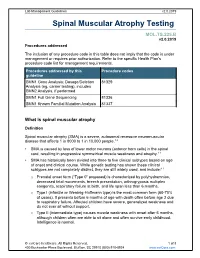
Spinal Muscular Atrophy Testing
Lab Management Guidelines v2.0.2019 Spinal Muscular Atrophy Testing MOL.TS.225.B v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline SMN1 Gene Analysis; Dosage/Deletion 81329 Analysis (eg, carrier testing), includes SMN2 Analysis, if performed SMN1 Full Gene Sequencing 81336 SMN1 Known Familial Mutation Analysis 81337 What is spinal muscular atrophy Definition Spinal muscular atrophy (SMA) is a severe, autosomal recessive neuromuscular disease that affects 1 in 8000 to 1 in 10,000 people.1,2 SMA is caused by loss of lower motor neurons (anterior horn cells) in the spinal cord, resulting in progressive symmetrical muscle weakness and atrophy.1-3 SMA has historically been divided into three to five clinical subtypes based on age of onset and clinical course. While genetic testing has shown these clinical subtypes are not completely distinct, they are still widely used, and include:1-3 o Prenatal onset form (“Type 0” proposed) is characterized by polyhydramnios, decreased fetal movements, breech presentation, arthrogryposis multiplex congenita, respiratory failure at birth, and life span less than 6 months. o Type I (infantile or Werdnig-Hoffmann type) is the most common form (60-70% of cases). It presents before 6 months of age with death often before age 2 due to respiratory failure. Affected children have severe, generalized weakness and do not ever sit without support. -

The Relationship Between H19 and Parameters of Ovarian Reserve Xi Xia1,2, Martina S
Xia et al. Reproductive Biology and Endocrinology (2020) 18:46 https://doi.org/10.1186/s12958-020-00578-z RESEARCH Open Access The relationship between H19 and parameters of ovarian reserve Xi Xia1,2, Martina S. Burn2, Yong Chen3,2, Cengiz Karakaya4 and Amanda Kallen2* Abstract Context: The H19 long noncoding RNA (lncRNA) belongs to a highly conserved, imprinted gene cluster involved in embryonic development and growth control. We previously described a novel mechanism whereby the Anti- mullerian hormone (Amh) appears to be regulated by H19. However, the relationship between circulating H19 and markers of ovarian reserve including AMH not been investigated. Objective: To determine whether H19 expression is altered in women with decreased ovarian reserve. Design: Experimental study. Setting: Yale School of Medicine (New Haven, USA) and Gazi University School of Medicine (Ankara, Turkey). Patients or other participants: A total of 141 women undergoing infertility evaluation and treatment. Intervention: Collection of discarded blood samples and cumulus cells at the time of baseline infertility evaluation and transvaginal oocyte retrieval, respectively. Main outcome measure: Serum and cumulus cell H19 expression. Results: Women with diminished ovarian reserve (as determined by AMH) had significantly lower serum H19 expression levels as compared to controls (p < 0.01). Serum H19 was moderately positively correlated with serum AMH. H19 expression was increased 3.7-fold in cumulus cells of IVF patients who demonstrated a high response to gonadotropins, compared to low responders (p < 0.05). Conclusion: In this study, we show that downregulation of H19 in serum and cumulus cells is closely associated with decreased ovarian reserve, as measured by decreased AMH levels and reduced oocyte yield at oocyte retrieval. -

This Document Was Released in November 2020. This Document Will Continue to Be Periodically Updated to Reflect the Growing Body of Literature Related to This Topic
MEDICAL STUDENT CURRICULUM This document was released in November 2020. This document will continue to be periodically updated to reflect the growing body of literature related to this topic. Help: Andrew Gusev - [email protected] MALE INFERTILITY KEYWORDS: infertility, azoospermia, oligospermia, semen analysis, varicocele LEARNING OBJECTIVES: At the end of medical school, the medical student will be able to… 1. Describe the hypothalamus-pituitary-gonadal (HPG) axis 2. Describe the workup for male infertility, including the importance of the physical exam 3. Restate the limitations of the semen analysis 4. List some common reversible causes of infertility and their treatments 5. Recognize when to refer a patient for ART Introduction Approximately 15% of couples will be unable to conceive after attempting unprotected intercourse for one year. Of these couples, about 50% of them will have some male factor to that is contributing to their infertility (a male factor is the sole reason in approximately 20% of infertile couples). (Thonneau P, 1991) Male infertility can be due to a variety of genetic, anatomic, and environmental conditions, many of which will be briefly discussed below. When a cause for an abnormal semen analysis cannot be found, it is termed idiopathic. When a man is infertile with a normal semen analysis and workup, the term unexplained infertility is used. As the word suggests, these men do not have a known cause for their infertility but it is thought to likely be due genetic defects that have not been described yet. The purpose of evaluation is to identify possible conditions causing infertility and treating reversible conditions which may improve a man’s fertility potential. -

The ART of Assisted Reproductive Technology
Infertility • THEME The ART of assisted reproductive technology BACKGROUND One in six Australian couples of The Australian Institute of Health and Welfare's reproductive age experience difficulties in National Perinatal Statistical Unit's annual report Jeffrey Persson, conceiving a child. Once a couple has been Assisted reproductive technology in Australia and New MD, FRANZCOG, CREI, is Clinical appropriately assessed, assisted reproductive Zealand 2002, shows that babies born in 2002 using Director (City), technology (ART) techniques can be used to assisted reproductive technology (ART) had longer IVFAustralia. overcome problems with ovulation, tubal patency, gestational ages, higher birth weights and fewer peri- [email protected] male fertility or unexplained infertility. natal deaths than their counterparts of 2 years OBJECTIVE This article discusses the range of previously.1 ART techniques available to subfertile couples. This is the first year national data have been avail- able on the age of women (and their partners) using DISCUSSION Intracytoplasmic sperm injection is now the most common form of ART used in ART. The average age of women undergoing treat- Australia, being used in almost half of all fresh ment in 2002 was 35.2 years, and the average cycles, with in vitro fertilisation being used in age of partners was 37.6 years.1 Age remains the approximately one-third of all fresh cycles. most significant issue affecting a couple's chance of conceiving and carrying a pregnancy to full term. Women need to understand the impact age has on their chance of becoming pregnant. Once a couple has been assessed and investigations suggest subfer- tility, the treatment options depend on the underlying cause (Table 1). -

Obesity and Reproduction: a Committee Opinion
Obesity and reproduction: a committee opinion Practice Committee of the American Society for Reproductive Medicine American Society for Reproductive Medicine, Birmingham, Alabama The purpose of this ASRM Practice Committee report is to provide clinicians with principles and strategies for the evaluation and treatment of couples with infertility associated with obesity. This revised document replaces the Practice Committee document titled, ‘‘Obesity and reproduction: an educational bulletin,’’ last published in 2008 (Fertil Steril 2008;90:S21–9). (Fertil SterilÒ 2015;104:1116–26. Ó2015 Use your smartphone by American Society for Reproductive Medicine.) to scan this QR code Earn online CME credit related to this document at www.asrm.org/elearn and connect to the discussion forum for Discuss: You can discuss this article with its authors and with other ASRM members at http:// this article now.* fertstertforum.com/asrmpraccom-obesity-reproduction/ * Download a free QR code scanner by searching for “QR scanner” in your smartphone’s app store or app marketplace. he prevalence of obesity as a exceed $200 billion (7). This populations have a genetically higher worldwide epidemic has underestimates the economic burden percent body fat than Caucasians, T increased dramatically over the of obesity, since maternal morbidity resulting in greater risks of developing past two decades. In the United States and adverse perinatal outcomes add diabetes and CVD at a lower BMI of alone, almost two thirds of women additional costs. The problem of obesity 23–25 kg/m2 (12). and three fourths of men are overweight is also exacerbated by only one third of Known associations with metabolic or obese, as are nearly 50% of women of obese patients receiving advice from disease and death from CVD include reproductive age and 17% of their health-care providers regarding weight BMI (J-shaped association), increased children ages 2–19 years (1–3). -

Risk of First Trimester Spontaneous Miscarriage Among Singleton
Middle East Fertility Society Journal (2013) xxx, xxx–xxx Middle East Fertility Society Middle East Fertility Society Journal www.mefsjournal.org www.sciencedirect.com ORIGINAL ARTICLE Risk of first trimester spontaneous miscarriage among singleton gestations following ICSI and its relation to underlying cause of infertility Wessam Magdi Abuelghar a,*, Osama Saleh Elkady a, Tarek Fathi. Tamara a, Mona Hassan Khalil b a Obstetrics and Gynaecology Department, Ain-shams University, Cairo, Egypt b Obstetrics and Gynaecology Department, El Khazendara MOH Hospital, Cairo, Egypt Received 16 April 2013; accepted 12 June 2013 KEYWORDS Abstract Study objective: To assess the association between the first trimester miscarriage rates Miscarriage; among women undergoing intracytoplasmic sperm injection (ICSI) and underlying etiology of ICSI; infertility. Infertility Design: Prospective cohort study. Setting: Ain Shams University maternity hospital. Materials and methods: The study included women who became pregnant with singleton preg- nancy following ICSI as a treatment for different causes of infertility. Women were followed up throughout the first trimester of pregnancy up to 12 weeks’ gestation (10 weeks after the day of embryo transfer). Main outcome measure: First trimester miscarriage rate. Results: Two hundred and thirty four pregnant young women were included in the study, 164 (70.9%) women miscarried. The causes of infertility among these women were as follows: 41 (25%) mild male factor infertility, 40 (24.4%) severe male factor infertility, 45 (27.44%) tubal fac- tor, 7 (4.27%) polycystic ovarian syndrome, 3 (1.83%) endometriosis, 20 (12.19%) unexplained and Abbreviations: BMI, body mass index; CI, confidence interval; E2, estradiol; ET, embryo transfer; FSH, follicle stimulating hormone; GnRH, gonadotropin-releasing hormone; hCG, human chorionic gonadotropin; ICSI, intracytoplasmic sperm injection; IVF, in vitro fertilization; LH, luteinizing hormone; LMP, last menstrual period; OR, odds ratio; SD, standard deviation * Corresponding author. -

Chronic Pelvic Pain Syndrome in Men
Chronic Pelvic Pain Syndrome in Men Diagram of the male genital tract showing the pelvic floor anatomy and how it is linked to the urinary tract with the urethra passing through it (external urethral sphincter). The pelvic floor therefore helps control how we pass water (urinate). (See resources at end for links to images of pelvic floor muscles and prostate.) SUMMARY Chronic pelvic pain syndrome (CPPS) and chronic prostatitis (CP) in men are often terms used to describe a condition which causes pain in the lower pelvic region of men. Symptoms are thought to come from the prostate gland or increased muscle tension around the pelvic floor. Our experience at Unity indicates that ¾ (75%) of men will have a significant improvement in their symptoms, with best results achieved by: 1) Ruling out underlying infection and excluding cancer in those who are worried about these being the cause 2) Having a detailed discussion so that you understand the complex mechanisms which can cause pelvic pain 3) Some treatments including alpha blockers, antibiotics, and sometimes painkillers 4) Pelvic floor muscle relaxation techniques 5) Psychological support/therapy in order to reduce pelvic floor muscle tension and improve strategies for coping with the pain, help you address your underlying worries and concerns and identify and reduce possible sources of stress. Vs3 31/03/2020 1 What is Chronic Pelvic Pain Syndrome? Chronic pelvic pain syndrome (CPPS) can occur in both men and women. It is sometimes also called chronic prostatitis (CP) in men. This leaflet deals with CPPS in men. CPPS/CP is an ongoing (persistent or recurrent > 3 of the last 6 months) discomfort or pain that you feel in your lower pelvic region - mainly at the base or tip of your penis, and/or your testicles and/or around your back passage (anus) for which no cause has been found.