Three Parts of Small Intestine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
General Principles of GIT Physiology Objectives
General Principles of GIT Physiology Objectives: ❖ Physiologic Anatomy of the Gastrointestinal Wall. ❖ The General & Specific Characteristics of Smooth Muscle. ❖ Neural & Hormonal Control of Gastrointestinal Function. ❖ Types of Neurotransmitters Secreted by Enteric Neurons. ❖ Functional Types of Movements in the GIT. ❖ Gastrointestinal Blood Flow "Splanchnic Circulation". ❖ Effect of Gut Activity and Metabolic Factors on GI Blood Flow. Done by : ➔ Team leader: Rahaf AlShammari ➔ Team members: ◆ Renad AlMigren, Rinad Alghoraiby ◆ Yazeed AlKhayyal, Hesham AlShaya Colour index: ◆ Turki AlShammari, Abdullah AlZaid ● Important ◆ Dana AlKadi, Alanoud AlEssa ● Numbers ◆ Saif AlMeshari, Ahad AlGrain ● Extra َ Abduljabbar AlYamani ◆ َوأن َّل ْي َ َس ِلْ ِْلن َسا ِنَ ِإََّلَ َما َس َع ىَ Gastrointestinal System: GIT Gastrointestinal System Associated Organs (Liver,gallbladder,pancreas,salivary gland) Gastrointestinal Function: ● The alimentary tract provides the body with a continual supply of water, electrolytes, and nutrients. To achieve this function, it requires: 1 Movement of food through the alimentary tract (motility). 2 Secretion of digestive juices and digestion of the food. 3 Absorption of water, various electrolytes, and digestive products. 4 Circulation of blood through the gastrointestinal organs to carry away the absorbed substances. ● Control of all these functions is by local, nervous, and hormonal systems. The Four Processes Carried Out by the GIT: 2 Physiologic Anatomy of the Gastrointestinal Wall ● The following layers structure the GI wall from inner surface outward: ○ The mucosa ○ The submucosa ○ Circular muscle layer ○ longitudinal muscle layer Same layers in Same layers Histology lecture Histology ○ The serosa. ● In addition, sparse bundles of smooth muscle fibers, the mucosal muscle, lie in the deeper layers of the mucosa. The General Characteristics of Smooth Muscle 1- Two Smooth Muscle Classification: Unitary type ● Contracts spontaneously in response to stretch, in the Rich in gap junctions absence of neural or hormonal influence. -

Autonomic Dysfunction in Cystic Fibrosis
JOURNAL OF THE ROYAL SOCIETY OF MEDICINE Supplement No. 43 Volume 96 2003 Autonomic dysfunction in cystic fibrosis AMirakhur MB MRCP MJWalshaw MD FRCP J R Soc Med 2003;96(Suppl. 43):11–17 SECTION OF PAEDIATRICS & CHILD HEALTH, 26 NOVEMBER 2002 INTRODUCTION thetic nervous system, has both pre- and postganglionic The autonomic nervous system (ANS) is a complex neural fibres. However, in general, the preganglionic fibres pass network largely responsible for the regulation of visceral uninterrupted to the organ that is to be controlled; function and maintenance of homeostasis of the internal postganglionic neurons are located in the wall of the organ.3 environment.1 This is achieved primarily through interac- The neurotransmitter for all preganglionic and para- tions with the endocrine system and via autonomic reflexes. sympathetic postganglionic fibres is acetylcholine. All The latter comprise specialized sensory receptors in the postganglionic sympathetic nerves are adrenergic except viscera which provide information regarding visceral for those fibres innervating the sweat glands which are function to higher ANS centres in the brain. At these sites cholinergic.1 sensory information is processed and integrated, and appropriate autonomic motor responses to the viscera are Higher centres relayed through the ANS efferent system. In many The supraspinal integration of ANS function is accomplished circumstances, the ANS reflexes are capable of responding by a complex interaction of many brainstem, mesencephalic very quickly to alterations in the internal environment and and cortical areas, the hypothalamus being the principal can rapidly return the system to its homeostatic baseline. higher centre for integration of ANS function. It receives sensory afferents as well as connections from the limbic GENERAL ANATOMICAL ORGANIZATION system and sensorimotor cortex, and exerts its effects via The ANS has two major divisions: the sympathetic and interactions with the endocrine system and through 2 parasympathetic nervous systems. -

Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments
ORIGINAL ARTICLE Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments Takayoshi Kiba, MD, PhD organ at birth, reaches its adult size and morphology after Abstract: Substantial new information has accumulated on the weaning (3 weeks of age). mechanisms of secretion, the development, and regulation of the gene In pancreatic regeneration after cholecystokinin analog expression, and the role of growth factors in the differentiation, growth, and regeneration of the pancreas. Many genes that are re- cerulein-induced acute pancreatitis, 2 separate peaks of DNA quired for pancreas formation are active after birth and participate in synthesis have been reported. The first peak corresponded with endocrine and exocrine cell functions. Although the factors that nor- duct cell and mesenchymal cell proliferation, and the second mally regulate the proliferation of the pancreas largely remain elu- peak was associated with acinar cell proliferation.1 However, sive, several factors to influence the growth have been identified. It in this model, islet cells did not regenerate. Formation of new was also reported that the pancreas was sensitive to a number of apop-  cells can take place via 2 pathways: replication of already totic stimuli. The autonomic nervous system influences many of the differentiated  cells and neogenesis from putative islet stem functions of the body, including the pancreas. In fact, the parasympa- cells. It is generally admitted that neogenesis mostly takes thetic nervous system and the sympathetic nervous system have op- place during fetal and neonatal life. In adulthood, little increase posing effects on insulin secretion from islet  cells; feeding-induced in the -cell number seems to occur. -

Current Strategies in the Management of Irritable Bowel Syndrome
icine- O ed pe M n l A a c n c r e e s t s n I Internal Medicine: Open Access Randall et al., Intern Med 2014, S1:006 DOI: 10.4172/2165-8048.S1-006 ISSN: 2165-8048 Review Article Open Access Current Strategies in the Management of Irritable Bowel Syndrome Randall CW1,2*, Saurez AV3 and Zaga-Galante J3 1Clinical Professor of Medicine, University of Texas Health Science Ctr, San Antonio, USA 2CEO, Gastroenterology Research of America, USA 3Anahuac University, Mexico City, Mexico *Corresponding author: Charles W Randall, Clinical Professor of Medicine, University of Texas Health Science Ctr, San Antonio, USA and CEO, Gastroenterology Research of America, USA, Tel: (210) 410 2515; E-mail: [email protected] Rec date: Jan 17, 2014, Acc date: Feb 28, 2014, Pub date: Mar 09, 2014 Copyright: ©2014 Randall CW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Irritable bowel syndrome (IBS) is one of the most studied and discussed problems in the field of gastroenterology, yet it often remains perplexing to both clinicians and patients. Some of the apprehension comes from a void of objective data that defines a diagnosis in most disorders. This level of comfort is not appreciated in the evaluation of IBS, where the art of medicine and subjective impressions are the cornerstones of proper assessment. Though this paper focuses on management, a review of pathophysiology and specific guidelines establishing a diagnosis of IBS will be addressed. -

Physiology of the Pancreas
LECTURE IV: Physiology of the Pancreas EDITING FILE IMPORTANT MALE SLIDES EXTRA FEMALE SLIDES LECTURER’S NOTES 1 PHYSIOLOGY OF THE PANCREAS Lecture Four OBJECTIVES ● Functional Anatomy ● Major components of pancreatic juice and their physiologic roles ● Cellular mechanisms of bicarbonate secretion ● Cellular mechanisms of enzyme secretion ● Activation of pancreatic enzymes ● Hormonal & neural regulation of pancreatic secretion ● Potentiation of the secretory response Pancreas Lying parallel to and beneath the stomach, it is a large compound gland with most of its internal structure similar to that of the salivary glands. It is composed of: Figure 4-1 Endocrine portion 1-2% Exocrine portion 95% (Made of Islets of Langerhans) (Acinar gland tissues) Secrete hormones into the blood Made of acinar & ductal cells.1 - ● Insulin (beta cells; 60%) secretes digestive enzymes, HCO3 ● Glucagon (alpha cells; 25%) and water into the duodenum . ● Somatostatin (delta cells; 10%). Figure 4-2 Figure 4-3 ● The pancreatic digestive enzymes are secreted by pancreatic acini. ● Large volumes of sodium bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. ● Pancreatic juice is secreted in response to the presence of chyme in the upper portions of the small intestine. ● Insulin and Glucagon are crucial for normal regulation of glucose, lipid, and protein metabolism. FOOTNOTES 1. Acinar cells arrange themselves like clusters of grapes, that eventually release their secretions into ducts. Collection of acinar cells is called acinus, acinus and duct constitute one exocrine gland. 2 PHYSIOLOGY OF THE PANCREAS Lecture Four Pancreatic Secretion: ● Amount ≈ 1.5 L/day in an adult human. ● The major functions of pancreatic secretion: To neutralize the acids in the duodenal chyme to optimum range 1 (pH=7.0-8.0) for activity of pancreatic enzymes. -

Gastrointestinal Motility Physiology
GASTROINTESTINAL MOTILITY PHYSIOLOGY JAYA PUNATI, MD DIRECTOR, PEDIATRIC GASTROINTESTINAL, NEUROMUSCULAR AND MOTILITY DISORDERS PROGRAM DIVISION OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION, CHILDREN’S HOSPITAL LOS ANGELES VRINDA BHARDWAJ, MD DIVISION OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION CHILDREN’S HOSPITAL LOS ANGELES EDITED BY: CHRISTINE WAASDORP HURTADO, MD REVIEWED BY: JOSEPH CROFFIE, MD, MPH NASPGHAN PHYSIOLOGY EDUCATION SERIES SERIES EDITORS: CHRISTINE WAASDORP HURTADO, MD, MSCS, FAAP [email protected] DANIEL KAMIN, MD [email protected] CASE STUDY 1 • 14 year old female • With no significant past medical history • Presents with persistent vomiting and 20 lbs weight loss x 3 months • Initially emesis was intermittent, occurred before bedtime or soon there after, 2-3 hrs after a meal • Now occurring immediately or up to 30 minutes after a meal • Emesis consists of undigested food and is nonbloody and nonbilious • Associated with heartburn and chest discomfort 3 CASE STUDY 1 • Initial screening blood work was unremarkable • A trial of acid blockade was started with improvement in heartburn only • Antiemetic therapy with ondansetron showed no improvement • Upper endoscopy on acid blockade was normal 4 CASE STUDY 1 Differential for functional/motility disorders: • Esophageal disorders: – Achalasia – Gastroesophageal Reflux – Other esophageal dysmotility disorders • Gastric disorders: – Gastroparesis – Rumination syndrome – Gastric outlet obstruction : pyloric stricture, pyloric stenosis • -

Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Enteric Nervous System (ENS): 1) Myenteric (Auerbach) plexus & 2) Submucosal (Meissner’s) plexus à both triggered by sensory neurons with chemo- and mechanoreceptors in the mucosal epithelium; effector motors neurons of the myenteric plexus control contraction/motility of the GI tract, and effector motor neurons of the submucosal plexus control secretion of GI mucosa & organs. Although ENS neurons can function independently, they are subject to regulation by ANS. Autonomic Nervous System (ANS): 1) parasympathetic (rest & digest) – can innervate the GI tract and form connections with ENS neurons that promote motility and secretion, enhancing/speeding up the process of digestion 2) sympathetic (fight or flight) – can innervate the GI tract and inhibit motility & secretion by inhibiting neurons of the ENS Sections and dimensions of the GI tract (alimentary canal): Esophagus à ~ 10 inches Stomach à ~ 12 inches and holds ~ 1-2 L (full) up to ~ 3-4 L (distended) Duodenum à first 10 inches of the small intestine Jejunum à next 3 feet of small intestine (when smooth muscle tone is lost upon death, extends to 8 feet) Ileum à final 6 feet of small intestine (when smooth muscle tone is lost upon death, extends to 12 feet) Large intestine à 5 feet General Histology of the GI Tract: 4 layers – Mucosa, Submucosa, Muscularis Externa, and Serosa Mucosa à epithelium, lamina propria (areolar connective tissue), & muscularis mucosae Submucosa à areolar connective tissue Muscularis externa à skeletal muscle (in select parts of the tract); smooth muscle (at least 2 layers – inner layer of circular muscle and outer layer of longitudinal muscle; stomach has a third layer of oblique muscle under the circular layer) Serosa à superficial layer made of areolar connective tissue and simple squamous epithelium (a.k.a. -

Gastrointestinal Motility
Gastrointestinal Motility H. J. Ehrlein and M.Schemann 1. Motility of the stomach Anatomic regions of the stomach are the fundus, corpus (body), antrum and pylorus. The functional regions of the stomach do not correspond to the anatomic regions. Functionally, the stomach can be divided into the gastric reservoir and the gastric pump (Fig. 1). The gastric reservoir consists of the fundus and corpus. The gastric pump is represented by the area at which peristaltic waves occur: it includes the distal part of the corpus and the antrum. Due to different properties of the smooth muscle cells the gastric reservoir is characterised by tonic activity and the gastric pump by phasic activity. AB Gastric reservoir Fundus tonic contractions Pylorus Corpus Antrum Gastric pump phasic contractions Figure 1 . The stomach can be divided into three anatomic (A) and two functional regions (B) 1.1 Function of the gastric reservoir At the beginning of the 20 th century it was already observed that with increasing volume of the stomach the internal pressure of the stomach increases only slightly. In dogs, for instance, the increase in pressure is only 1.2 cm of water/100 ml volume. The small increase in gastric pressure indicates that the stomach does not behave like an elastic balloon but that it relaxes as it fills. Three kinds of gastric relaxation can be differentiated: a receptive, an adaptive and a feedback-relaxation of the gastric reservoir. The receptive relaxation consists of a brief relaxation during chewing and swallowing. The stimulation of mechano-receptors in the mouth and pharynx induces vago-vagal reflexes which cause a relaxation of the gastric reservoir (Fig. -
Digestive System
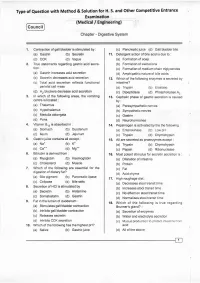
Type of Question with Method & Solution for H. S. and Other Competitive Entrance Examination (Medical / Engineering) Cou ncil Chapter - Digestive System '1. Contraction of gall bladder is stimulated by : (c) Pancreatic,uice (d) Gall bladder bile (a) Gastrin (b) Secretin 1r. Detergent action of bile acid is due to : (c) CCK (d) Vagus (a) Formation of soap 2. True statemenls regarding gastric acid secre- (b) Formation of zwitterions . tion: (c) Formation of medium chain triglycerides (a) Gastrin increases acid secretion (d) Amphipathic nature of bile acids (b) Secretin decreases acid secretion 12. Which of the following enzymes is secreted by (c) Total acid secretion reflects functional intestine? parietal cell mass (a) Trypsin (b) Elaslase (d). H2 blockers decrease acid secretion . (c) Dipeptidase (d) Phospholipase 42 3. ln which of the following areas, the vomiting 13. Cephalic phase of gastric secretion is caused centre is located : by: (a) Thalamus . (a) Parasympathetic nerves (b) Hypothalamus (b) Sympathetic nerves (c) Medulla oblongata (c) Gastrin (d) Pons (d) Neurohormones in : 4, Vitamin 8,, is absorbed '14. Pepsinogen is activated by lhe the following : (a) Stomach (b) Duodenum (a) Enterokinase (b) Low pH (c) lleum (d) Jejunum (c) Trypsin (d) Chymotrypsin 5. Gastricjuice contains all except : 15. All are secreted as proenzymes except : (a) Na" (b) K- (a) Trypsin (b) Chymotrypsin (c) Ca". (d) Ms.* (c) Pepsin (d) Ribonuclease Bilirubin is derived from : 6. 16. Most potent stimulus for secretin secretion is : . (a) Myoglobin (b) Haemoglobin (a) Dilatation of intestine (c) Cholesterol (d) Muscle (b) Protein 7. Which of the following are essential for the (c) Fat digestion of dietary fat? (d) Acid chyme (a) Bile plgment (b) Pancreatlc lipase 17. -

Digestive System Physiology of the Pancreas
Digestive System Physiology of the pancreas Dr. Hana Alzamil Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin What are the types of glands? Anatomy of pancreas Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Histology of the Pancreas Acini ◦ Exocrine ◦ 99% of gland Islets of Langerhans ◦ Endocrine ◦ 1% of gland Secretory function of pancreas Acinar and ductal cells in the exocrine pancreas form a close functional unit. Pancreatic acini secrete the pancreatic digestive enzymes. The ductal cells secrete large volumes of sodium bicarbonate solution The combined product of enzymes and sodium bicarbonate solution then flows through a long pancreatic duct Pancreatic duct joins the common hepatic duct to form hepatopancreatic ampulla The ampulla empties its content through papilla of vater which is surrounded by sphincter of oddi Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Composition of Pancreatic Juice Contains ◦ Water ◦ Sodium bicarbonate ◦ Digestive enzymes Pancreatic amylase pancreatic lipase Pancreatic nucleases Pancreatic proteases Functions of pancreatic secretion Fluid (pH from 7.6 to 9.0) ◦ acts as a vehicle to carry inactive proteolytic enzymes to the duodenal lumen ◦ Neutralizes acidic gastric secretion Enzymes ◦ -

Behaviour of Digestive Enzymes in the Pancreatic Juice and Pancreas of Rats Fed on a Low-Protein Diet (3 P
Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. Kheroua, J. Belleville To cite this version: O. Kheroua, J. Belleville. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein). Reproduction Nutrition Développement, 1981, 21 (6A), pp.901-917. hal-00897907 HAL Id: hal-00897907 https://hal.archives-ouvertes.fr/hal-00897907 Submitted on 1 Jan 1981 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. KHEROUA, J. BELLEVILLE Laboratoire de Physiologie de la Nutrition Université d’Oran, Algérie. * Laboratoire de Physiologie de la Nutrition UER Nutrition, BP 138, 21100 Dijon Cedex, France. Summary. The aim of this study in the rat was to determine the effect of a low-protein diet (3 p. -

Effect of Acid Infusion Into Various Levels of the Intestine on Gastric and Pancreatic Secretion in the Cat
Gut: first published as 10.1136/gut.10.9.749 on 1 September 1969. Downloaded from Gut, 1969, 10, 749-753 Effect of acid infusion into various levels of the intestine on gastric and pancreatic secretion in the cat S. J. KONTUREK, J. DUBIEL, AND B. GABRY9 From the Department ofMedicine, Medical School, Krakow, Poland SUMMARY Intraduodenal infusion of increasing amounts of hydrochloric acid solution results in a stepwise increase in the volume of pancreatic secretion and output of bicarbonate, reaching about 90 % of amounts attained with exogenous secretin infused intravenously in increasing doses. Acid infusion into the different regions of the intestine stimulates pancreatic secretion only from the duodenum and upper jejunum, suggesting that the area ofendogenous release of secretin by acid is confined to the upper part ofthe small bowel in the cat. Gastric acid secretion induced by pentagastrin, but not by histamine, is inhibited by acid perfusion of the duodenum. The acidification of other parts of the small intestine does not result in any change in gastric acid secretion induced either by pentagastrin or by histamine. Previous studies have shown that acidification of the ligament of Treitz, and the third in the ileum about 25 cm duodenum in the cat inhibits gastric acid secretion proximal to the caecum. and stimulates pancreatic secretion, due to the endogenous release of secretin (Konturek, Dubiel, SECRETORY PROCEDURE The secretory tests were started and and about two weeks after the cats hadrecoveredfrom surgery. Gabryg, 1969; Konturek, Gabrys, Dubiel, http://gut.bmj.com/ 1969). No study, however, has compared the relative effects on gastric and pancreatic secretion of acid infusions into various regions of the small intestine.