Making Football Safer: Optimizing the Efficacy and Implementation of the 11+ Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Legislative Assembly
25138 LEGISLATIVE ASSEMBLY Thursday 2 September 2010 __________ The Speaker (The Hon. George Richard Torbay) took the chair at 10.00 a.m. The Speaker read the Prayer and acknowledgement of country. BUSINESS OF THE HOUSE Notices of Motions General Business Notices of Motions (General Notices) given. ADOPTION AMENDMENT (SAME SEX COUPLES) BILL 2010 (No. 2) Agreement in Principle Debate resumed from 1 September 2010. Mr BARRY O'FARRELL (Ku-ring-gai—Leader of the Opposition) [10.01 a.m.]: In line with usual practice Liberal-National party members of Parliament have a conscience vote on the Adoption Amendment (Same Sex Couples) Bill 2010 (No. 2) on the basis of their views and the assessment of their consideration of the issues involved. I have high regard for conscience votes on issues like this where personal beliefs, political philosophy and community mores intersect. It is important that all members of Parliament think long and hard before casting their votes. Another benefit of these types of votes is the fact that debates like this are also generally conducted with a maximum of reason and tolerance. As deeply as we hold our views, as much as we may disagree with each other, we must surely respect each member's right to his or her own conscientious views. That respect is the reason I have declined, until now, to indicate my position on this legislation. In accordance with my usual practice on conscience votes, I have left my colleagues to form their views and make their decisions, free of any influence from their party leader. -

2021 R05 – Wollongong Wolves FC V Northbridge Bulls FC
KICKOFF 2021 - ROUND 05 SUNDAY 28TH MARCH WIN STADIUM 1PM MEN’S CORPORATE PARTNERS 2 #NPLNSW CONTENTS WOLLONGONG WOLVES COACHING STAFF & MANAGEMENT 1st Team Coach Luke Wilkshire 1st Grade Assistant Coach Stephen O’Connor Senior Manager Mark Wilkshire Under 20s Coach Matheus Scapin Under 20s Assistant Coach Daniell Zeleny Under 20s Manager Jorge Perez GK Coach John Krajnovic Chairman Tory Lavalle Match Preview 6 Health and Medical Services Figtree Physiotherapy Technical Director Neil Mann Team Lineups 22 Admin Manager Susan Gatt Season Draw - Home Games 36 Program Contributors Malcolm Rowney Photographer - Seniors Pedro Garcia Photographer – Juniors Chris Horn For advertising opportunities, please contact Susan Gatt @ [email protected]. This program is proudly printed by WOLVES SHOP Fraternity Club, 11 Bourke Street, Fairy Meadow Public Notices: • Entry inside the perimeter fence of the playing area is prohibited at all times and offenders will be prosecuted. • All spectators are requested to vacate the ground within 15 minutes of the end of the final game. Police may be requested to remove any unauthorised people who remain after the stipulated time. • The setting alight of, or the lighting or discharging of any type of object, including fireworks, signal or smoke flares is strictly prohibited. Offenders will be arrested and charged. Website: wollongongwolves.com.au Email: [email protected] Address: 32 Waverley Drive Unanderra NSW 2526 Twitter: @wollgongwolves Facebook: fb.com/wollongongwolves Instagram: @WollongongWolves NPLNSW.COM.AU 3 FROM THE COACH Welcome to WIN Stadium for our second doubler Northbridge have a young side and we will header with Wellington Phoenix. We are looking be looking to pressure them in possession, be forward to today, with the Phoenix taking on physically strong and move the ball about quickly. -

To View the TAFE NSW Waratah Cup 2019 Match Day Program
KICKOFF GRAND FINAL SUNDAY 14 JULY 2019 2.30PM LILY HOMES STADIUM ® V WELCOME Welcome to the 2019 TAFE NSW Waratah Cup Final, Today only two teams remain, both of whom are an opportunity that will see two very historic football elite NPL NSW Men’s clubs. teams in the Marconi Stallions and Sydney United 58 grab Football NSW’s first piece of silverware. Both teams immersed in Australian football history, the Marconi Stallions battle neighbours Sydney It’s been an amazing year for TAFE NSW Waratah United 58 in what promises to be a titanic battle Cup and it all will come to a climax today at Lily between two highly rated and talented teams. Homes Stadium, home of Blacktown City FC. Cup Finals always produce an entertaining spectacle Over 100 clubs – including Association teams from and this year’s combatants will be no exception. across NSW and teams from the NPL NSW Men’s, NPL 2 NSW Men’s, NPL 3 NSW Men’s and State I would like to extend a huge congratulations to all League Men’s, participated in what has been a great teams involved in this season’s TAFE NSW Waratah campaign to date. Cup for their participation and support of this historic tournament. The TAFE NSW Waratah Cup represents the wonderful history of the game in New South Wales, Finally a big thank you to the fans for your and each year there are fairytale stories of local tremendous support today and throughout the association teams beating their more favoured State season. League opposition. -
2017-Year-In-Review.Pdf
FOOTBALL SOUTH COAST YEAR IN 2017REVIEW Football South Coast – 2017 Year in Review Cntents PAG Chairmans Report FSC Board 6 Cs Report 7 Council embers 1 ead o Council Reports Junior Football Council 15 ens Football Council 17 Womens Football Council 1 Reerees Council 21 echnical irectors Report 2 onour Roll Junior Competition 2 ens Premiership 1 ens Community eague 5 Womens Competition 7 Award Winners ens Premiership ens Community eague 2 Womens Competition FSW Competition onour Roll 5 ie embers 6 Contribution to Football Recipients 7 Summer Football 51 Sponsors 52 FSW State Cup Grand Final Winners 5 Page | 1 Football South Coast – 2017 Year in Review Contents PAGE Chairman’s Report 3 FSC Board 6 CEO’s Report 7 Council Members 14 Head of Council Reports Junior Football Council 15 Men’s Football Council 17 Women’s Football Council 19 Referee’s Council 21 Technical Directors Report 23 Honour Roll Junior Competition 28 Men’s Premiership 31 Men’s Community League 35 Women’s Competition 37 Award Winners Men’s Premiership 39 Men’s Community League 42 Women’s Competition 43 FNSW Competition Honour Roll 45 Life Members 46 Contribution to Football Recipients 47 Summer Football 51 Sponsors 52 FNSW State Cup Grand Final Winners 53 Page | 1 Football South Coast – 2017 Year in Review Football South Coast – 2017 Year in Review Chairman’s Report Hi everyone. Welcome back to FSC – and if you are new to FSC – then welcome to this big diverse family. You may recall that last year I wrote about success, achievements and credibility and how we measure these. -

2019-Annual-Report-Lores.Pdf
Football South Coast – 2018 Year in Review Contents PAGE Chairman’s Report 3 FSC Board 6 CEO’s Report 7 Council Members 12 Head of Council Reports Junior Football Council 13 Men’s Football Council 15 Women’s Football Council 19 Referee’s Council 21 Technical Director’s Report 23 Honour Roll Junior Competition 27 Men’s Premiership 29 Men’s Community League 32 Women’s Competition 34 Award Winners Men’s Premiership 36 Men’s Community League 39 Women’s Competition 41 FNSW Competition Honour Roll 44 Life Members 45 Contribution to Football Recipients 46 Summer Football 50 Indigenous Football 51 FNSW Competitions – Grand Final Winners 52 Sponsors 54 Page | 1 1 Football South Coast – 2018 Year in Review (Pictured above – Clubs involved in the 2018 Junior Grand Finals which were held at Myimbarr Sports fields in Shellharbour) Page | 2 2 Football South Coast – 2018 Year in Review Chairman’s Report Hi Everyone. Welcome back to the FSC Community Family. This year sees our community much bigger, covering a wider area of the region and includes many more members of our diverse community than ever before. And that shows the success of our sport as the leading inclusive participation sport of the region and the nation. I am proud to say that as I wrote last year, and as I have been stating over the last few years, FSC – as an organisation and as a Board assesses our performance as an association on 3 benchmarks. SUCCESS in our game (on & off the field of play including Governance, Communication and Leadership), ACHIEVEMENTS in developing, progressing & advancing our sport & its competitions (Junior Boys & Girls Development & Pathways, Club Infra-Structure & Facilities, Community Inclusion Programmes & Quality Competitions) and finally CREDIBILITY and trust within our Communities (Government MPs & Councillors, Business Sector, Social/Charities Organisations, the Football Community and of course our fabulous Club Members). -

2017 Round 09 Wollongong Wolves V Bonnyrigg White
KICKOFF ROUND 9 SUNDAY WIN STADIUM V 7TH MAY 2017 FIXTURES TEAM LISTS FIRST GRADE MATCH PREVIEW 3PM TEAM OF THE WEEK #PS4NPLNSW CORPORATE PARTNERS 2 CONTENTSHEADING NPLNSW.COM.AU WOLLONGONG WOLVES COACHING STAFF & MANAGEMENT 1st Team Coach Jacob Timpano 1st Grade Assistant Coach Neil Mann and Alfredo Esteves Senior Managers Robert Positti and Surit Wadhwa Under 20s Coach Julio Miranda Under 18s Coach Richard Lloyd GK Coach John Krajnovic Match Preview 6 Health and Medical Services Figtree Physiotherapy Technical Director Neil Mann Team Lineups 18 CEO Chris Papakosmas 2017 Ladder 19 Admin Manager Susan Gatt Season Draw 30 Program Contributors Malcolm Rowney Photographer - Seniors Pedro Garcia Photographer – Juniors Chris Horn Ground Announcer Kevin Morrissey For advertising opportunities, please contact This program is proudly Susan Gatt on 4225 0999. printed by WOLVES SHOP 105 Crown Street Wollongong Public Notices: • Entry inside the perimeter fence of the playing area is prohibited at all times and offenders will be prosecuted. • All spectators are requested to vacate the ground within 15 minutes of the end of the final game. Police may be requested to remove any unauthorised people who remain after the stipulated time. • The setting alight of, or the lighting or discharging of any type of object, including fireworks, signal or smoke flares is strictly prohibited. Offenders will be arrested and charged. Website: wollongongwolves.com.au Email: [email protected] Phone: +61 2 4225 0999 Phone: 105 Crown St Wollongong NSW 2500 Twitter: @wollgongwolves Facebook: fb.com/wollongongwolves Instagram: @WollongongWolves 3 SPONSORS #PS4NPLNSW 4 WELCOME NPLNSW.COM.AU FROM THE elcome everyone to our Round 9 fixture against and software solutions with the Wollongong Wolves WBonnyrigg White Eagles. -
Year in Review 2016
YEAR IN REVIEW 2016 Football South Coast – 2016 Year in Review Contents PAGE Chairman’s Report 3 FSC Board 5 CEO’s Report 6 Council Members 10 Head of Council Reports Junior Football Council 11 Men’s Football Council 13 Women’s Football Council 15 Referee’s Council 16 Technical Directors Report 18 Honour Roll Junior Competition 23 Men’s Premiership 26 Men’s Community League 29 Women Competition 31 Award Winners Men’s Premiership 34 Men’s Community League 37 Women’s Competition 38 FNSW Competition Honour Roll 40 Life Members 41 Contribution to Football Recipients 42 Summer Football 45 Sponsors 46 Page | 1 Football South Coast – 2016 Year in Review Page | 2 Football South Coast – 2016 Year in Review Chairman’s Report Success, Achievement and Credibility. How do we measure these 3-key benchmarks? Well I think knowing that our local football family is growing and expanding its reach across our community so fast and is now the biggest participation sport in Australia and the Illawarra Region is one of the most important and satisfying aspects of being given the privilege of being Chairman of a great Board of Directors in running a great Sports Association in Football South Coast. Of course success is not measured by one event, nor is achievement and certainly credibility is not measured by one event – all 3 must be ongoing and – just like a Football Club - just winning the first game of the season does NOT make you successful, but winning the championship makes everyone successful - but only for that season. So FSC can demonstrate success across many areas of our great game – but it does not stop – and like that football club, there’s the next match, the next season and the years ahead. -
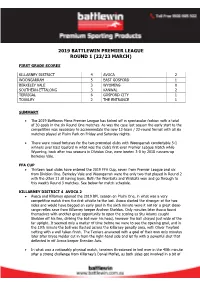
BPL RD1 Wrap-Up
2019 BATTLEWIN PREMIER LEAGUE ROUND 1 (22/23 MARCH) FIRST GRADE SCORES KILLARNEY DISTRICT 4 AVOCA 2 WOONGARRAH 5 EAST GOSFORD 1 BERKELEY VALE 3 WYOMING 0 SOUTHERN-ETTALONG 3 KANWAL 2 TERRIGAL 6 GOSFORD CITY 1 TOUKLEY 2 THE ENTRANCE 1 SUMMARY • The 2019 Battlewin Mens Premier League has kicked off in spectacular fashion with a total of 30 goals in the six Round One matches. As was the case last season the early start to the competition was necessary to accommodate the new 12-team / 22-round format with all six matches played at Pluim Park on Friday and Saturday nights. • There were mixed fortunes for the two promoted clubs with Woongarrah comfortable 5-1 winners over East Gosford in what was the club’s first-ever Premier League match while Wyoming, back after two seasons in Division One, were beaten 3-0 by 2018 runners-up Berkeley Vale. FFA CUP • Thirteen local clubs have entered the 2019 FFA Cup, seven from Premier League and six from Division One. Berkeley Vale and Woongarrah were the only two that played in Round 2 with the other 11 all having byes. Both the Wombats and Wildcats won and go through to this week’s Round 3 matches. See below for match schedule. KILLARNEY DISTRICT 4 AVOCA 2 • Avoca and Killarney opened the 2019 BPL season on Pluim One, in what was a very competitive match from the first whistle to the last. Avoca started the stronger of the two sides and would have bagged an early goal in the sixth minute were it not for a great close- range reflex save from Killarney keeper Andrew Sheldon. -

FOOTBALL SOUTH COAST - NEWSLETTER ` Volume: August 2013 Email:[email protected]
FOOTBALL SOUTH COAST - NEWSLETTER ` Volume: August 2013 www.footballsouthcoast.com Email:[email protected] News and Events The Finals are Upon Us! Finals Fever…It starts with our Women’s Finals on the 1st September. Our Junior Grand Finals are on the following weekend (the 7th and 8th September) at Terry Reserve Albion Park. Amateur Grand Finals will be held on the 21st September at Ian McLennan Park, Kembla Grange and football will be back at WIN Stadium with our Illawarra Credit Union / People Care District League Grand Finals on the 28th September and the Illawarra Mercury Premier League Grand Finals on the 29th September. Good luck to all players and clubs involved in the Final Series! Lock in the 14th September – Sydney FC is coming and our Illawarra Mercury Premier League Major Semi Final is the curtain raiser Tickets are selling fast. Make sure you purchase your tickets through Ticketek to see the A-League Preseason game between Sydney FC and the Newcastle Jets. What a great opportunity for our area to see ADP play with some of our very own local stars including Ruben Zadkovic from the Newcastle Jets (pictured) who are now part of this great A-League competition. The Illawarra Premier League First Grade Grand Final Qualifier between Port Kembla and a yet to be determined opponent will be the curtain raiser kicking off at 2:30pm. FOOTBALL SOUTH COAST - NEWSLETTER ` CEO Update Chairman’s Corner What a huge month in our quest for a Home of Congratulations to all the competition winners and Football. First it was announced by our Federal finalists in our Junior, Men’s, Women’s and Labor Government that we were successful in Amateur competitions. -

ILLAWARRA MERCURY PREMIER LEAGUE GRAND FINAL 10Th October 2010 at Crehan Park Cringila Australia’S Best Credit Union...Again!
Raising funds for Breast Cancer Research in conjunction with The National Breast Cancer Foundation Full time and Port Kembla begin celebrating winning 2010 IPL ILLAWARRA MERCURY PREMIER LEAGUE GRAND FINAL 10th October 2010 at Crehan Park Cringila Australia’s Best Credit Union...Again! Love your Team! As a Platinum Sponsor, Peoplecare has something special for IFA football families. Give us a buzz for details. 1800 808 700 Lysaght Peoplecare Limited. A registered private health insurer. ABN: 95 087 648 753 PRESIDENt’s WELCOME It is my pleasure to welcome everyone here today to the 2010 Illawarra Mercury Premier League Grand Final. This has been clearly the most exciting Football Season the Premier League has ever enjoyed and going on this season’s amazing twists & turns, today promises to be one of those great Illawarra Mercury Premier League Grand Finals. For Football lovers, this 2010 Premier League Season has been nothing short of fantastic, it was unquestionably many things but certainly it was very exciting, unpredictable, unexpected, nerve racking and ultimately that final 1 minute of football spread across many Premier League Football fields in the Illawarra Region, was probably the “fitting end” to conclude our Championship in 2010. Today we see 2 great Premier League clubs face-off for the Grand Final Trophy. Historically, Port Kembla has been a Trophy collecting powerhouse of yester year and more recently Dandaloo has swept all before them, similarly collecting every Trophy on offer. As Port Kembla re-emergences from its re-building era, the young, fast and dynamic Port Kembla side comes up against a very powerful, well organised, highly experienced and professional Dandaloo team filled with proven high quality players with a proven football record. -

AT 16-31 Wollongong United FC V
APPEAL TRIBUNAL OF FOOTBALL NEW SOUTH WALES DETERMINATION IN THE FOLLOWING MATTER: Club Wollongong United FC Decision appealed Appeal from the decision of Football South Coast Appeal Committee Date of Decision 16 June 2016 The basis upon which the Sections 9.1(c) & 9.2 of the Football matter is before the Appeals NSW Grievance and Disciplinary Tribunal Regulations, 2016 Ground(s) of Appeal Sections 9.3(d) and (e)(v) of the Football NSW Grievance and Disciplinary Regulations, 2016 Date of Hearing 27 July 2016 Date of Determination 15 August 2016 Appeals Tribunal Members Iain Todd, Chair Graham Turnbull SC, Member David Stanton, Member Introduction and Jurisdiction 1. The Appeals Tribunal (AT) has been established in accordance with sections 4 and 9.1 of the Football NSW Grievance and Disciplinary Regulations, 2016 (FNSW Regulations) to determine appeals from the Disciplinary Committee (DC), the General Purposes Tribunal (GPT) and Member Appeals Committees (MAC). “Body” is defined in the Regulations to mean a body established under section 4 of the Regulations and relevantly includes the purposes of an appeal to the AT, the DC and the GPT. 2. The sole grounds of appeal prescribed by section 9.3 of the FNSW Regulations are as follows: 2 a. a party was not afforded a reasonable opportunity to present its case; b. lack or excess of jurisdiction of a Body or a Member Appeals Committee; c. the decision of a Body or Member Appeals Committee was affected by actual bias; d. the decision was one that was not reasonably open to a Body or Member Appeals Committee having regard to the evidence before the decision- maker; e. -

Wollongong Wolves V North Shore Mariners
KICKOFF 2020 - ROUND 02 ALBERT BUTLER SUNDAY MEMORIAL 8TH MARCH PARK 2.30PM MEN’S CORPORATE PARTNERS 2 #NPLNSW CONTENTS WOLLONGONG WOLVES COACHING STAFF & MANAGEMENT 1st Team Coach Luke Wilkshire 1st Grade Assistant Coach Matheus Vianna Scapin Senior Manager Mark Wilkshire Under 20s Coach Steve O’Connor Under 20s Assistant Coach Icko Atanasoski Under 18s Coach Darren Jones Under 18s Assistant Coach Scott Nichols Under 18s Manager Robbie Day Match Preview 6 GK Coach John Krajnovic Chairman Tory Lavalle Team Lineups 22 Health and Medical Services Figtree Physiotherapy Season Draw 38 Technical Director Neil Mann Admin Manager Susan Gatt Program Contributors Malcolm Rowney Photographer - Seniors Pedro Garcia Photographer – Juniors Chris Horn For advertising opportunities, please contact Susan Gatt on 02 42 722 624. This program is proudly printed by WOLVES SHOP 32 Waverley Drive Unanderra Public Notices: • Entry inside the perimeter fence of the playing area is prohibited at all times and offenders will be prosecuted. • All spectators are requested to vacate the ground within 15 minutes of the end of the final game. Police may be requested to remove any unauthorised people who remain after the stipulated time. • The setting alight of, or the lighting or discharging of any type of object, including fireworks, signal or smoke flares is strictly prohibited. Offenders will be arrested and charged. Website: wollongongwolves.com.au Email: [email protected] Phone: 02 42 722 624 Address: 32 Waverley Drive Unanderra NSW 2526 Twitter: @wollgongwolves Facebook: fb.com/wollongongwolves Instagram: @WollongongWolves NPLNSW.COM.AU 3 FROM THE COACH Welcome to season 2020! Our pre-season was good, if not a little disjointed in mid to late February due to the weather.