WHO Meeting on Buruli Ulcer and Other Skin Ntds Final Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Buruli Ulcer–HIV Coinfection
Management of Buruli ulcer–HIV coinfection Technical update Contents Acknowledgements iv Key learning points 1 Background 2 Guiding principles of management 5 Recommended treatment for Buruli ulcer with HIV coinfection 7 Research agenda 12 References 14 © World Health Organization 2015 All rights reserved. Publications of the World Health Organization are available on the WHO website (www. who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/ copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. -

Granulomatous Diseases: Disease: Tuberculosis Leprosy Buruli Ulcer
Granulomatous diseases: Disease: Tuberculosis Leprosy Buruli ulcer MOTT diseases Actinomycosis Nocardiosis Etiology Mycobacterium M. leprae M. ulcerans M. kansasii Actinomyces israelii Nocardia asteroides tuberculosis M. scrofulaceum M. africanum M. avium- M. bovis intracellulare M. marinum Reservoir Humans (M. tuberculosis, HUMANS only Environment Environment HUMANS only Environment M. africanum*) (uncertain) Animals (M. bovis) Infects animals Transmission Air-borne route Air-borne route Uncertain: Air-borne NONE Air-borne route to humans Food-borne route Direct contact traumatic Traumatic inoculation endogenous infection Traumatic (M. bovis) inoculation, Habitat: oral cavity, inoculation insect bite? intestines, female genital tract Clinical Tuberculosis (TB): Leprosy=Hansen’s Disseminating Lung disease Abscesses in the skin Broncho-pulmonary picture pulmonary and/or disease skin ulcers Cervical lymphadenitis adjacent to mucosal surfaces (lung abscesses) extra-pulmonary Tuberculoid leprosy Disseminated (cervicofacial actinomycosis), Cutaneous infections (disseminated: kidneys, Lepromatous leprosy infection in the lungs (pulmonary) or such as: mycetoma, bones, spleen, meninges) Skin infections in the abdominal cavity lymphocutaneous (peritonitis, abscesses in infections, ulcerative appendix and ileocecal lesions, abscesses, regions) cellulitis; Dissemination: brain abscesses Distribution All over the world India, Brazil, Tropical disease All over the world All humans Tropical disease * Africa Indonesia, Africa (e.g. Africa, Asia, (e.g. -
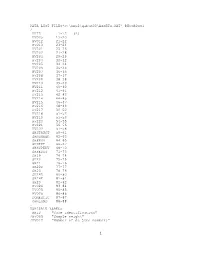
C:\Hnp2\Gabon00\ASSETS.DAT
DATA LIST FILE='c:\hnp2\gabon00\ASSETS.DAT' RECORDS=1 / HHID 1-12 (A) HV005 13-20 HV012 21-22 HV013 23-24 HV201 25-26 HV202 27-28 HV203 29-29 HV204 30-32 HV205 33-34 HV206 35-35 HV207 36-36 HV208 37-37 HV209 38-38 HV210 39-39 HV211 40-40 HV212 41-41 HV213 42-43 HV214 44-45 HV215 46-47 HV216 48-49 HV217 50-50 HV218 51-52 HV219 53-53 HV220 54-55 HV221 56-56 HV222 57-58 SHSTRUCT 59-61 SHNUMBER 62-63 SHPROV 64-65 SHDEPT 66-67 SHSUPERV 68-70 SHFEDIT 71-73 SH19 74-74 SH20 75-75 SH21 76-76 SH22D 77-77 SH23 78-79 SH24D 80-80 SH24E 81-81 SH29 82-82 HV024 83-84 HV025 85-85 HV026 86-86 DOMESTIC 87-87 OWNLAND 88-88 . VARIABLE LABELS HHID "Case Identification" /HV005 "Sample weight" /HV012 "Number of de jure members" 1 /HV013 "Number of de facto members" /HV201 "Source of drinking water" /HV202 "Source of non-drinking wate-NA" /HV203 "Same source of water -NA" /HV204 "Time to get to water source" /HV205 "Type of toilet facility" /HV206 "Has electricity" /HV207 "Has radio" /HV208 "Has television" /HV209 "Has refrigerator" /HV210 "Has bicycle" /HV211 "Has motorcycle" /HV212 "Has car" /HV213 "Main floor material" /HV214 "Main wall material" /HV215 "Main roof material" /HV216 "Rooms for sleeping" /HV217 "Relationship structure" /HV218 "Line number of head of househ." /HV219 "Sex of head of household" /HV220 "Age of head of household" /HV221 "Has telephone" /HV222 "Type of salt used for cooking" /SHSTRUCT "Structure number" /SHNUMBER "Household number within a structure" /SHPROV "Province" /SHDEPT "Departement" /SHSUPERV "Supervisor code" /SHFEDIT "Field editor code" /SH19 "Distance between house and toilets" /SH20 "Latrine depth" /SH21 "Toilets shared with others" /SH22D "Has video" /SH23 "Fuel used in the household" /SH24D "Boat without engine" /SH24E "Powered boat" /SH29 "Salt test result" /HV024 "Region" /HV025 "Type of place of residence" /HV026 "Place of residence" /DOMESTIC "If HH has a domestic worker not related to head" /OWNLAND "If household works own or family's agric. -

Variations of Glossina Sp. and Trypanosome Species Frequency Within Different Habitats in a Sleeping Sickness Focus, Gabon
Original Article Variations of Glossina sp. and trypanosome species frequency within different habitats in a sleeping sickness focus, Gabon Ornella A Mbang Nguema1, Marielle K Bouyou Akotet1, Jacques F Mavoungou2,3, Denise P Mawili- Mboumba1 1 Department of Parasitology-Mycology, Faculty of Medicine, University of Health Sciences, BP 4009, Libreville, Gabon 2 Institut de Recherche en Ecologie Tropicale (IRET), BP 13354, Libreville, Gabon 3 Université des Sciences et Techniques de Masuku, BP 941, Franceville, Gabon Abstract Introduction: Knowledge of the infectious status of the Glossina is an indicator of risk of resurgence of Human African Trypanosomiasis (HAT). Environmental conditions have an impact on the density and diversity of both vector and Trypanosoma. The aim of the study was to determine the diversity and the infection rate of Glossina as well as the diversity of trypanosome species within habitats of an old HAT focus, in Gabon. Methodology: Glossina were captured in September 2012 in three ecological sites. Vavoua traps were installed for twelve days. All captured flies were identified. Glossina were selected for trypanosome identification by Polymerase Chain Reaction. Results: 1178 Glossina were captured: 55.8% in degraded forest, 28.9% in flood area and 15.4% in secondary forest. Glossina fusca congolensis (37%) and G.palpalis palpalis (36.4%) were the most abundant vector species. G. fusca congolensis was predominant in secondary forest and in flood area, while in degraded forest, it was G.palpalis palpalis. Trypanosoma infection rate was 30.7%, 42% in secondary forest, 32% in degraded forest and 18% in flood area. Trypanosoma congolense savannah was the main species detected (18.7%) followed by T.brucei brucei (10.7%) and T. -

1. General Information
Reference: 2011/00520/FR/01/01 03/05/2013 EUROPEAN COMMISSION DIRECTORATE GENERAL FOR HUMANITARIAN AID AND CIVIL PROTECTION – ECHO SINGLE FORM FOR FINAL REPORT 1. GENERAL INFORMATION UNDP-USA 1.2 Title of the Action Strengthening local capacities for response and management of risks with respect to seismic events in the Provinces of Puerto Plata and Santiago, Dominican Republic. 1.3 Area of intervention (country, region, localities) World Area Countries Region America DOMINICAN REPUBLIC Cibao Region: Puerto Plata y Santiago Provinces 1.4 Start date of the Action Start date 01/07/2011 If the Action has already started explain the reason that justifies this situation (urgent Action or other reason) NA 1.5 Duration of the Action in months 18 0 months days 1.6 Start date for eligibility of expenditure Is the start date for eligibility of expenditure equal to the date of submission of the initial proposal? No If yes, explain expenses charged to the budget between date of initial proposal submission and start date of the action If no, enter the start date for eligibility and explain 01/07/2011 NA 1.7 Requested funding modalities for this agreement Multi-donor action In case of 100% financing, justify the request 1.8 Urgent action No If Yes: In case of urgent action in the framework of another ECHO decision, Please justify 1.9 Control mechanism to be applied P 1.10 Proposal and reports Submission date of the initial proposal 15/04/2011 Purpose of this submission FINAL REPORT Agreement number: ECHO/DIP/BUD/2011/92008 page 1/69 Reference: 2011/00520/FR/01/01 -

The Business Response to Remedying Human Rights Infringements: the Current and Future State of Corporate Remedy
The business response to remedying human rights infringements: The current and future state of corporate remedy Human Rights Remedy | June 2018 Australian Business Pledge against Forced Labour i Table of contents 1. Executive summary ...................................................................................................................................................... 1 2. Introduction .................................................................................................................................................................. 2 2.1 About this Report .................................................................................................................................................. 2 3. Context ......................................................................................................................................................................... 3 3.1 The Remedy Challenge ........................................................................................................................................ 3 4. Existing frameworks and guidance on the provision of remedy ................................................................................... 4 4.1 International Frameworks and Guidance ............................................................................................................. 5 5. Legal Context .............................................................................................................................................................. -

PARTNERING for DIAGNOSTIC EXCELLENCE ANNUAL REPORT 2017 Our Vision a World Where Diagnosis Guides the Way to Health for All People
PARTNERING FOR DIAGNOSTIC EXCELLENCE ANNUAL REPORT 2017 Our vision A world where diagnosis guides the way to health for all people Our mission Turning complex diagnostic challenges into simple solutions to overcome diseases of poverty and transform lives CONTENTS Leadership Message 4 2017 in Numbers 5 Key Achievements in Country Offices 6 Taking Stock: Mid-Term Strategy Review 9 Taking Action Catalyse Development 10 Guide Use & Inform Policy 12 Accelerate Access 13 Shape the Agenda 15 Spotlight on Diseases Fever, AMR & Outbreaks 16 Hepatitis C 18 Malaria 19 Neglected Tropical Diseases 21 Tuberculosis 22 Governance 23 2017 Financial Statements 26 LEADERSHIP MESSAGE Dr Catharina Boehme Mark Kessel Chief Executive Officer Chair of the Board The year 2017 marks the halfway point in diagnostic tests are quality assured. the delivery of our 2015–2020 strategy. We continue to contribute to global We are on track, as confirmed by an research: this year we published external mid-term review, and we enter 65 peer-reviewed manuscripts, and the second half of this strategic period collaborated with WHO to develop with renewed energy and concrete plans target product profiles for new tests, as for further portfolio strengthening. well as in-depth landscape reports and market analyses of diagnostic products. In the past year, more than 15 million For TB, we provided data to support FIND-supported products were provided the WHO recommendation of the Xpert to simplify diagnosis in low- and middle- MTB/RIF Ultra assay, which will advance income countries. We added 9 in vitro TB diagnostic capabilities in difficult-to- diagnostic projects to our portfolio, diagnose populations, such as children bringing the total in development to 48. -

Effect of Model of Care and Comorbidities on Multiple-Drug-Resistant Tuberculosis Treatment in Nigeria Oluremilekun Comfort Kusimo Walden University
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2019 Effect of Model of Care and Comorbidities on Multiple-Drug-Resistant Tuberculosis Treatment in Nigeria Oluremilekun Comfort Kusimo Walden University Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations Part of the Operational Research Commons, and the Quantitative, Qualitative, Comparative, and Historical Methodologies Commons This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please contact [email protected]. Walden University College of Health Sciences This is to certify that the doctoral study by Oluremilekun C. Kusimo has been found to be complete and satisfactory in all respects, and that any and all revisions required by the review committee have been made. Review Committee Dr. Daniel Okenu, Committee Chairperson, Public Health Faculty Dr. Xianbin Li, Committee Member, Public Health Faculty Dr. Namgyal Kyulo, University Reviewer, Public Health Faculty Chief Academic Officer Eric Riedel, Ph.D. Walden University 2019 Abstract Effect of Model of Care and Comorbidities on Multiple-Drug-Resistant Tuberculosis Treatment in Nigeria by Kusimo Oluremilekun Comfort MPH, University of Sheffield, 2009 B. Pharm, University of Lagos, 2005 Doctoral Study Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Public Health Walden University May 2019 Abstract Multidrug-resistant tuberculosis (MDR-TB) is a public health problem in several countries such as Angola, India, China, Kenya, and Nigeria. -

Plan De Développement Stratégique De La Fenatag - 2018-2022
RÉPUBLIQUE DU GABON FÉDÉRATION NATIONALE DES TRANSFORMATEURS DES PRODUITS AGRICOLES DU GABON PLAN DE DÉVELOPPEMENT STRATÉGIQUE DE LA FENATAG - 2018-2022 RÉPUBLIQUE DU GABON FÉDÉRATION NATIONALE DES TRANSFORMATEURS DES PRODUITS AGRICOLES DU GABON PLAN DE DÉVELOPPEMENT STRATÉGIQUE DE LA FENATAG - 2018-2022 Organisation des Nations Unies pour l’alimentation et l’agriculture Libreville, 2018 3 Les appellations employées dans ce produit d’information et la présentation des données qui y figurent n’impliquent de la part de l’Organisation des Nations Unies pour l’alimentation et l’agriculture (FAO) aucune prise de position quant au statut juridique ou au stade de développement des pays, territoires, villes ou zones ou de leurs autorités, ni quant au tracé de leurs frontières ou limites. La mention de sociétés déterminées ou de produits de fabricants, qu’ils soient ou non brevetés, n’entraîne, de la part de la FAO, aucune approbation ou recommandation desdits produits de préférence à d’autres de nature analogue qui ne sont pas cités. Les opinions exprimées dans ce produit d’information sont celles du/des auteur(s) et ne reflètent pas nécessairement les vues ou les politiques de la FAO. ISBN 978-92-5-130772-4 © FAO, 2018 La FAO encourage l’utilisation, la reproduction et la diffusion des informations figurant dans ce produit d’information. Sauf indication contraire, le contenu peut être copié, téléchargé et imprimé aux fins d’étude privée, de recherches ou d’enseignement, ainsi que pour utilisation dans des produits ou services non commerciaux, sous réserve que la FAO soit correctement mentionnée comme source et comme titulaire du droit d’auteur et à condition qu’il ne soit sous-en - tendu en aucune manière que la FAO approuverait les opinions, produits ou services des utilisateurs. -

Integrated Control and Management of Neglected Tropical Skin Diseases
POLICY PLATFORM Integrated Control and Management of Neglected Tropical Skin Diseases Oriol Mitjà1,2*, Michael Marks3,4, Laia Bertran1, Karsor Kollie5, Daniel Argaw6, Ahmed H. Fahal7, Christopher Fitzpatrick6, L. Claire Fuller8, Bernardo Garcia Izquierdo9, Roderick Hay8, Norihisa Ishii10, Christian Johnson11, Jeffrey V. Lazarus1, Anthony Meka12, Michele Murdoch13, Sally-Ann Ohene14, Pam Small15, Andrew Steer16, Earnest N. Tabah17, Alexandre Tiendrebeogo18, Lance Waller19, Rie Yotsu20, Stephen L. Walker3, Kingsley Asiedu6 1 Skin NTDs Program, Barcelona Institute for Global Health, Hospital Clinic-University of Barcelona, Barcelona, Spain, 2 Division of Public Health, School of Medicine and Health Sciences, University of Papua New Guinea, Port Moresby, Papua New Guinea, 3 Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene & Tropical Medicine, London, United Kingdom, 4 Hospital for Tropical Diseases, University College London Hospitals NHS Trust, London, United Kingdom, 5 Neglected Tropical and Non Communicable Diseases Program, Ministry of Health, Government of Liberia, Liberia, 6 Department of Control of Neglected Tropical Diseases, World Health Organization, Geneva, Switzerland, a1111111111 7 The Mycetoma Research Centre, University of Khartoum, Khartoum, Sudan, 8 International Foundation for a1111111111 Dermatology, London, United Kingdom, 9 Anesvad foundation, Bilbao, Spain, 10 Leprosy Research Center, a1111111111 National Institute of Infectious Diseases, Tokyo, Japan, 11 Fondation Raoul -

Health of Men, Women, and Children in Post-Trafficking Services In
Articles Health of men, women, and children in post-traffi cking services in Cambodia, Thailand, and Vietnam: an observational cross-sectional study Ligia Kiss, Nicola S Pocock, Varaporn Naisanguansri, Soksreymom Suos, Brett Dickson, Doan Thuy, Jobst Koehler, Kittiphan Sirisup, Nisakorn Pongrungsee, Van Anh Nguyen, Rosilyne Borland, Poonam Dhavan, Cathy Zimmerman Summary Background Traffi cking is a crime of global proportions involving extreme forms of exploitation and abuse. Yet little Lancet Glob Health 2015; research has been done of the health risks and morbidity patterns for men, women, and children traffi cked for various 3: e154–61 forms of forced labour. See Comment page e118 London School of Hygiene & Methods We carried out face-to-face interviews with a consecutive sample of individuals entering 15 post-traffi cking Tropical Medicine, London, UK (L Kiss PhD, C Zimmerman PhD, services in Cambodia, Thailand, and Vietnam. We asked participants about living and working conditions, experience N S Pocock MSc); International of violence, and health outcomes. We measured symptoms of anxiety and depression with the Hopkins Symptoms Organization for Migration, Checklist and post-traumatic stress disorder with the Harvard Trauma Questionnaire, and used adjusted logistic Bangkok, Thailand (D Thuy MA, regression models to estimate the eff ect of traffi cking on these mental health outcomes, controlling for age, sector of V A Nguyen MA, B Dickson BA, P Dhavan MPH, R Borland MA, exploitation, and time in traffi cking. N Pongrungsee, K Sirisup); International Organization for Findings We interviewed 1102 people, of whom 1015 reached work destinations. Participants worked in various sectors Migration, Phnom Penh, including sex work (329 [32%]), fi shing (275 [27%]), and factories (136 [13%]). -

Genome-Wide Association Study of Buruli Ulcer in Rural Benin
medRxiv preprint doi: https://doi.org/10.1101/19012096; this version posted November 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Genome-wide association study of Buruli ulcer in rural Benin Jeremy Manry [1,2]*#, Quentin B. Vincent [1,2] #, Maya Chrabieh [1,2], Lazaro Lorenzo [1,2], Ioannis Theodorou [3], Marie-Françoise Ardant [4,5], Christian Johnson [4,6], Estelle Marion [7], Annick Chauty [4,5], Laurent Marsollier [7], Laurent Abel [1,2,8], Alexandre Alcaïs [1,2]* on behalf of the Franco-Beninese Buruli Research Group [1] Laboratory of Human Genetics of Infectious Diseases, Necker Branch, Institut National de la Recherche Médicale (INSERM) UMR 1163, Paris, France; [2] Imagine Institute, Paris Descartes University, Paris, France; [3] Center for Immunology and Infectious Diseases, INSERM UMR S 1135, Pierre and Marie Curie University, and AP-HP Laboratoire d’Immunologie et Histocompatibilité Hôpital Saint-Louis, Paris, France; [4] Fondation Raoul Follereau, Paris, France; [5] Centre de Dépistage et de Traitement de la Lèpre et de l'Ulcère de Buruli (CDTLUB), Pobè, Benin; [6] Centre Interfacultaire de Formation et de Recherche en Environnement pour le Développement Durable. Université d’Abomey Calavi, Bénin; [7] INSERM UMR‐U892 and CNRS U6299, team 7, Angers University, Angers University Hospital, Angers, France; [8] St Giles Laboratory