Everyday Practice: Diabetes Mellitus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Acute Abdominal Pain in Children
Clinical Acute Abdominal Pain in Children Urgent message: This article will guide you through the differential diagnosis, management and disposition of pediatric patients present- ing with acute abdominal pain. KAYLEENE E. PAGÁN CORREA, MD, FAAP Introduction y tummy hurts.” That is a simple statement that shows a common complaint from children who seek “M 1 care in an urgent care or emergency department. But the diagnosis in such patients can be challenging for a clinician because of the diverse etiologies. Acute abdominal pain is commonly caused by self-limiting con- ditions but also may herald serious medical or surgical emergencies, such as appendicitis. Making a timely diag- nosis is important to reduce the rate of complications but it can be challenging, particularly in infants and young children. Excellent history-taking skills accompanied by a careful, thorough physical exam are key to making the diagnosis or at least making a reasonable conclusion about a patient’s care.2 This article discusses the differential diagnosis for acute abdominal pain in children and offers guidance for initial evaluation and management of pediatric patients presenting with this complaint. © Getty Images Contrary to visceral pain, somatoparietal pain is well Pathophysiology localized, intense (sharp), and associated with one side Abdominal pain localization is confounded by the or the other because the nerves associated are numerous, nature of the pain receptors involved and may be clas- myelinated and transmit to a specific dorsal root ganglia. sified as visceral, somatoparietal, or referred pain. Vis- Somatoparietal pain receptors are principally located in ceral pain is not well localized because the afferent the parietal peritoneum, muscle and skin and usually nerves have fewer endings in the gut, are not myeli- respond to stretching, tearing or inflammation. -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department -
Monographie Des Dégenérations Skirrheuses De L'estomac, Fondée
PART II. COMPREHENSIVE ANALYTICAL REVIEW OF MEDICAL LITERATURE. u Tros, tyriusve, nobis nullo discrimine agetur." Monographic des Degenerations Skirrheuses de VEstOmac, Jondee sur un grand nombre d'Observations recueillies tant a la Clinique de VEcole de Medecine de Paris, qvHa / Hopilal Cochin. Par Frederic Chardel, D. M. Medecin de l'Hopital Cochin, &c. 8vo. pp. 216. A Paris. " This excellent Monograph on scirrhous Affections of the Stomach" is the production of Dr. Chardel, a disciple of the celebrated Corvisart, to whom the volume is inscribed. Chardel, on scirrhous Affections of the Stomach. 1Q? a Although publication of no very recent date, we feel persuaded that, in announcing it, we shall introduce to the acquaintance of the general practitioner a work, the contents and even title of which are little known within his sphere of reading and conversation ; and we are in- cited to the labour of its analysis by the hope of confer- ring no mean benefit upon those to whom the original is inaccessible, but who prefer the researches of the dead- house to the abstract and commonly futile speculations of the closet, and regard a correct knowledge of the anato- mical character and varieties of a disease quite as essen- tial to sound nosological arrangement and successful prac- tice, as vigilant observation of the external phaenomena which it presents. To such, then, our analytical sketch is dedicated: and may the ardour displayed by the en- lightened foreigner in the prosecution of his pathological inquiries, exert a benignant influence upon those for whom we write, and arouse them to emulate his example. -

Non-Traumatic Abdominal Emergency Imaging Hepatobiliary Emergency
บทความวชาการิ Non-Traumatic Abdominal Emergency Imaging Hepatobiliary Emergency จฬาลุ กษณั ์ พรหมศร ภาควิชารังสีวิทยา คณะแพทยศาสตร์ มหาวิทยาลัยขอนแก่น Non Traumatic Abdominal Emergency Imaging invasive amebiasis Hepatobiliary Emergency o Antibody to Entamoeba rising - Liver abscess o trophosoites ascend via portal vein then - Cholangitis invaded parenchyma - Acute cholecystitis o chocolate-colored, pasty material (anchovy - Gall stone ileus paste) - Mirizzi syndrome o single/multipe Periperheral near capsule Pancreatitis - Fungal liver abscess Appendicitis o Pts hematologic malignancy or compromised Small bowel obstruction o Microabcess involving liver, spleen and Peptic Ulcer perforation kidneys Mid gut volvulous o Leukemia/ most common Candia albicans Sigmoid volvulous o Other; Cryptococcus, histoplasmosis, Mesenteric vascular ischemia mucormycosis, Aspergillus Diverticulitis o Size 2-20 mm Imaging tools Acute abdomen series Imaging; Chest upright - Plain film; hepatomegaly, intrahepatic gas/an Abdomen upright fluid level Abdomen supine - US: Left lateral decubitus o variable in shape and echo (hypoechoic, Ultrasound hyperechoic, anechoic) with septation, fluid level CT without and with posterior enhancement MRI o Amebic; round/oval hypoechoic mass abuts liver capsule Liver abscess o Fungal; multiple tiny small echoic lesions - Pyogenic liver abscess scattered through liver parenchyma o(K pneumonia, E coli, Enterococcus, o US, CT 4 patterns of hepatosplenic Burkholderia, Streptococcus, and Staphylococcus spe- candidiasis cies) 1. wheel-within-a wheel; central hypoechic of o Solitary necrosis containing fungal, surrounded echogenic o Multiple inflammatory cells o Few mm- cm 2. Bull’s-eye of central echogenic nidus surrounded - Amebic liver abscess by hypoechoic rim( pts active fungal infection with nor- o Amebic liver abscess; E.Histolytica mal white cell) o most common extraintestinal from of 3. -

The Survey Film in Acute Abdominal Disorders
Gratitude is expressed to Dr. Price E. Thomas, determine some of factors controlling rate of action of curare. J. Physiol. 106:20P, 1947. Department of Physiology, Kirksville College of 10. Kalow, W.: Hydrolysis of local anesthetics by human serum Osteopathy and Surgery, for his guidance in the cholinesterase. J. Pharmacol. Exper. Therap. 104:122-134, Feb. 1952. writing of this paper, and to Mrs. Kathryn Balder- 11. Beecher, H. K., and Murphy, A. J.: Acidosis during thoracic son for preparation of the diagrams. surgery. J. Thoracic Surg. 19:50-70, Jan. 1950. 12. Lehmann, H., and Silk, E.: Succinylrnonocholine. Brit. M. J. 1:767-768, April 4, 1953. 13. Frumin, J. M.: Hepatic inactivation of succinylcholine in dog. Fed. Proc. 17:368, 1958. 1. Boba, A., et al.: Effects of apnea, endotracheal suction, and 14. Barnes, J. M., and Davies, D. R.: Blood cholinesterase levels oxygen insufflation, alone and in combination, upon arterial oxygen in workers exposed to organo-phosphorous insecticides. Brit. M. J. saturation in anesthetized patients. J. Lab. Clin. Med. 53:680-685, 2:816-819, Oct. 6, 1951. May 1959. 15. Lehmann, H., and Ryan, E.: Familial incidence of low pseudo- 2. Bard, P.: Medical physiology. Ed. 10. C. V. Mosby Co., St. cholinesterase level. Lancet 2:124, July 21, 1956. Louis, 1956. 16. Lehmann, H., and Simmons, P. H.: Sensitivity to suxame- 3. Ruch, T. C., and Fulton, J. F.: Medical physiology and bio- thonium; apnoea in two brothers. Lancet 2:981-982, Nov. 8, 1958. physics. Ed. 18. W. B. Saunders Co., Philadelphia, 1960. 17. -
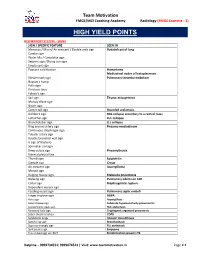
High Yield Points
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB -

Idiopathic Cervical and Retroperitoneal Fibrosis: Report of a Case Treated with Steroids PETER HUSBAND A
Postgrad Med J: first published as 10.1136/pgmj.52.614.788 on 1 December 1976. Downloaded from Postgraduate Medical Journal (December 1976) 52, 788-793. CASE REPORTS Idiopathic cervical and retroperitoneal fibrosis: report of a case treated with steroids PETER HUSBAND A. KNUDSEN M.R.C.P., D.C.H. M.D., F.R.C.P., F.R.C.Path. Departments ofPaediatrics and Histopathology, West Middlesex Hospital, Isleworth, Middlesex Summary of malignant lymphoma was made and a biopsy of Retroperitoneal fibrosis in a 12-year-old boy is the cervical mass was therefore carried out. reported. This was associated with a fibrotic mass in Histology. The biopsy consisted mainly of young the neck which resolved spontaneously. Right-sided proliferating fibroblastic tissue sparsely infiltrated ureteric obstruction responded to treatment with by lymphocytes and eosinophil leucocytes. Plasma steroids. cells and neutrophil polymorphs were absent. Small areas of fibrinoid degeneration were present in the Introduction young fibrous tissue. Blood vessels were few and the Idiopathic retroperitoneal fibrosis was first de- appearance did not resemble granulation tissue. scribed by Albarran in 1905 and the first account was There was no evidence of vasculitis. One small lymphProtected by copyright. published in the English literature by Ormond in node was present. This showed sinus cell hyperplasia 1948. Since then many cases have been described but and infiltration of the medulla by plasma cells. it is a most unusual disease in childhood. The fibrosis Follicular pattern was preserved and germinal centres in the retroperitoneal space may be associated with were prominent. There was no evidence of fibrosis in other parts of the body. -

Ultrasound Guided Percutaneous Catheter Drainage of An
International Surgery Journal Das DK et al. Int Surg J. 2019 Jun;6(6):2219-2221 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: http://dx.doi.org/10.18203/2349-2902.isj20192399 Case Report Ultrasound guided percutaneous catheter drainage of an appendicular perforation with large intraperitoneal abscess formation: an effective modality of management in selected cases Deepak Kumar Das*, Rajat Kumar Patra, Subhrajit Mishra, Sudhir Kumar Panigrahi Department of Surgery, Kalinga Institute of medical Sciences, Bhubaneswar, Odisha, India Received: 20 March 2019 Accepted: 17 May 2019 *Correspondence: Dr. Deepak Kumar Das, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Appendicular pathology is a very common entity and appendicular perforation can present in various forms ranging from right lower abdominal pain, fever and anorexia to frank peritonitis with endotoxaemic shock. We present a 18 year female with fever, anorexia and a large upper and mid abdominal swelling of 2 weeks duration which after admission was treated with intravenous fluids, antibiotics, analgesics and antiemetics. Her CECT abdomen and pelvis revealed a huge fluid containing cystic lesion with a perforated appendix tip and intraluminal faecolith and calculi. She underwent USG guided 10F pigtail catheter drainage of the walled off peritoneal collection on 3rd day of admission. About 700 ml of serous fluid with minimal flecks was drained within 2 hours and another 860 ml over next 3 days. -

Tion of Fluid, Apparently Wholly Within an Abdominal Right the Liver Dulness Was Made out at the Ninth Rib
Patient.—Mrs. A. N., aged 39, recently entered Professor Dock's clinic on account of an abdominal tumor, which had been present for more than fourteen months ; weakness, loss of PARAVERTEBRAL TRIANGLE OF DULNESS weight, abdominal pain of no distinct type and ascites ( ? ). (GROCCO'S SIGN) History.—Thirteen years ago the right ovary was removed for an enlargement of the nature of which she is ignorant. IN A CASE OF ABDOMINAL MULTILOCULAR CYSTADENOMA. Was married at 27 ; was never pregnant ; still menstruates FRANK SMITHIES, M.D. regularly. Shortly after ovarian operation, hernia developed at side of and wears a stout truss. Instructor in Internal Medicine and Demonstrator of Clinical Medi- incision, patient History cine, University of Michigan. otherwise negative. a noted in It ANN ARBOR, MICH. July, 1906, mass was left hypochondrium. grew rapidly larger, and in October, 1906, was tapped, and a In various conditions complicated with collections of amount of fluid removed. Since that time she has been in the large fluid pleural sacs, the clinical observations of tapped fourteen times. At present the abdomen is as large Grocco,1 Baduel and Siciliano,2 Rauchfuss,3 Thayer and as it ever was. Apart from the abdominal condition she has Fabyan,4 Ewart,5 Morison6 and others, have established been in fair health. the constancy of an area of percussion dulness, Examination.—A rather cachectic woman of medium build. roughly somewhat triangular in outline, lying along the on the oppo- Thorax : Anterior, short, but fairly broad ; expansion spine, but shallow; no distinct Lit- site side to that on which the fluid is found. -

Congenital Left Lobe Megaly of Liver Resembling Splenic Pathology
Splenosis. Indian Journal of Surgery. 2019 Dec 1;81(6):602- Dec 2019 Surgery. of Journal Indian Splenosis. liver. Journal of the Anatomical Society of India. 2018 Aug 1;67:S73. Aug 2018 India. of Society Anatomical the of Journal liver. 11. Solav SV, Patil AM, Savale SV. Radionuclide Liver-Spleen Scan to Detect Detect to Scan Liver-Spleen Radionuclide SV. Savale AM, Patil SV, Solav 11. 3. Joshi SS, Valimbe N, Joshi SD. Morphological variations of left lobe of of lobe left of variations Morphological SD. Joshi N, Valimbe SS, 3. Joshi patients. Journal of hepatology. 2003 Sep 1;39(3):326-32. Sep 2003 hepatology. of Journal patients. MDText. com, Inc.. com, MDText. tomography (SPECT) for assessment of hepatic function in cirrhotic cirrhotic in function hepatic of assessment for (SPECT) tomography GnRH and gonadotropin secretion. In Endotext [Internet] 2018 Jun 19. 19. Jun 2018 [Internet] Endotext In secretion. gonadotropin and GnRH Quantitative liver-spleen scan using single photon emission computerized computerized emission photon single using scan liver-spleen Quantitative 2. Marques P, Skorupskaite K, George JT, Anderson RA. Physiology of of Physiology RA. Anderson JT, George K, Skorupskaite P, 2. Marques 10. Zuckerman E, Slobodin G, Sabo E, Yeshurun D, Naschitz JE, Groshar D. D. Groshar JE, Naschitz D, Yeshurun E, Sabo G, Slobodin E, Zuckerman 10. Toronto: Elsevier Churchill Livingstone 2008p. 1207-8. 2008p. Livingstone Churchill Elsevier Toronto: Jan;19(1):3. Edinburg, London, New York, Oxford, Philadelphia, St. Louis, Sydney, Sydney, Louis, St. Philadelphia, Oxford, York, New London, Edinburg, medicine: official publication, Society of Nuclear Medicine. -

Common Surgical Concerns Dr. Metzgar
COMMON SURGICAL Martha Metzgar, DO, CONCERNS FAAFP SURGERY ON AOBFP EXAM ¡EENT – 5% - Just the first E ¡General Surgery – 3% - some ¡Orthopedics – 3% - NOPE A 45-year-old female has ultrasonography of her kidneys as part of an evaluation for uncontrolled hypertension. The report notes an incidental finding of stones in the gallbladder, confirmed on right upper quadrant ultrasonography. She has no CASE 1 symptoms you can relate to the gallstones. Other than hypertension she has no chronic medical problems. Which one of the following should you recommend to her at this time regarding the gallstones? A) Expectant management B) Oral dissolution therapy C) Extracorporeal lithotripsy D) Endoscopic retrograde cholangiopancreatography(ERCP) E) Laparoscopic cholecystectomy BILIARY CONDITIONS ¡Cholecystitis §inflammation and infection of the gallbladder caused by blockage of the cystic duct ¡Cholelithiasis – Cause Biliary colic §Transient obstruction of the cystic duct with gallstone. ¡Choledocholithiasis § stone in the common bile duct – often causes increases in LFTs ¡Cholangitis §Inflammation of the bile ducts CHOLELITHIASIS ¡ Risk factors ¡ Asymptomatic - Obesity § 10% will be symptomatic - Rapid/Cyclic weight loss in 5 years § Childbearing § 25% in 10 years § Female § Expectant management § First degree relative ¡ Oral dissolution therapy § Native American or not helpful Scandinavian descent ¡ Symptomatic – surgery § Drugs - Ceftriaxone, estrogen, TPN ¡ Imaging of choice is § Increasing age ultrasound. § Ileal disease, resection, or bypass