District Health Society Vaishali
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A List of Terminated Vendors As on April 30, 2021. SR No ID Partner
A List of Terminated Vendors as on April 30, 2021. SR No ID Partner Name Address City Reason for Termination 1 124475 Excel Associates 123 Infocity Mall 1 Infocity Gandhinagar Sarkhej Highway , Gandhinagar Ahmedabad Breach Of Contract 2 125073 Karnavati Associates 303, Jeet Complex, Nr.Girish Cold Drink, Off.C.G.Road, Navrangpura Ahmedabad Breach Of Contract 3 132097 Sam Agency 29, 1St Floor, K B Commercial Center, Lal Darwaja, Ahmedabad, Gujarat, 380001 Ahmedabad Breach Of Contract 4 124284 Raza Enterprises Shopno 2 Hira Mohan Sankul Near Bus Stand Pimpalgaon Basvant Taluka Niphad District Nashik Ahmednagar Fraud Termination 5 124306 Shri Navdurga Services Millennium Tower Bldg No. A/5 Th Flra-201 Atharva Bldg Near S.T Stand Brahmin Ali, Alibag Dist Raigad 402201. Alibag Breach Of Contract 6 131095 Sharma Associates 655,Kot Atma Singh,B/S P.O. Hide Market, Amritsar Amritsar Breach Of Contract 7 124227 Aarambh Enterprises Shop.No 24, Jethliya Towars,Gulmandi, Aurangabad Aurangabad Fraud Termination 8 124231 Majestic Enterprises Shop .No.3, Khaled Tower,Kat Kat Gate, Aurangabad Aurangabad Fraud Termination 9 125094 Chudamani Multiservices Plot No.16, """"Vijayottam Niwas"" Aurangabad Breach Of Contract 10 NA Aditya Solutions No.2239/B,9Th Main, E Block, Rajajinagar, Bangalore, Karnataka -560010 Bangalore Fraud Termination 11 125608 Sgv Associates #90/3 Mask Road,Opp.Uco Bank,Frazer Town,Bangalore Bangalore Fraud Termination 12 130755 C.S Enterprises #31, 5Th A Cross, 3Rd Block, Nandini Layout, Bangalore Bangalore Breach Of Contract 13 NA Sanforce 3/3, 66Th Cross,5Th Block, Rajajinagar,Bangalore Bangalore Breach Of Contract 14 132890 Manasa Enterprises No-237, 2Nd Floor, 5Th Main First Stage, Khb Colony, Basaveshwara Nagar, Bangalore-560079 Bangalore Breach Of Contract 15 177367 Bharat Associates 243 Shivbihar Colony Near Arjun Ki Dairy Bankhana Bareilly Bareilly Breach Of Contract 16 132878 Nuton Smarte Service 102, Yogiraj Apt, 45/B,Nutan Bharat Society,Opp. -

Danapur Sonpur Samastipur Mugalsarai Dhanbad
S.N Division Name of station Division Name of Division Name of Division Name of Division Name of station station station station 1 DANAPUR DHANBAD MUGALSARAI SONPUR SAMASTIPUR 2 Patna Jn. Dhanbad Gaya Sonpur Samastipur 3 Ara Gomoh Mugalsarai Muzaffarpur Darbhanga 4 Buxar Daltonganj Sasaram Hajipur Narkatiaganj Patna Saheb Chandrapura Dehri-on-sone Barauni Saharsa 5 Danapur Koderma Bhabhua Road Khagaria Motihari 6 Rajgir Hazaribag Road Anugrah Begusarai Betiah 7 Narayan Road 8 Mokama Barkakana Rafiganj Dholi Chakia 9 Kiul Renukut Japala Bhagwanpur Bagaha 10 Jhajha Parasnath Ismailpur Naugachhia Sugauli 11 Jamui Garhwa Road Manpur Mansi Harinagar 12 Lakhisarai Singrauli Guraru Thanabihpur Raxaul 13 Hathidah Tori Saiyad Raja Dalsinghsarai Sakari Barh Chandauli 14 Ranchi Road Majhwar Shahpur Patori Jaynagar 15 Bakhtiyarpur Phusro Paraiya Desari Banmankhi 16 Fatuha Katrasgarh Kudra Dighwara Madhubani Jehanabad Akshwaywat Rai Simri 17 Chopan Pehsar Nagar Bhakhtiyarpur Dumraon Sindri Town Mohiudddin Hasanpur 18 Karwandiya Nagar Road Dildarnagar Pradhankhunta 19 Durgawati Semapur Rusera Ghat 20 Zamania Paharpur Pusauli Kursela Rajnagar Sekhpura Tetulmari 21 Karmnasa Karhagola Road Raghopur Nawada Choubey Khudiram B. Dauram 22 Sonnagar Pusa Madhepura 23 Biharsharif Parsabad Jakhim Karpoorigram Sitamarhi Rajendra Nagar T. Nayagaon 24 Gomia Ganj Khwaja Laheriasarai Gulzarbag Narayanpur 25 Bokaro Thermal Muthani Anant Supaul 26 Bihta Garhwa Town Kumahu Sarai Jhanjharpur Bihiya Shiv Sagar Baragopal 27 Barwadih Road Ghorasahan 28 Taregna Patratu Nimiaghat -
Note :- in Case of Any Clarification /Objection of Below Mentioned List
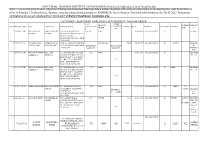
INDUSTRIAL TRAINING INSTITUTE, MUZAFFARPUR (Provisional Application List of Guest Faculty) Note :- In case of any clarification /objection of below mentioned List Please provide a written objection with necessary doccument in any working day upto 02-03-2017 at office of Principal, I.T.I Muzaffarpur, Gannipur, Near kalambag chowk, (contact no. 9504694156). No clarification/ Objection will considered after 02-03-2017. Doccument verification and viva will scheduled from 06-03-2017 of District Muzaffarpur Candidates only. CATEGORY - B (RETIRED EMPLOYEE LIST) DISTRICT - MUZAFFARPUR TECH. OTHER BRANCH/ EXPERIE REMARK Sl No. Diary No. / Date Name Father's Name Parmanant Adress QUALIFICATIO QUALIFICAT MARKS % D.OB DISTRICT CATEGORY BRANCH TRADE NCE S N ION 1 425/06-09-2016 ANIL KUMAR HARI SHANKAR VILL+PO - BISHNUPUR B TECH MMV 01-05-1969 MUZAFFARPUR B ex. Army MISHRA MISHRA BAGHANAGARI VIA- DHOLI PS- SAKRA DIST- MUZAFFARPUR 843105 MOB -9931161254 2 1709-16-09-16 SAYED KAISER SAYED AHMAD MOH -KAMRA CHANDWARA ELCTRICAL 54.33 15/08/1947 MUZAFFARPUR B MATH RETIERE IMAM KAJMI HASAN KAJMI MUZAFFARPUR 842001 MOB DIPLOMA IN DIPLOMA IN D - 9835827204 ELEC.ENG. ELEC.ENG. INSTRUC TOR 3 436/07-09-2016 REHAN AHMAD MD. ANAS AT- SIRSAIDYAD COLONEY CTI DMM 01-03-1954 MUZAFFARPUR B RETIRED SIDDIQUE SIDDIQUE NEAR DAV PUBLIC SCHOOL ITI A.S. BEHIND BMP -6 MALIGHAT PO - H.P.O. PS - AHIYAPUR ITI DIST - MUZAFFARPUR 842001 MOB- 9470601665 4 437/07-09-2016 REHAN AHMAD MD. ANAS AT- SIRSAIDYAD COLONEY CTI DMM 01-03-1954 MUZAFFARPUR B DMM RETIRED SIDDIQUE SIDDIQUE NEAR DAV PUBLIC SCHOOL ITI A.S. -

Village Midline Study Vaishali, Bihar State, India
Village Midline Study Vaishali, Bihar State, India Authors: Pratyaya Jagannath Kanchan Kargwal Namrata Sharma Sanjay Prasad Mansi Nagpal Arun Khatri-Chhetri Village Midline Study: Vaishali, Bihar State, India CGIAR Research Program on Climate Change, Agriculture and Food Security (CCAFS) Pratyaya Jagannath, Kanchan Kargwal, Namrata Sharma, Sanjay Prasad, Mansi Nagpal and Arun Khatri-Chhetri 1 Correct citation: Jagannath P, Kargwal K, Sharma N, Prasad S, Nagpal M, Khatri-Chhetri A. 2020. Village Midline Study: Vaishali, Bihar State, India. CCAFS Report. Wageningen, the Netherlands: CGIAR Research Program on Climate Change, Agriculture and Food Security (CCAFS). Available online at: www.ccafs.cgiar.org Published by the CGIAR Research Program on Climate Change, Agriculture and Food Security (CCAFS). The CGIAR Research Program on Climate Change, Agriculture and Food Security (CCAFS) is a strategic partnership of CGIAR and Future Earth, led by the International Center for Tropical Agriculture (CIAT). The Program is carried out with funding by CGIAR Fund Donors, Australia (ACIAR), Ireland (Irish Aid), Netherlands (Ministry of Foreign Affairs), New Zealand Ministry of Foreign Affairs & Trade; Switzerland (SDC); Thailand; The UK Government (UK Aid); USA (USAID); The European Union (EU); and with technical support from The International Fund for Agricultural Development (IFAD). Contact: CCAFS Program Management Unit, Wageningen University & Research, Lumen building, Droevendaalsesteeg 3a, 6708 PB Wageningen, The Netherlands. Email: [email protected] Creative Commons License This Report is licensed under a Creative Commons Attribution – NonCommercial 4.0 International License. Articles appearing in this publication may be freely quoted and reproduced provided the source is acknowledged. No use of this publication may be made for resale or other commercial purposes. -

Rehablitation of Mahatma Gandhi Setu in Patna
Rehablitation of Mahatma Gandhi Setu in Patna Contractor Name:- FPCC Ind. Ltd 1. Introduction The Mahatma Gandhi Bridge was constructed about 25 years ago over the Ganges River in order to connect patna to the other side of river. Once completed it was supposed to be the part of N.H 19 and comes directly under Central Government of India. It is one of the longest bridge in india. The bridge has 46 spans each with length 120m. Each span has two cantilever beams on both sides which are free to move at the ends. It has two lanes one upstream and the other downstream each with a width of around 6m. Both the lanes are also free from each other and are not connected anywhere. It was constructed by using 3 meter pre-casted parts being joined at both ends to complete the span. The Spans are connected by using a Protrusion which is free to move longitudinally also along the river flow. In upwards and downwards direction it is such that it allows vibration to transfer smoothly to the next span while vehicular movement without much discreteness. It is shown in fig. Due to heavy traffic movement and being the only bridge to cross ganges river the bridge is used heavily now. Hence it has started vibrating with a higher amplitude than it was designed to. Also in many spans the cantilever beams were found to have sagged at ends. 2. Rehabilitation Keeping the structural health prospective in mind it was decided for immediate rehabilitation of the bridge to provide extra strength to the spans so that it bear the existing vehicular load according to the IRC. -

Zila Parishad JITESH KUMAR ARARIA
Panchayati Raj Department Government of Bihar List of Panchayat IT Operators Deployed in the Districts for PRIASoft SL District Block Name Father's Name Mobile 1 Zila Parishad JITESH KUMAR 2 Araria RAJ KUMAR RAJ KRIPA NAND JHA 9835838537 3 Bhargama MD. SARWAR ALAM MD. SIRAJUDDIN 9709996217 4 Forbesganj SANJAY KUMAR SAH MAHENDRA SAH 9199120088 5 Jokihat MD. ASHALAM JAFAR HAZI ASFAQUE HUSAIN 9308734215 ARARIA 6 Kursakatta SANTOSH KUMAR SAH MAKSHUDAN SAH 7 Narpatganj MANOJ KR. BHARATI BHAGWAN MANDAL 9709573281 8 Palasi 9 Raniganj ANUBHAV KUMAR JAI PRAKASH NAYAK 9570357990 10 Sikti PREM KUMAR PASWAN YOGENDRA PASWAN 7250394187 D:\Sarvesh-2012\IT Operators Deployed in District HQ Block\IT Operators deployed in the districts_HQ_Block 1 | 38 it operator_Blocks_n_HQ_280 (2) Panchayati Raj Department Government of Bihar List of Panchayat IT Operators Deployed in the Districts for PRIASoft SL District Block Name Father's Name Mobile 1 Zila Parishad SANTOSH KUMAR 9771734044 2 Arwal ARVIND KUMAR BHIM SINGH 9334480335 3 Kaler AMITSH SHRIVASTAV VIJAY KUMAR SHRIVASTAV ARWAL 4 Karapi RAVIRANJAN KR. PARASAR HARIDWAR SHARMA 8334800422 5 Kurtha KUNDAN KUMAR BINESHWAR PANDIT 9279386443 6 Sonabhadra Vanshi Suryapur MANOJ KUMAR LEELA SINGH D:\Sarvesh-2012\IT Operators Deployed in District HQ Block\IT Operators deployed in the districts_HQ_Block 2 | 38 it operator_Blocks_n_HQ_280 (2) Panchayati Raj Department Government of Bihar List of Panchayat IT Operators Deployed in the Districts for PRIASoft SL District Block Name Father's Name Mobile 1 Zila Parishad RAKESH -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -
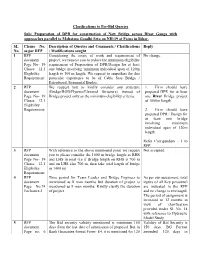
Clarifications to Pre-Bid Queries Sub: Preparation of DPR for Construction
Clarifications to Pre-Bid Queries Sub: Preparation of DPR for construction of New Bridge across River Ganga with approaches parallel to Mahatma Gandhi Setu on NH-19 at Patna in Bihar. SL Clause No. Description of Queries and Comments / Clarifications Reply No. as per RFP / Modifications sought 1 RFP Considering the scope of work and requirement of No change. document project, we request you to reduce the minimum eligibility Page No- 19 requirement of Preparation of DPR/Design for at least Clause 12.1 one bridge involving minimum individual span of 120m Eligibility length to 100 m length. We request to empathise for this Requirement; particular experience to be of Cable Stay Bridge / Extradosed /Segmental Bridge. 2 RFP We request you to kindly consider any structure 1. Firm should have document (Bridge/ROB/Flyover/Elevated Structure) instead of prepared DPR for at least Page No- 19 Bridge project only as the minimum eligibility criteria. one River Bridge project Clause 12.1 of 1000m length. Eligibility Requirement; 2. Firm should have prepared DPR / Design for at least one bridge involving minimum individual span of 120m length. Refer Corrigendum - I to RFP. 3 RFP With reference to the above mentioned point we request Not accepted. document you to please consider the 1000 m bridge length as RHS Page No- 19 and LHS in total (i.e if Bridge length on RHS is 700 m Clause 12.1 and on LHS also 700 m, then take total length of bridge Eligibility as 1400 m) Requirement; 4 RFP Time period for Team Leader and Bridge Engineer is As per our assessment, total document mentioned as 8 man months but duration of project is inputs of all Key personnel Page No.74 mentioned as 9 man months. -

Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-Gradation Cum Consolidation Priority List
Pradhan Mantri Gram Sadak Yojana CUCPL - Comprehensive Up-gradation cum Consolidation Priority List State : Bihar District : All Districts Block : All Blocks Sr.No. State District Block Plan CN Plan Road Name Plan Road Route Educati Medical Veterin Transp Market Administ Populatio Total Score Per Avg PCI Road No. Length Priority onal Faciliti ary ort and Faciliti rative n Score Unit Services es Facilitie Commu es Centres Length s nicatio n Infrastr ucture 1 Bihar Arwal Arwal MRL01 Walidad, T01 To Khamhaini 10.835 M 12 0 0.00 0.00 0.00 1 68 81.00 7.48 1.00 2 Bihar Arwal Banshi MRL02 Manjhiyama to Khatangi 9.465 M 16 8 0.00 9.00 0.00 1 77 111.00 11.73 1.00 Surajpur 3 Bihar Arwal Banshi MRL03 Kharasi to Belaura 14.943 M 22 8 0.00 3.00 0.00 1 89 123.00 8.23 1.00 Surajpur 4 Bihar Arwal Banshi MRL01 Khatangi senari RD to Mobarakpur 10.860 M 9 4 0.00 3.00 0.00 1 42 59.00 5.43 1.00 Surajpur 5 Bihar Arwal Kaler MRL01 Sohasa Road L037 To Masadpur 21.676 M 10 6 0.00 6.00 0.00 1 54 77.00 3.55 1.00 6 Bihar Arwal Karpi MRL02 Imamganj Deokund Road,T04 To Jonha 7.365 M 22 8 3.00 11.00 9.00 2 91 146.00 19.82 1.00 7 Bihar Arwal Karpi MRL01 Karpi Barahmile Road, T03 To Salarpur 12.365 M 18 6 0.00 9.00 7.00 2 104 146.00 11.81 1.00 8 Bihar Arwal Karpi MRL03 Arwal Jehanabad Road, T02 To Aiyara 16.787 M 7 0 0.00 0.00 7.00 1 52 67.00 3.99 1.00 9 Bihar Arwal Kurtha MRL02 Salarpur L042, To Dhamaul 15.238 M 9 4 0.00 3.00 7.00 2 88 113.00 7.42 1.00 10 Bihar Arwal Kurtha MRL01 Pinjrawan to Manepaker 9.456 M 8 2 0.00 0.00 0.00 1 55 66.00 6.98 1.00 11 Bihar Aurangabad -

DISTRICT : Muzaffarpur
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Muzaffarpur 1 KIRAN KUMARIARVIND KUMAR kiran kumari c/o arvind 10-Dec-66 GEN 700 603 86.14 Muzaffarpur (1) Samastipur (1) Darbhanga (1) Vaishali (1) Champaran-E (1) kumar vill+po-parsara dis-muzaffarpur 2 ARCHANA SRI ARUN vill-ratanpur post- 11-Aug-85 ST 900 757 84.11 Muzaffarpur (2) KUMARI CHAUDHARY jagdishparn vhaya- kalyanapur dist- muzaffarpur pin-848302 3PREM LATA SHARI NAND LAL village raja bigha, p.s. 10-Jan-79 GEN 700 566 80.86 Saran (2) Muzaffarpur (3) Darbhanga (2) Gaya (4) Champaran-E (2) KUMARI PRASAD dhanarua. p.o barni district patna pin code 804452 4 REENA SINHASRI DINESH SINGH dinesh singh, d/o- sita 31-Dec-76 BC 900 721 80.11 Siwan (2) Begusarai (3) Muzaffarpur (4) Samastipur (4) Vaishali (5) sharan singh, vill- ruiya, post- ruiya bangra, p.s.- jiradei, distt- siwan 5NILAM SHRI GUJESHWER nilam srivastav c/o-shri 06-Jan-69 BC 700 554 79.14 Gopalganj (2) Siwan (3) Saran (3) Muzaffarpur (5) Patna (14) SRIVASTAV PRASAD akhilesh prasad vill-manichapar, po-hathua dis-gopalginj pin-841436 6 BEENA KUMARIMAHARANGHI vill-mahrana 01-Oct-75 BC 900 700 77.78 Munger (17) Lakhisarai (11) Bhagalpur (15) Muzaffarpur (6) Jamui (12) MATHO po-dahara dis-munger pin-811201 7 KANAK LATASRI ANIL KUMAR village+post- dahibhatta, 23-Dec-85 GEN 700 541 77.29 Gopalganj (5) -

The India Toy Fair Virtual-2021 27 Feb- 2 Mar-2021
THE INDIA TOY FAIR VIRTUAL-2021 27 FEB- 2 MAR-2021 1 THE INDIA TOY FAIR VIRTUAL-2021 27 FEB- 2 MAR-2021 PARTICIPANTS PROFILE 2Teeth Kidswear Address : 168, Arulandhanammalnagar, Pudukottai main Road, Thanjavur, Thanjavur - 613007 (TAMIL NADU) Contact Number : 8610225174, Email : [email protected] , Contact Person : Suganthan Product Category : Baby & Toddler Toys 3LININVOVATIONS Address : 448, BHARATHIYAR RD, PAPA NAICKENPALAYAM, COIMBATORE - 641037 (TAMIL NADU) Contact Number : 9791330359, Email : [email protected] , Contact Person : BALAJI Product Category : Action & Toy Figures 7 Star Toys Industrial Corportaion, Address : G1-1287, RIICO Industrial Area, Phase-V, Bhiwadi, Distt- Alwar, BHIWADI - 301019 (RAJASTHAN) Contact Number : 9873433143, Email : [email protected] , Contact Person : Mr MukulMehndiratta- Partner Product Category : Action & Toy Figures A K Enterprise Address : K 704 Maple Tree, B/s. Manichandra Bungalows, Nr. Surdhara Circle, Sal Hospital Road, Memnagar, Ahmedabad - (Gujarat) Contact Number : 9898812211, Email : [email protected], [email protected] , Contact Person : Kalpesh Bhatia Product Category : Bikes, Skates & Ride-Ons A STAR MARKETING PVT LTD Address : GALI NO 4, JAWAHAR COMPOUND 186, JAKARIA BUNDER RD, SHIWDI WEST, MUMBAI - 400015 (MAHARASHTRA) Contact Number : 9820644540, Email : [email protected] , Contact Person : DIPESH SAVLA Product Category : Action & Toy Figures A. JERALD SHOBAN Address : 29, Near Arul Theatre, Pookara Matha Kobil,Street, Tanjore- DCH - 613501 (TAMIL NADU) Contact Number : 9360936022, Email : [email protected] , Contact Person : A.Jerald Shoban Product Category : Traditional Toys 2 THE INDIA TOY FAIR VIRTUAL-2021 27 FEB- 2 MAR-2021 A2Z PAMTY DECCE PVT. LTD. Address : 25, 36 GOVIND NAGAR ,SODAULA LANE,BORAWALI EAST, MUMBAI - 400092 (MAHARASHTRA) Contact Number : 8104804075, Email : [email protected] , Contact Person : JAYESH M. -

Geospatial Planning
ESMAP Global Mini Grid Technical Conference Abuja, Nigeria, December 6, 2017 FRONTIER DEVELOPMENTS IN MINI GRIDS Geospatial planning Ignacio J. Pérez-Arriaga CEEPR, MIT Instituto de Investigación Tecnológica (IIT), Comillas University Florence School of Regulation, European University Institute We have to change the “top-down” perspective… … by another one with demand & generation all over the place 4 What could be the true frontier of mini grids in the developing world? 5 I do believe that mini grids must… … become integrated as one more component of a comprehensive electrification process… … led by the incumbent distributor 6 • The differentiation between grid extension, mini grids & SHS is becoming blurred • An integrated perspective is becoming increasingly necessary 7 How can geospatial planning help in the electrification planning process? 8 What’s an electrification plan? (the techno-economic answer) • An electrification plan will consist of some mix of on- & off-grid expansions providing electricity access to all consumers at minimum cost – For some prescribed demand for each consumer – Meeting minimum reliability requirements – And additional constraints (e.g. limit on the total diesel utilization) 9 The costs of the plan • The plan will consist of on- & off-grid expansions • Grid extension costs – Investment & operation costs of new grid, reinforcements of existing grid, “upstream” cost of grid-supplied electricity, cost of non served energy • Off-grid development costs – Microgrids: Investment & operation costs of generation,