Epidemiological Characteristics and Spatiotemporal Analysis Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Thesis
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Across the Geo-political Landscape Chinese Women Intellectuals’ Political Networks in the Wartime Era 1937-1949 Guo, Xiangwei Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT Unless another licence is stated on the immediately following page this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 30. Sep. 2021 Across the Geo-political Landscape: Chinese Women Intellectuals’ Political -

Printmgr File
DIRECTORS, SUPERVISORS AND PARTIES INVOLVED IN THE GLOBAL OFFERING DIRECTORS Name Address Nationality Executive Directors Sun Nengyi No. 2-301 Block 6 Chinese Gulousi Village Nanan District Chongqing City China He Yong 6-2 Unit 3 Chinese No. 1 Yuanbao Village Shuangqiao District Chongqing City China Liao Shaohua No. 12 to No. 130 Chinese Jingjian Village Huaxi Town Banan District Chongqing City China Chen Xianzheng 9-4 Unit 1 Chinese No. 8 Gulouwu Village Nanan District Chongqing City China Non-executive Directors Huang Yong 4-5 Block 25 Chinese No. 1111 Jinkai Road Yubei District Chongqing City China Yu Gang 23-1 Chinese No. 26 Danlong Road Nanan District Chongqing City China 61 DIRECTORS, SUPERVISORS AND PARTIES INVOLVED IN THE GLOBAL OFFERING Name Address Nationality Yang Jingpu 3-2 Block 1 Chinese No. 46-1 Yanyu Castle Nanan District Chongqing City China Wu Jian Unit 1 Chinese No. 9 Daijia Village Yuzhong District Chongqing City China Independent non-executive Directors Lo Wah Wai Duplex C, 19th and 20th Floor Chinese Tower 1, The Astrid 180 Argyle Street Ha Tan Wei Kowloon Hong Kong Ren Xiaochang No. 1 on Level 4 Chinese Unit 1 Block 25 Zhujiang Garden Jiulongpo District Chongqing City China Kong Weiliang 16-4 Chinese No. 2-128 Beixia Road Beibei District Chongqing City China 62 DIRECTORS, SUPERVISORS AND PARTIES INVOLVED IN THE GLOBAL OFFERING Name Address Nationality SUPERVISORS Duan Rongsheng 15-3 Chinese No. 155 Zhongshansan Road Yuzhong District Chongqing City China Ye Zusheng 7-2 Chinese No. 385 Xinhua Road Shizhong District Chongqing City Sichuan Province China Wang Rongxue 1-2 Chinese No. -
Chongqing Handbook All Essential Information You Need to Know About Chongqing
Chongqing Handbook All essential information you need to know about Chongqing Presented by Chongqing Expat Club www.cqexpat.com Copyright 2008. All Rights Reserved. Table of Contents CHAPTER ONE - ABOUT CHONGQING Page 3 CHAPTER TWO – THE CITY HUBS Page 3 CHAPTER THREE – CITY TRANSPORT Page 4 CHAPTER FOUR – ATTRACTIONS Page 6 CHAPTER FIVE – NIGHTLIFE & ENTERTAINMENT Page 16 CHAPTER SIX – ACCOMMODATION Page 18 CHAPTER SEVEN – INTERNATIONAL FOOD Page 21 CHAPTER EIGHT– SHOPPING Page 24 CHAPTER NINE - EDUCATION Page 27 CHAPTER TEN – HEALTH CARE Page 29 CHAPTER ELEVEN – EMBASSIES & CONSULATES Page 31 CHAPTER TWELVE – USEFUL CONTACTS Page 32 CHAPTER THIRTEEN – USEFUL WORDS and PHRASES Page 32 CHAPTER ONE - ABOUT CHONGQING Chongqing is the economic hub of southwest China and the fourth Municipality in China (after Beijing, Shanghai and Tianjin). Chongqing is situated in the east of southwest China, about 2,500km up the Yangtze River from Shanghai. Under its jurisdiction there are 40 districts, cities and counties. It covers an area of 82,000 square kilometres with a total population of 31 million. An estimated 6 million people live in urban Chongqing city. Downtown Chongqing lies at the point where the Yangtze River and the Jialing River merge. Known as the Mountain City, the whole city is built against a backdrop of hills and rivers, characterized by zig-zagging roads and overlapping houses. It is also known as one of the four Furnace Cities for its hot summers and the Foggy City for its misty winters. CHAPTER TWO – THE CITY HUBS Chongqing has five major business and shopping precincts - the oldest and most important being Jiefangbei situated within what remains of the Old Walled City. -

P020200328433470342932.Pdf
In accordance with the relevant provisions of the CONTENTS Environment Protection Law of the People’s Republic of China, the Chongqing Ecology and Environment Statement 2018 Overview …………………………………………………………………………………………… 2 is hereby released. Water Environment ………………………………………………………………………………… 3 Atmospheric Environment ………………………………………………………………………… 5 Acoustic Environment ……………………………………………………………………………… 8 Solid and Hazardous Wastes ………………………………………………………………………… 9 Director General of Chongqing Ecology Radiation Environment …………………………………………………………………………… 11 and Environment Bureau Landscape Greening ………………………………………………………………………………… 12 May 28, 2019 Forests and Grasslands ……………………………………………………………………………… 12 Cultivated Land and Agricultural Ecology ………………………………………………………… 13 Nature Reserve and Biological Diversity …………………………………………………………… 15 Climate and Natural Disaster ……………………………………………………………………… 16 Eco-Priority & Green Development ………………………………………………………………… 18 Tough Fight for Pollution Prevention and Control ………………………………………………… 18 Ecological environmental protection supervision …………………………………………………… 19 Ecological Environmental Legal Construction ……………………………………………………… 20 Institutional Capacity Building of Ecological Environmental Protection …………………………… 20 Reform of Investment and Financing in Ecological Environmental Protection ……………………… 21 Ecological Environmental Protection Investment …………………………………………………… 21 Technology and Standards of Ecological Environmental Protection ………………………………… 22 Heavy Metal Pollution Control ……………………………………………………………………… 22 Environmental -

Haiyu Hot Spring Hotel
Conference Hotel The 13th International Conference on Networking, Architecture, and Storage (NAS 2018) will be held at: Haiyu Hot Spring Hotel No.198 ShuangYuan Avenue, Beibei District, ChongQing, China. TEL: 86-023-63179999 Links: http://hotels.ctrip.com/hotel/445411.html#ctm_ref=www_hp_bs_lst / (Chinese) https://www.trip.com/hotels/chongqing-hotel-detail-445411/haiyu-hotspring-hotel/ (Englisth) Haiyu Hot Spring Hotel is located in Beibei district Chongqing and adjacent to the government and the popular Jialing Flavor pedestrian Street. It has a walking distance from subway line 6, is roughly 40 minutes away via highway from the city center, and is 40 minutes away via highway from the airport. This hotel is a five-star hotel focusing on conference and leisure. The western- style hotel is modern and elegant, designed like a swallow tail. It has 306 various guest rooms. Its International conference center can accommodate up to 1200 people at the same time. The hotel remains a hot spring SPA center, a fitness center, a lobby bar, an exclusive lounge bar, and a business center. We have held some rooms in Haiyu Hot Spring Hotel Chongqing (the conference hotel). The hotel has special prices for NAS2018. To make a reservation please fill in this form. Please check the reservation form and mail to Ms. Wu ([email protected]).The reservation deadline is on September 15, 2018. Near to the hotel, there are many hotels. We also offer the following alternatives. Ji Bei Hotel No.7 YunHua Road, Beibei District, ChongQing, China. TEL: 023-60315678 Links:http://hotels.ctrip.com/hotel/1460697.html?isFull=F#ctm_ref=hod_sr_lst_dl_n_1_1 (Chinese) https://www.trip.com/hotels/chongqing-hotel-detail-1460697/jibei-hotel (English) Authors for conference hotel reservation can contact Ms. -
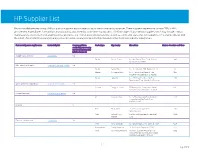
HP Supplier List
HP Supplier List Below is an alphabetized listing of HP production suppliers and information about their sustainability practices. These suppliers represent more than 95% of HP’s procurement expenditures for materials, manufacturing, and assembly at the time of publication. This list includes final assembly suppliers, which may include contract manufacturers, electronic manufacturing service providers, and original design manufacturers, as well as commodity and component suppliers. HP is sharing this list with the intent of promoting transparency and progress in raising social and environmental standards in the electronics industry supply chain. Final assembly parent supplier name Sustainability link Company publishes Product type City, Country Site address Number of workers on HP lines sustainability report using the Global Reporting (GRI) Initiative framework AU Optronics Corporation Sustainability Yes Display Suzhou, China No. 398, Suhong Zhong Road, Suzhou 890 Industrial Park, 215021 BOE Technology Group Co. Corporate Social Responsibility Yes Display Beijing, China No.118 Jinghaiyilu, BDA, Beijing, 100176 50 Display Chongqing, China No. 7, Yunhan Road, Shuitu Hi Tech 950 Industrial Park, Beibei District, 400700 Display Hefei, China No.2177, Great East Road, Xin Zhan 150 Development Zone, Hefei, An Hui Province Cheng Uei Precision Industry Co. Corporate Responsibility Yes Scanner Dongguan, China FIT Industry Park, Yinhe Industrial Area, 1013 Qingxi, Dongguan Guangdong Province Compal Electronics Sustainable Development Yes PC Kunshan, -

Hospital List.Xlsx
Hospitals Participated in Mental Tortures No. 医院名 Hospital Names 地址 Address 省 Province 市 City 联系方式 Contact Information 备注 医院网站 九江市第五人民医院(九江市 Jiujiang City No. 5 People's Hospital 九江市浔阳区白水湖路6号 6 Baishuihu Rd, Xunyang 江西 Jiangxi 九江 Jiujiang 0792-8222656 http://jxjj5y.h. 1 精神病医院) (Jiujiang City Mental Illness Hospital) District, Jiujiang City 51daifu.com/ 九龙坡区精神病医院石坪桥 Shipingqiao Branch of Jiulongpo District 九龙坡区石坪桥正街116号 重庆 Sichuan 重庆 Chongqin 023-68678134 023-68826153 2 116 Shipingqiaozheng St, J 分院 Mental Hospital g 上海市闸北区精神卫生中心 Shanghai city Zhabei District Mental 上海市闸北区普善路247号 247 Pushan Rd,Zhabei 上海 Shanghai 上海 Shanghai 020-56682889 56627963 3 Health Center District, Shanghai 56625327 56723027 上海市金山区精神卫生中心 Shanghai city Jinshan District Mental 上海市金山区金山大道3528号 3528 Jingshan Blvd, 上海 Shanghai 上海 Shanghai 021-57930999\57958771\57934828 4 Health Center Jingshan District, [email protected] Shanghai 大庆市第三人民医院 Daqing City No. 3 People's Hospital 大庆市让胡路区西泰路54号 54 Xitai Rd, Ranghulu 黑龙江 Heilongj 大庆 Daqing 0459-5596185 0459-5595542 http://www.dqxin 5 District, Daqing City iang li.com/ 大连市第七人民医院、大连 Dalian City No. 7 People's Hospital, 大连市甘井子区凌水路179号 179 Lingshui Rd, Jingzi 辽宁 Liaoning 大连 Dalian 0411-84691871 http://www.dl- 6 市心理医院 Dalian City Mental Hospital District, Dalian City qy.com/ 大连市张国礼神经精神医院 Zhang Guoli Mental Hospital, Dalian City 大连市西岗区兴海屯15号 15 Xinghaitun, Xigang 辽宁 Liaoning 大连 Dalian 0411-86760017 0411-86760020 7 District, Dalian City 山西省一零九医院(原公安医 Shanxi Police No.109 Hospital 山西省太原市迎泽区太堡街73 73 Taibao St, Yingze 山西 Shanxi 太原 -

Analysis of the Spatial and Temporal Evolution of Land Cover and Heat Island Effects in Six Districts of Chongqing’S Main City
sensors Article Analysis of the Spatial and Temporal Evolution of Land Cover and Heat Island Effects in Six Districts of Chongqing’s Main City Qin Lang 1, Wenping Yu 1,*, Mingguo Ma 1 and Jianguang Wen 2 1 Chongqing Engineering Research Center for Remote Sensing Big Data Application, School of Geographical Sciences, Southwest University, Chongqing 400715, China; [email protected] (Q.L.); [email protected] (M.M.) 2 Institute of Remote Sensing and Digital Earth, Chinese Academy of Sciences, Beijing 100101, China; [email protected] * Correspondence: [email protected]; Tel.: +86-23-6825-3912 Received: 8 October 2019; Accepted: 25 November 2019; Published: 28 November 2019 Abstract: The urban heat island effect has always been one of the hottest issues in urban development. In this study, Landsat images from the summers of 2001, 2004, 2009, 2014 and 2018 were used to identify land cover type in six districts of Chongqing’s main city. Land cover was categorized as water, vegetation or impervious surface with the object-oriented method. Land surface temperature (LST) data was calculated with the atmospheric radiation transfer equation method, and was then divided into different heat island intensity grades. Next, the spatial and temporal changes in land cover type and heat island effect were analyzed in the six districts. Center migration analysis and heat island coefficients were used to quantitatively reflect the spatiotemporal evolution relationship between land cover and heat island effect. All six districts exhibited a trend of expanding impervious surface, with a 419.38% increase from 2001 to 2018, and shrinking vegetation, with a 17.81% decrease from 2001 to 2018. -

Minimum Wage Standards in China August 11, 2020
Minimum Wage Standards in China August 11, 2020 Contents Heilongjiang ................................................................................................................................................. 3 Jilin ............................................................................................................................................................... 3 Liaoning ........................................................................................................................................................ 4 Inner Mongolia Autonomous Region ........................................................................................................... 7 Beijing......................................................................................................................................................... 10 Hebei ........................................................................................................................................................... 11 Henan .......................................................................................................................................................... 13 Shandong .................................................................................................................................................... 14 Shanxi ......................................................................................................................................................... 16 Shaanxi ...................................................................................................................................................... -

2020 Interim Report
BANK OF CHONGQING CO., LTD.* 重慶銀行股份有限公司* (A joint stock company incorporated in the People's Republic of China with limited liability) (Stock Code: 1963) (Stock Code of Preference Shares: 4616) 2020 INTERIM REPORT * The Bank holds a financial licence number B0206H250000001 approved by the regulatory authority of the banking industry of the PRC and was authorised by the Administration for Market Regulation of Chongqing to obtain a corporate legal person business licence with a unified social credit code 91500000202869177Y. The Bank is not an authorised institution within the meaning of Hong Kong Banking Ordinance (Chapter 155 of the Laws of Hong Kong), not subject to the supervision of the Hong Kong Monetary Authority, and not authorised to carry on banking and/or deposit-taking business in Hong Kong. CONTENTS 1. Definitions 2 2. Corporate Information 4 3. Financial Highlights 5 4. Management Discussions and Analysis 8 4.1 Overview 8 4.2 Financial Review 9 4.3 Business Overview 42 4.4 Employees and Human Resources 54 Management 4.5 Risk Management 56 4.6 Capital Management 61 4.7 Environment and Outlook 64 5. Change in Share Capital and Shareholders 65 6. Directors, Supervisors and Senior Management 73 7. Significant Events 75 8. Report on Review of Interim Financial Information 77 9. Interim Condensed Consolidated Financial 78 Statements and Notes 10. Unaudited Supplementary Financial Information 170 11. Organizational Chart 173 12. List of Branch Outlets 174 Definitions In this report, unless the context otherwise requires, the following terms shall have the meanings set forth below: “Articles of Association” the articles of association of the Bank, as amended from time to time “Bank” or “Bank of Chongqing” Bank of Chongqing Co., Ltd. -

中國內地指定醫院列表 出版日期: 2019 年 7 月 1 日 Designated Hospital List in Mainland China Published Date: 1 Jul 2019
中國內地指定醫院列表 出版日期: 2019 年 7 月 1 日 Designated Hospital List in Mainland China Published Date: 1 Jul 2019 省 / 自治區 / 直轄市 醫院 地址 電話號碼 Provinces / 城市/City Autonomous Hospital Address Tel. No. Regions / Municipalities 中國人民解放軍第二炮兵總醫院 (第 262 醫院) 北京 北京 西城區新街口外大街 16 號 The Second Artillery General Hospital of Chinese 10-66343055 Beijing Beijing 16 Xinjiekou Outer Street, Xicheng District People’s Liberation Army 中國人民解放軍總醫院 (第 301 醫院) 北京 北京 海澱區復興路 28 號 The General Hospital of Chinese People's Liberation 10-82266699 Beijing Beijing 28 Fuxing Road, Haidian District Army 北京 北京 中國人民解放軍第 302 醫院 豐台區西四環中路 100 號 10-66933129 Beijing Beijing 302 Military Hospital of China 100 West No.4 Ring Road Middle, Fengtai District 中國人民解放軍總醫院第一附屬醫院 (中國人民解 北京 北京 海定區阜成路 51 號 放軍 304 醫院) 10-66867304 Beijing Beijing 51 Fucheng Road, Haidian District PLA No.304 Hospital 北京 北京 中國人民解放軍第 305 醫院 西城區文津街甲 13 號 10-66004120 Beijing Beijing PLA No.305 Hospital 13 Wenjin Street, Xicheng District 北京 北京 中國人民解放軍第 306 醫院 朝陽區安翔北里 9 號 10-66356729 Beijing Beijing The 306th Hospital of PLA 9 Anxiang North Road, Chaoyang District 中國人民解放軍第 307 醫院 北京 北京 豐台區東大街 8 號 The 307th Hospital of Chinese People’s Liberation 10-66947114 Beijing Beijing 8 East Street, Fengtai District Army 中國人民解放軍第 309 醫院 北京 北京 海澱區黑山扈路甲 17 號 The 309th Hospital of Chinese People’s Liberation 10-66775961 Beijing Beijing 17 Heishanhu Road, Haidian District Army 中國人民解放軍第 466 醫院 (空軍航空醫學研究所 北京 北京 海澱區北窪路北口 附屬醫院) 10-81988888 Beijing Beijing Beiwa Road North, Haidian District PLA No.466 Hospital 北京 北京 中國人民解放軍海軍總醫院 (海軍總醫院) 海澱區阜成路 6 號 10-66958114 Beijing Beijing PLA Naval General Hospital 6 Fucheng Road, Haidian District 北京 北京 中國人民解放軍空軍總醫院 (空軍總醫院) 海澱區阜成路 30 號 10-68410099 Beijing Beijing Air Force General Hospital, PLA 30 Fucheng Road, Haidian District 中華人民共和國北京市昌平區生命園路 1 號 北京 北京 北京大學國際醫院 Yard No.1, Life Science Park, Changping District, Beijing, 10-69006666 Beijing Beijing Peking University International Hospital China, 東城區南門倉 5 號(西院) 5 Nanmencang, Dongcheng District (West Campus) 北京 北京 北京軍區總醫院 10-66721629 Beijing Beijing PLA. -

出版日期: 2018 年1 月- Designated Hospital List in Mainland China
中國內地指定醫院列表 (((生活守護保障(生活守護保障))) 出版日期: 2018 年年年 1 月月月 Designated Hospital List in Mainland China (Life Impact Reliever) Published Date: Jan 2018 省省省 / 自治區 / 直直直 轄市 Provinces / 城市 醫院 地址 電話號碼 Autonomous City Hospital Address Tel. No. Regions / Municipalities 安徽省 合肥 合肥市第一人民醫院 盧陽區淮河路 390 號 551-2652893 Anhui Hefei Hefei No.1 People's Hospital 390 Huaihe Road, Luyang District 安徽省 合肥 合肥市第二人民醫院 包河區和平路 246 號 551-2203500 Anhui Hefei Hefei No.2 People's Hospital 246 Heping Road, Yaohai District 安徽省 合肥 安徽中醫學院第一附屬醫院 (安徽省中醫院) 蜀山區梅山路 117 號 551-2821852 Anhui Hefei Anhui TCM College No. 1 Hospital 117 Meishan Road, Shushan District 安徽省 合肥 安徽省立兒童醫院 包河區望江東路 39 號 551-2237114 Anhui Hefei Anhui Children's Hospital 39 Wangjiang East Road, Baohe District 安徽省 合肥 安徽省立醫院 廬陽區廬江路 17 號 551-2283114 Anhui Hefei Anhui Hospital 17 Lujiang Road, Luyang District 安徽省 合肥 安徽醫科大學第一附屬醫院 蜀山區績溪路 218 號 551-2922114 Anhui Hefei Anhui Medical University No.1 Hospital 218 Jixi Road, Shushan District 安徽省 合肥 安徽醫科大學第二附屬醫院 經濟技術開發區芙蓉路 678 號 551-3869420 Anhui Hefei Anhui Medical University No.2 Hospital 678 Furong Road, Shushan District 中國中醫科學院廣安門醫院 北京 北京 西城區北線閣 5 號 Guang'anmen Hospital, China Academy of Chinese 10-83123311 Beijing Beijing 5 Beixiange St. Xicheng District Medical Sciences 北京 北京 中國中醫科學院望京醫院 朝陽區花家地街 10-84739047 Beijing Beijing Wangjing Hospital of CACMS Huajiadi Street, Chaoyang District 北京 北京 中國中醫科學院西苑醫院 (西苑醫院) 海澱區西苑操場 1 號 10-62835678 Beijing Beijing Xiyuan Hospital CACMS No.1, Xiyuang Caochang, Haidian District 北京 北京 中國人民解放軍海軍總醫院 (海軍總醫院) 海澱區阜成路 6 號 10-66958114 Beijing Beijing PLA Naval General Hospital 6 Fucheng Road, Haidian District 北京 北京 中國人民解放軍空軍總醫院 (空軍總醫院) 海澱區阜成路 30 號 10-68410099 Beijing Beijing Air Force General Hospital, PLA 30 Fucheng Road, Haidian District 北京 北京 中國人民解放軍第 302 醫院 豐台區西四環中路 100 號 10-66933129 Beijing Beijing 302 Military Hospital of China 100 West No.4 Ring Road Middle, Fengtai District 重要資料: Important Notes: 1.