Procedures in FM
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

The Differences Between ICD-9 and ICD-10
Preparing for the ICD-10 Code Set: Fact Sheet 2 October 1, 2015 Compliance Date Get the Facts to be Compliant Alert: The new ICD-10 compliance date is October 1, 2015. The Differences Between ICD-9 and ICD-10 This is the second fact sheet in a series and is focused on the differences between the ICD-9 and ICD-10 code sets. Collectively, the fact sheets will provide information, guidance, and checklists to assist you with understanding what you need to do to implement the ICD-10 code set. The ICD-10 code sets are not a simple update of the ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and concepts that make them very different from ICD-9. Because of these differences, it is important to develop a preliminary understanding of the changes from ICD-9 to ICD-10. This basic understanding of the differences will then identify more detailed training that will be needed to appropriately use the ICD-10 code sets. In addition, seeing the differences between the code sets will raise awareness of the complexities of converting to the ICD-10 codes. Overall Comparisons of ICD-9 to ICD-10 Issues today with the ICD-9 diagnosis and procedure code sets are addressed in ICD-10. One concern today with ICD-9 is the lack of specificity of the information conveyed in the codes. For example, if a patient is seen for treatment of a burn on the right arm, the ICD-9 diagnosis code does not distinguish that the burn is on the right arm. -
Appendectomy: Simple Appendicitis
Appendectomy: Simple Appendicitis Your child has had an appendectomy (ap pen DECK toe mee). This is the surgical removal of the appendix. The appendix is a small, narrow sac at the beginning of the large intestine (Picture 1). The appendix has no known function. What to Expect After Surgery . Your child will awaken in the Post Anesthesia Care Unit (PACU) near the surgery area. He or she may be in the PACU for 1 to 2 hours. After your child wakes up in the PACU, he or she will return to a hospital room or be Esophagus transferred to the Surgery Unit. Discharge will be directly from the Surgery Unit. Liver Stomach . Your child will have 3 to 4 small incision Large sites (see Helping Hand HH-I-283, Intestines Laparoscopic Surgery (colon) ). Small . Your child will receive fluids and pain intestines medicine through an intravenous line (IV). Rectum When your child can take liquids by mouth, pain medicine will also be given by mouth. Appendix . Your child will need to cough and deep-breathe often to help keep the lungs clear. He or she may use a plastic device called an incentive Picture 1 The appendix inside the body. spirometer to help with this. Your child will need to get up and walk soon after surgery. Walking will help "wake up" the bowels; it will also help with breathing and blood flow. Your child will be able to go home on the same day of the surgery if he or she is: o able to drink clear liquids like water, clear soft drinks, broth, and fruit punch o taking pain medicine by mouth and his or her pain is controlled, and o able to walk. -
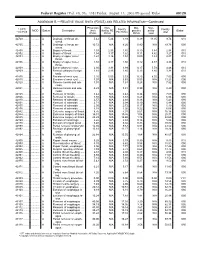
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Incidental Drainage of a Periappendicular Abscess During Colonoscopy
UCTN – Unusual cases and technical notes E175 Incidental drainage of a periappendicular abscess during colonoscopy A 50-year-old man was referred to the of oral metronidazole and ciprofloxacin. A P. Figueiredo, V. Fernandes, J. Freitas outpatient colonoscopy clinic after a posi- computed tomography (CT) scan 1 week Department of Gastroenterology, tive fecal occult blood test during screen- after the procedure revealed no abnormal Hospital Garcia de Orta, Almada, Portugal ing for colorectal cancer. Colonoscopy, findings and the patient remained asymp- which was performed with the patient tomatic. sedated, revealed a 12-mm tumor covered Acute appendicitis is the most frequent References by normal, smooth mucosa at the site of acute abdominal emergency seen in de- 1 Oliak D, Yamini D, Udani VM et al. Can per- forated appendicitis be diagnosed preopera- the appendicular orifice. A biopsy was veloped countries. Its most common com- tively based on admission factors? J Gastro- taken, but this led to an immediate puru- plication is perforation and this may be intest Surg 2000; 4: 470–474 lent discharge occurring from the lesion followed by abscess formation [1]. Colo- 2 Ohtaka M, Asakawa A, Kashiwagi A et al. (●" Video 1). Therefore, a diagnosis of a noscopic diagnosis and treatment of a Pericecal appendiceal abscess with drainage periappendicular abscess was incidentally periappendicular abscess is rare [2]. In during colonoscopy. Gastrointest Endosc 1999; 49: 107–109 established. this case a periappendicular abscess was 3 Antevil J, Brown C. Percutaneous drainage After the patient had recovered from the incidentally discovered and drained dur- and interval appendectomy. In: Scott-Turner sedation, he was specifically questioned ing a colonoscopy. -

Immune Functions of the Vermiform Appendix
The Proceedings of the International Conference on Creationism Volume 3 Print Reference: Pages 335-342 Article 30 1994 Immune Functions of the Vermiform Appendix Frank Maas Follow this and additional works at: https://digitalcommons.cedarville.edu/icc_proceedings DigitalCommons@Cedarville provides a publication platform for fully open access journals, which means that all articles are available on the Internet to all users immediately upon publication. However, the opinions and sentiments expressed by the authors of articles published in our journals do not necessarily indicate the endorsement or reflect the views of DigitalCommons@Cedarville, the Centennial Library, or Cedarville University and its employees. The authors are solely responsible for the content of their work. Please address questions to [email protected]. Browse the contents of this volume of The Proceedings of the International Conference on Creationism. Recommended Citation Maas, Frank (1994) "Immune Functions of the Vermiform Appendix," The Proceedings of the International Conference on Creationism: Vol. 3 , Article 30. Available at: https://digitalcommons.cedarville.edu/icc_proceedings/vol3/iss1/30 IMMUNE FUNCTIONS OF THE VERMIFORM APPENDIX FRANK MAAS, M.S. 320 7TH STREET GERVAIS, OR 97026 KEYWORDS Mucosal immunology, gut-associated lymphoid tissues. immunocompetence, appendix (human and rabbit), appendectomy, neoplasm, vestigial organs. ABSTRACT The vermiform appendix Is purported to be the classic example of a vestigial organ, yet for nearly a century it has been known to be a specialized organ highly infiltrated with lymphoid tissue. This lymphoid tissue may help protect against local gut infections. As the vertebrate taxonomic scale increases, the lymphoid tissue of the large bowel tends to be concentrated In a specific region of the gut: the cecal apex or vermiform appendix. -
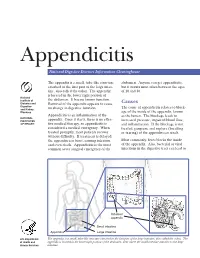
Appendicitis
Appendicitis National Digestive Diseases Information Clearinghouse The appendix is a small, tube-like structure abdomen. Anyone can get appendicitis, attached to the first part of the large intes- but it occurs most often between the ages tine, also called the colon. The appendix of 10 and 30. is located in the lower right portion of National Institute of the abdomen. It has no known function. Diabetes and Removal of the appendix appears to cause Causes Digestive The cause of appendicitis relates to block- and Kidney no change in digestive function. Diseases age of the inside of the appendix, known Appendicitis is an inflammation of the as the lumen. The blockage leads to NATIONAL INSTITUTES appendix. Once it starts, there is no effec- increased pressure, impaired blood flow, OF HEALTH tive medical therapy, so appendicitis is and inflammation. If the blockage is not considered a medical emergency. When treated, gangrene and rupture (breaking treated promptly, most patients recover or tearing) of the appendix can result. without difficulty. If treatment is delayed, the appendix can burst, causing infection Most commonly, feces blocks the inside and even death. Appendicitis is the most of the appendix. Also, bacterial or viral common acute surgical emergency of the infections in the digestive tract can lead to Inflamed appendix Small intestine Appendix Large intestine U.S. Department The appendix is a small, tube-like structure attached to the first part of the large intestine, also called the colon. The of Health and appendix is located in the lower right portion of the abdomen, near where the small intestine attaches to the large Human Services intestine. -

Hospital Confinement Sickness Indemnity Limited Benefit Policy Surgical Benefit
HOSPITAL CONFINEMENT SICKNESS INDEMNITY LIMITED BENEFIT POLICY SURGICAL BENEFIT AFLAC will pay benefits according to the Schedule of Operations when a covered person has a surgical operation performed for a covered sickness in a hospital or ambulatory surgical center. Only one benefit is payable per 24-hour period for surgery even though more than one surgical procedure may be performed. We will pay the highest eligible benefit. Benefits are not payable for cosmetic or elective surgery that is not due to sickness. Surgical Benefits are not payable for surgery performed in a doctor's or dentist's office, clinic, or other such location. Surgery performed but not listed in the Schedule of Operations will be paid according to the amount shown for the surgery most similar in severity and gravity. No lifetime maximum. SCHEDULE OF OPERATIONS BONE DIGESTIVE (cont.) Bone marrow biopsy Gastroscopy ................................... 100 or aspiration ............................. $100 Sigmoidoscopy ............................... 100 Arthroscopy.................................... 150 Appendectomy................................ 200 Removal of knee cartilage............. 150 Colostomy....................................... 300 Total knee replacement................. 500 ERCP .............................................. 300 Total hip replacement.................... 750 Vagotomy........................................ 300 Partial colectomy ............................ 400 BRAIN Colectomy....................................... 600 Burr holes not -

Benefit of Rectal Examination in Children with Acute Abdomen
Benefit of Rectal Examination in Children with Acute Abdomen Wasun Nuntasunti MD*, Mongkol Laohapensang MD** * Department of Surgery, Sisaket Hospital, Sisaket, Thailand ** Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand Background: Acute abdomen is a condition that often mandates urgent treatment. PR or DRE (per rectal examination or digital rectal examination) is one of the fundamental physical examinations that doctors use to differentiate causes of acute abdominal pain. However, it is not a pleasant examination to undergo. Sometimes doctors ignore this examination. The benefit of per rectal examination has rarely been studied in children. Objective: This study was designed to demonstrate the benefit of rectal examination for contribution to the diagnosis of acute abdominal pain in children and reduction of unnecessary operation. Material and Method: A prospective cross sectional study of children ages 3 to 15 years old who presented with acute abdominal pain from January 2012 to December 2013 was conducted. The clinical parameters including DRE results were correlated to the diagnosis. The diagnoses prior to and after DRE were compared. The accuracy of DRE was analyzed by pair response analysis of pre and post-DRE results using McNemar‘s Chi-square test. Results: A total of 116 children with acute abdominal pain were enrolled in the study. The final diagnoses were appendicitis accounting for 27%, constipation 28%, non-surgical gastrointestinal diseases such as gastritis, diarrhea and food poisoning 9%, diseases of the female reproductive system 7% and others 29%. In comparing the diagnoses prior to and after digital rectal examination, it was demonstrated that rectal examination significantly helped differentiate diagnosis in 38.8% of patients, whereas 19% of the patients gained no benefit.DRE corrected the diagnosis in 45 cases which was significantly higher than misguiding the diagnosis in 3 cases. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Guidance for Image-Guided Procedures and Diagnostic Imaging Under Anesthesia During the COVID-19 Pandemic
Guidance for Image-Guided Procedures and Diagnostic Imaging under Anesthesia During the COVID-19 Pandemic Approved: 4/24/20 Revision: 5/7/20 – revised timing of COVID-19 testing for inpatients , Tables 1-4 Last Revision: 8/9/20 – revised timing of COVID-19 testing for asymptomatic pediatric patients, updated permissive use of N95s/PAPRs for aerosol-generating procedures in patients with negative tests, addition of COVID-19 (exposed) flag to guidance Background: This document provides guidance for the management of patients and facilities during image-guided interventions and diagnostic imaging performed under anesthesia in the Department of Radiology and Biomedical Imaging. This document represents an update to prior guidance published 5/7/20 and maintains alignment with anesthesia and perioperative practice at UCSF and national standards. Several important concepts underpin these guidelines. These include: 1) asymptomatic patients may be sources of SARS-CoV-2 disease transmission, 2) disease transmission may occur by aerosol inhalation in addition to droplet spread, 3) certain surgeries and procedures carry higher risk than others for disease transmission to healthcare workers due to aerosolization of virus, and 4) intubation, extubation, and certain forms of respiratory support are aerosol-generating. General information to be familiar with and new updates include: • COVID-19 PCR test results: Based on current estimates of COVID-19 prevalence among asymptomatic patients in San Francisco and surrounding areas and the performance of the UCSF RT-PCR test, the likelihood is very high that a patient with a negative test result does not have COVID-19 infection (~99.7% negative predictive value) (see Appendix A). -

Interventional Radiology
Patient Safety Framework for Mitigating Risk in Interventional Radiology RECOMMENDATIONS OF THE INTERVENTIONAL RADIOLOGY TASK FORCE Created: 2017 TABLE OF CONTENTS Executive Summary ........................................................................... 1 Introduction ..................................................................................... 3 Definitions .......................................................................................4 1. Introduction of New/Rare Procedures/Technologies ........................ 5 2. Pre-assessment & Clinical Decision-making ................................. 6 3. Staffing ....................................................................................... 9 4. Communications & Hand-Offs ................................................... 10 5. Production Issues ........................................................................12 6. Institutional & Executive Leadership Issues ..................................13 7. Emerging Issue: Hybrid Rooms .................................................... 15 Appendix: Interventional Radiology WHO Safety Checklist .................... 16 ABOUT THIS DOCUMENT The recommendations for Patient Safety Framework for Mitigating Risk in Interventional Radiology were developed under the auspices of the Academic Medical Center Patient Safety Organization (AMC PSO) Interventional Radiology Task Force. These consensus recommendations are for informational purposes only and should not be construed or relied upon as a standard of care. The AMC PSO recommends