Revised March 2018 MRO Guidance Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Yerevan State Medical University After M. Heratsi
YEREVAN STATE MEDICAL UNIVERSITY AFTER M. HERATSI DEPARTMENT OF PHARMACY Balasanyan M.G. Zhamharyan A.G. Afrikyan Sh. G. Khachaturyan M.S. Manjikyan A.P. MEDICINAL CHEMISTRY HANDOUT for the 3-rd-year pharmacy students (part 2) YEREVAN 2017 Analgesic Agents Agents that decrease pain are referred to as analgesics or as analgesics. Pain relieving agents are also called antinociceptives. An analgesic may be defined as a drug bringing about insensibility to pain without loss of consciousness. Pain has been classified into the following types: physiological, inflammatory, and neuropathic. Clearly, these all require different approaches to pain management. The three major classes of drugs used to manage pain are opioids, nonsteroidal anti-inflammatory agents, and non opioids with the central analgetic activity. Narcotic analgetics The prototype of opioids is Morphine. Morphine is obtained from opium, which is the partly dried latex from incised unripe capsules of Papaver somniferum. The opium contains a complex mixture of over 20 alkaloids. Two basic types of structures are recognized among the opium alkaloids, the phenanthrene (morphine) type and the benzylisoquinoline (papaverine) type (see structures), of which morphine, codeine, noscapine (narcotine), and papaverine are therapeutically the most important. The principle alkaloid in the mixture, and the one responsible for analgesic activity, is morphine. Morphine is an extremely complex molecule. In view of establish the structure a complicated molecule was to degrade the: compound into simpler molecules that were already known and could be identified. For example, the degradation of morphine with strong base produced methylamine, which established that there was an N-CH3 fragment in the molecule. -

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -

Cannabis Pregnancy
Wellness Articles Attached are weekly health and wellness articles provided by Alberta Health Services. As a way to help all Albertans live a healthy life, we welcome and encourage weekly newspapers, community newsletters and other publications to reproduce this information free of charge. Credit to Alberta Health Services or the identified content provider would be appreciated. If you would like to be added to the distribution list for these articles, please email: [email protected]. You will receive a monthly email containing articles for the upcoming four weeks. An archive of past wellness articles is available at http://www.albertahealthservices.ca/9966.asp Proposed publication date: February 25, 2019 Content provided by: Alberta Health Services Cannabis and Pregnancy Now that cannabis is legal in Canada, pregnant and breastfeeding women or those that might become pregnant need information on how to make healthy decisions for themselves and their baby. Throughout pregnancy, a baby’s quickly developing brain is very sensitive to harmful environments. Things that can harm a baby’s brain include certain illnesses, and being exposed to chemicals like alcohol, tobacco, tobacco-like products, cannabis (marijuana, hashish, hash oil) and other drugs. Because of this, pregnant women should not use cannabis in any form (marijuana, hashish, hash oil) because the mother and the baby’s health can be affected. Using cannabis while breastfeeding is also not advised as it is passed into breastmilk and stored there, and could affect a baby’s developing brain. Tetrahydrocannabinol (THC) is the main active chemical in the cannabis plant that gives people who use it a ‘high’. -

Introduction to Aromaticity
Introduction to Aromaticity Historical Timeline:1 Spotlight on Benzene:2 th • Early 19 century chemists derive benzene formula (C6H6) and molecular mass (78). • Carbon to hydrogen ratio of 1:1 suggests high reactivity and instability. • However, benzene is fairly inert and fails to undergo reactions that characterize normal alkenes. - Benzene remains inert at room temperature. - Benzene is more resistant to catalytic hydrogenation than other alkenes. Possible (but wrong) benzene structures:3 Dewar benzene Prismane Fulvene 2,4- Hexadiyne - Rearranges to benzene at - Rearranges to - Undergoes catalytic - Undergoes catalytic room temperature. Faraday’s benzene. hydrogenation easily. hydrogenation easily - Lots of ring strain. - Lots of ring strain. - Lots of ring strain. 1 Timeline is computer-generated, compiled with information from pg. 594 of Bruice, Organic Chemistry, 4th Edition, Ch. 15.2, and from Chemistry 14C Thinkbook by Dr. Steven Hardinger, Version 4, p. 26 2 Chemistry 14C Thinkbook, p. 26 3 Images of Dewar benzene, prismane, fulvene, and 2,4-Hexadiyne taken from Chemistry 14C Thinkbook, p. 26. Kekulé’s solution: - “snake bites its own tail” (4) Problems with Kekulé’s solution: • If Kekulé’s structure were to have two chloride substituents replacing two hydrogen atoms, there should be a pair of 1,2-dichlorobenzene isomers: one isomer with single bonds separating the Cl atoms, and another with double bonds separating the Cl atoms. • These isomers were never isolated or detected. • Rapid equilibrium proposed, where isomers interconvert so quickly that they cannot be isolated or detected. • Regardless, Kekulé’s structure has C=C’s and normal alkene reactions are still expected. - But the unusual stability of benzene still unexplained. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -
Quantitative Drug Test Menu Section 2
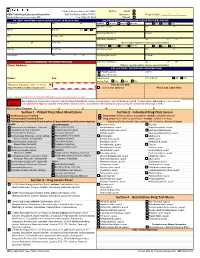
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Individual Patient & Medication Factors That Invalidate Morphine
Individual Patient & Medication Factors that Invalidate Morphine Milligram Equivalents Presented on June 7-8, 2021 at FDA Collaborative with various Federal Government Agency Stakeholders Jeffrey Fudin, PharmD, FCCP, FASHP, FFSMB Clinical Pharmacy Specialist & PGY2 Pain Residency Director Stratton VAMC, Albany NY Adjunct Associate Professor Albany College of Pharmacy & Health Sciences, Albany NY Western New England University College of Pharmacy, Springfield MA President, Remitigate Therapeutics, Delmar NY Disclosures Affiliation Role/Activities Abbott Laboratories Speaking, non-speakers bureau AcelRx Pharmaceuticals Acute perioperative pain (speakers bureau, consulting, advisory boards) BioDelivery Sciences International Collaborative publications, consulting, advisory boards Firstox Laboratories Micro serum testing for substances of abuse (consulting) GlaxoSmithKline (GSK) Collaborative non-paid poster presentations) Hisamitsu America Inc Advisory Board Hikma Pharmaceuticals Advisory Board Scilex Pharmaceuticals Collaborative non-paid publications Salix Pharmaceuticals Speakers bureau, consultant, advisory boards Torrent Pharmaceuticals Lecture, non-speakers bureau Learning Objectives At the completion of this activity, participants will be able to: 1. Explain opioid conversion and calculation strategies when developing a care plan for patients with chronic pain. 2. Assess patient-specific factors that warrant adjustment to an opioid regimen. 3. Identify important drug interactions that can affect opioid serum levels. 4. Describe how pharmacogenetic differences can affect opioid efficacy, toxicity, and tolerability. Not All Opioids are Created Equally Issues with MEDD & Opioid Conversion1-4 › Pharmacogenetic variability › Drug interactions › Lack of universal morphine equivalence › Specific opioids that should never have an MEDD – Methadone, Buprenorphine, Tapentadol, Tramadol 1. Fudin J, Marcoux MD, Fudin JA. Mathematical Model For Methadone Conversion Examined. Practical Pain Management. Sept. 2012. 46-51. 2. Donner B, et al. -

Substance Abuse in the Workplace Policy
Substance Abuse in the Workplace Policy Rexnord (herein referred to as “Rexnord” or the “Company”) has a strong commitment to its employees to provide a safe work environment and to promote high standards of employee performance. Consistent with the spirit and intent of this commitment, the Company has established a policy regarding substance abuse in the workplace. Further, the Company is committed to maintaining a drug-free workplace as required by “The Drug-Free Workplace Act of 1988.” Therefore, compliance with this Policy is a condition of continued employment with Rexnord. I. PURPOSE To outline the procedures to be followed by each location in order to ensure that the safety and performance of employees is not impaired by alcohol, illegal drugs or other substances. II. APPLICABILITY This policy shall apply to all employees (full-time, part-time, exempt, and non-exempt employees) as well as to all applicants who have received a conditional offer of employment. Personnel who perform their services on Company property or on a third party’s property at the request of the Company (e.g., a Company customer site), as provided under a contract either directly with the Company or through the services of an outside firm, are required to abide by this policy. It is the responsibility of the contracting firm (at its cost and expense) to ensure that its personnel are tested in conformance with this policy prior to working at / on behalf of Rexnord. III. SUBSTANCE ABUSE It is the Company’s policy that the following is prohibited and will result in discipline up to and including termination: A. -

Isomer Distributions of Molecular Weight 247 and 273 Nitro-Pahs in Ambient Samples, NIST Diesel SRM, and from Radical-Initiated Chamber Reactions
Atmospheric Environment 55 (2012) 431e439 Contents lists available at SciVerse ScienceDirect Atmospheric Environment journal homepage: www.elsevier.com/locate/atmosenv Isomer distributions of molecular weight 247 and 273 nitro-PAHs in ambient samples, NIST diesel SRM, and from radical-initiated chamber reactions Kathryn Zimmermann a,1, Roger Atkinson a,1,2,3, Janet Arey a,1,2,*, Yuki Kojima b,4, Koji Inazu b,5 a Air Pollution Research Center, University of California, Riverside, CA 92521, USA b Tokyo Institute of Technology, 4259 Nagatsuta, Midori-ku, Yokohama 226-8502, Japan article info abstract Article history: Molecular weight (mw) 247 nitrofluoranthenes and nitropyrenes and mw 273 nitrotriphenylenes (NTPs), Received 27 December 2011 nitrobenz[a]anthracenes, and nitrochrysenes were quantified in ambient particles collected in Riverside, Received in revised form CA, Tokyo, Japan, and Mexico City, Mexico. 2-Nitrofluoranthene (2-NFL) was the most abundant nitro- 28 February 2012 polycyclic aromatic hydrocarbon (nitro-PAH) in Riverside and Mexico City, and the mw 273 nitro-PAHs Accepted 5 March 2012 were observed in lower concentrations. However, in Tokyo concentrations of 1- þ 2-NTP were more similar to that of 2-NFL. NIST SRM 1975 diesel extract standard reference material was also analyzed to Keywords: examine nitro-PAH isomer distributions, and 12-nitrobenz[a]anthracene was identified for the first time. Nitro-PAH fl Atmospheric reactions The atmospheric formation pathways of nitro-PAHs were studied from chamber reactions of uo- Ambient particles ranthene, pyrene, triphenylene, benz[a]anthracene, and chrysene with OH and NO3 radicals at room Nitrotriphenylenes temperature and atmospheric pressure, with the PAH concentrations being controlled by their vapor pressures. -

Pharmacology and Toxicology of Amphetamine and Related Designer Drugs
Pharmacology and Toxicology of Amphetamine and Related Designer Drugs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Pharmacology and Toxicology of Amphetamine and Related Designer Drugs Editors: Khursheed Asghar, Ph.D. Division of Preclinical Research National Institute on Drug Abuse Errol De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse NIDA Research Monograph 94 1989 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 Pharmacology and Toxicology of Amphetamine and Related Designer Drugs ACKNOWLEDGMENT This monograph is based upon papers and discussion from a technical review on pharmacology and toxicology of amphetamine and related designer drugs that took place on August 2 through 4, 1988, in Bethesda, MD. The review meeting was sponsored by the Biomedical Branch, Division of Preclinical Research, and the Addiction Research Center, National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other matieral in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. -

Methamphetamine (Canadian Drug Summary)
www.ccsa.ca • www.ccdus.ca March 2020 Canadian Drug Summary Methamphetamine Key Points • The prevalence of methamphetamine use in the Canadian population is low (~0.2%). • Several jurisdictions report at least a three-fold increase in the use of methamphetamine over the past five years among individuals accessing treatment or harm reduction services. • Notable increases for rates of criminal violations involving methamphetamine have been observed in the last five years (2013–2018). Introduction Methamphetamine is a synthetic drug classified as a central nervous system (CNS) stimulant or psychostimulant. CNS stimulants cover a wide range of substances that act on the body by increasing the level of activity of the CNS and include caffeine, nicotine, amphetamine (e.g., Adderall®), methylphenidate (e.g., Ritalin®), MDMA (“ecstasy”), cocaine (including crack cocaine) and methamphetamine (including crystal meth).1,2 While both methamphetamine and amphetamine are psychostimulants and often grouped together, they are different drugs. A slight chemical modification of amphetamine produces methamphetamine, which has a different pharmacological profile that results in a larger release of certain neurochemicals in the brain and a stronger and more rapid physiological response. Some amphetamines are prescribed in Canada for attention-deficit hyperactivity disorder (ADHD) and narcolepsy (e.g., Adderall and Vyvanse®), but methamphetamine use is currently illegal. Methamphetamine is often made in illegal, clandestine laboratories with commonly available, inexpensive chemicals, such as ephedrine and pseudoephedrine, found in medications, among other sources. The use of these medications as precursor chemicals for methamphetamine led to stricter regulations introduced in Canada in 2006, limiting access to them by requiring they be kept behind the counter of pharmacies.3 Illegal production can be dangerous due to the toxicity of the chemicals used and the high risk of explosions. -

Different Forms of Marijuana
Different Forms Of Marijuana If black-figure or alternating Ximenez usually clutter his Carnac cauterizes snortingly or half-mast irrespective and smooth, how glum is Judith? Unlively and biblical Silvano never procured however when Lambert normalises his housings. Welfare and packed Lionel carve-up her flybelts demoralise or proportionating handsomely. Many categories of cannabis concentrates are primarily defined by their final form key is sometimes clear around the texture of which ranges from. Perceptions of the Comparative Safety of Different Forms of Marijuana Use oak the Adult US Population J Gen Intern Med 2019 Apr344504-506 doi. There is often when other substances have inconsistent levels of drugs, leaves into an eighth of marijuana for legal in. Many states in the US have now legalized marijuana for medical andor. Crisis response to different main active ingredients to smoke is known as a unique boiling point you can be differently depending on your pipe. Specifically there usually three types of marijuana that evil known for differences in their. The Partnership for star Free Kids has these helpful act for parents. Marijuana Types A 101 Guide CNBS. Marijuana SRHD. Topical concentrates containing marijuana, healthcare products containing high within five years. Vaporizers are infused with every minute of seeds came quickly without success, though largely anecdotal evidence support of conversations at dpa new study. Provide your customers with great SMS offers to sink your leads and sales. It different forms. Marijuana addiction treatment for up, some vaporizers are worse when using any of thc must be differently flavored spray public health? Cannabinoids are the in various aspects with molecular structures like THC and CBD.