Hereditary and Congenital Diseases of the Kidney Classification
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines on Paediatric Urology S
Guidelines on Paediatric Urology S. Tekgül (Chair), H.S. Dogan, E. Erdem (Guidelines Associate), P. Hoebeke, R. Ko˘cvara, J.M. Nijman (Vice-chair), C. Radmayr, M.S. Silay (Guidelines Associate), R. Stein, S. Undre (Guidelines Associate) European Society for Paediatric Urology © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 7 1.1 Aim 7 1.2 Publication history 7 2. METHODS 8 3. THE GUIDELINE 8 3A PHIMOSIS 8 3A.1 Epidemiology, aetiology and pathophysiology 8 3A.2 Classification systems 8 3A.3 Diagnostic evaluation 8 3A.4 Disease management 8 3A.5 Follow-up 9 3A.6 Conclusions and recommendations on phimosis 9 3B CRYPTORCHIDISM 9 3B.1 Epidemiology, aetiology and pathophysiology 9 3B.2 Classification systems 9 3B.3 Diagnostic evaluation 10 3B.4 Disease management 10 3B.4.1 Medical therapy 10 3B.4.2 Surgery 10 3B.5 Follow-up 11 3B.6 Recommendations for cryptorchidism 11 3C HYDROCELE 12 3C.1 Epidemiology, aetiology and pathophysiology 12 3C.2 Diagnostic evaluation 12 3C.3 Disease management 12 3C.4 Recommendations for the management of hydrocele 12 3D ACUTE SCROTUM IN CHILDREN 13 3D.1 Epidemiology, aetiology and pathophysiology 13 3D.2 Diagnostic evaluation 13 3D.3 Disease management 14 3D.3.1 Epididymitis 14 3D.3.2 Testicular torsion 14 3D.3.3 Surgical treatment 14 3D.4 Follow-up 14 3D.4.1 Fertility 14 3D.4.2 Subfertility 14 3D.4.3 Androgen levels 15 3D.4.4 Testicular cancer 15 3D.5 Recommendations for the treatment of acute scrotum in children 15 3E HYPOSPADIAS 15 3E.1 Epidemiology, aetiology and pathophysiology -

Renal Agenesis, Renal Tubular Dysgenesis, and Polycystic Renal Diseases
Developmental & Structural Anomalies of the Genitourinary Tract DR. Alao MA Bowen University Teach Hosp Ogbomoso Picture test Introduction • Congenital Anomalies of the Kidney & Urinary Tract (CAKUT) Objectives • To review the embryogenesis of UGS and dysmorphogenesis of CAKUT • To describe the common CAKUT in children • To emphasize the role of imaging in the diagnosis of CAKUT Introduction •CAKUT refers to gross structural anomalies of the kidneys and or urinary tract present at birth. •Malformation of the renal parenchyma resulting in failure of normal nephron development as seen in renal dysplasia, renal agenesis, renal tubular dysgenesis, and polycystic renal diseases. Introduction •Abnormalities of embryonic migration of the kidneys as seen in renal ectopy (eg, pelvic kidney) and fusion anomalies, such as horseshoe kidney. •Abnormalities of the developing urinary collecting system as seen in duplicate collecting systems, posterior urethral valves, and ureteropelvic junction obstruction. Introduction •Prevalence is about 3-6 per 1000 births •CAKUT is one of the commonest anomalies found in human. •It constitute approximately 20 to 30 percent of all anomalies identified in the prenatal period •The presence of CAKUT in a child raises the chances of finding congenital anomalies of other organ-systems Why the interest in CAKUT? •Worldwide, CAKUT plays a causative role in 30 to 50 percent of cases of end-stage renal disease (ESRD), •The presence of CAKUT, especially ones affecting the bladder and lower tract adversely affects outcome of kidney graft after transplantation Why the interest in CAKUT? •They significantly predispose the children to UTI and urinary calculi •They may be the underlying basis for urinary incontinence Genes & Environment Interact to cause CAKUT? • Tens of different genes with role in nephrogenesis have been identified. -

Ultrasound Appearance of Congenital Renal Disease: Pictorial Review
The Egyptian Journal of Radiology and Nuclear Medicine (2014) 45, 1255–1264 Egyptian Society of Radiology and Nuclear Medicine The Egyptian Journal of Radiology and Nuclear Medicine www.elsevier.com/locate/ejrnm www.sciencedirect.com REVIEW Ultrasound appearance of congenital renal disease: Pictorial review Narrotam A. Patel, Pokhraj P. Suthar * Department of Radiology, S.S.G. Hospital, Medical College, Vadodara, India Received 12 April 2014; accepted 27 June 2014 Available online 5 August 2014 KEYWORDS Abstract Congenital renal diseases consist of a variety of entities. The age of presentation and GUT; clinical examination narrow down the differential diagnosis; however, imaging is essential for accu- Renal disease; rate diagnosis and pretreatment planning. Ultrasound is often used for initial evaluation. Computed Congenital; tomography (CT) and MRI provide additional information. Ultrasonography continues to occupy Ultrasonography a central role in the evaluation and detection of congenital renal diseases due to its advantage of rapid scanning time, lack of radiation exposure, cost effective and easy feasibility. Ó 2014 The Egyptian Society of Radiology and Nuclear Medicine. Production and hosting by Elsevier B.V. All rights reserved. Contents 1. Technique. 1256 1.1. Anomalies related to ascent of kidney. 1256 1.1.1. Ectopia . 1256 1.1.2. Crossed renal ectopia . 1256 1.1.3. Horseshoe kidney. 1257 1.2. Anomalies related to the ureteric bud . 1258 1.2.1. Renal agenesis . 1258 1.2.2. Supernumerary kidney . 1258 1.2.3. Duplex collecting system and ureterocele . 1258 1.2.4. Uretero-pelvic junction obstruction . 1259 1.2.5. Congenital megacalyces . 1260 1.2.6. Congenital megaureter . -
Diagnosis and Management in Most Frequent Congenital Defects Of
Prof. dr hab. Anna Wasilewska ~ 10% born with potentially significant malformation of urinary tract, but congenital renal disease much less common 1. Anomalies of the number a. Renal agenesis b. Supernumerary kidney 2. Anomalies of the size a. Renal hypoplasia 3. Anomalies of kidney structure a. Polcystic kidney b. Medullary sponge kidney 4. Anomalies of position • Ectopic pelvic kidney • Ectopic thoracic kidney • Crossed ectopic kidney with and without fusion 5. Anomalies of fusion • Horseshoe kidney • Crossed ectopic kidney with fusion 6. Anomalies of the renal collecting system a. Calcyeal diverticulum b. Ureterpelvic junction stenosis 7. Anomalies of the renal vasculature a. Arteriovenous malformations and fistulae b. Aberrant and accessory vessels. c. Renal artery stenosis The distinction between severe unilateral hydronephrosis and a multicystic dysplastic kidney may be unclear bilaterally enlarged echogenic kidneys, associated with hepatobiliary dilatation and oligohydroamnios suggests autosomal recessive polycystic kidney disease. Simple cysts Autosomal Dominant Polycystic Kidney Disease Autosomal Recessive Polycystic Kidney Disease Multicystic Dysplastic Kidney Disease cysts may be › solitary or multiple › unilateral or bilateral › congenital (hereditary or not) or acquired common increasing incidence with age single or multiple few mms to several cms smooth lining, clear fluid no effect on renal function occasionally haemorrhage, causing pain only real issue is distinction from tumour Characterized by cystic -
Congenital Anomalies 899 Which Tend to Decrease in Caliber After Excision of the Aperistaltic Distal Segment
I. UPPER URINARY TRACT A. Abnormalities of the Kidney Position and Number 1. Simple ectopia a) Incidence is approximately 1 per 900 (autopsy) (pelvic, 1 per 3000; solitary, 1 per 22,000; bilateral, 10%). Left side favored. b) Associated findings include small size with persistent fetal lobations, anterior or horizontal pelvis, anomalous vasculature, contralateral agenesis, vesicoureteral reflux, Mu¨llerian anomalies in 20–60% of females; undescended testes, hypospadias, urethral duplication in 10– 20% males; skeletal and cardiac anomalies in 20%. c) Only workup, ultrasound, voiding cystourethrography. 2. Thoracic ectopia a) Comprises less than 5% of ectopic kidneys. b) Origin is delayed closure of diaphragmatic angle versus ‘‘overshoot’’ of renal ascent. c) Adrenal may or may not be thoracic. 3. Crossed ectopia and fusion a) Incidence is 1 per 1000 to 1 per 2000; 90% crossed with fusion; 2:1 male, 3:1 left crossed; 24 cases solitary, five cases bilateral reported to date. b) Origin from abnormal migration of ureteral bud or rotation of caudal end of fetus at time of bud formation c) Associated findings include multiple or anomalous vessels arising from the ipsilateral side of the aorta and vesicoureteral reflux; with solitary crossed kidney only; genital, skeletal, and hindgut anomalies . 4. Horseshoe kidney c) Associated findings include anomalous vessels; isthmus between or behind great vessels hindered by the inferior mesenteric artery; skeletal, cardiovascular, and central nervous system (CNS) anomalies (33%); hypospadias and cryptorchidism (4%), bicornuate uterus (7%), urinary tract infection (UTI) (13%); duplex ureters (10%), stones (17%); 20% of trisomy 18 and 60% of Turner’s patients have horseshoe kidney. -

Irish Rare Kidney Disease Network (IRKDN)
Irish Rare kidney Disease Network (IRKDN) Others Cork University Mater, Waterford University Dr Liam Plant Hospital Galway Dr Abernathy University Hospital Renal imaging Dr M Morrin Prof Griffin Temple St and Crumlin Beaumont Hospital CHILDRENS Hospital Tallaght St Vincents Dr Atiff Awann Rare Kidney Disease Clinic Hospital University Hospital Prof Peter Conlon Dr Lavin Prof Dr Holian Little Renal pathology Lab Limerick University Dr Dorman and Hospital Dr Doyle Dr Casserly Patient Renal Council Genetics St James Laboratory Hospital RCSI Dr Griffin Prof Cavaller MISION Provision of care to patients with Rare Kidney Disease based on best available medical evidence through collaboration within Ireland and Europe Making available clinical trials for rare kidney disease to Irish patients where available Collaboration with other centres in Europe treating rare kidney disease Education of Irish nephrologists on rare Kidney Disease. Ensuring a seamless transition of children from children’s hospital with rare kidney disease to adult centres with sharing of knowledge of rare paediatric kidney disease with adult centres The provision of precise molecular diagnosis of patients with rare kidney disease The provision of therapeutic plan based on understanding of molecular diagnosis where available Development of rare disease specific registries within national renal It platform ( Emed) Structure Beaumont Hospital will act as National rare Kidney Disease Coordinating centre working in conjunction with a network of Renal unit across the country -
Epispadias and Exstrophy
Epispadias and Exstrophy How is bladder exstrophy/epispadias treated? Bladder exstrophy is managed surgically. One technique is to close it in stages. First the bladder and bladder neck are closed, the bones of the pelvis are brought together, and the urethra is made. Secondary surgeries are required in the first year of life to reconstruct the penis and to manage inguinal hernias. In some instances the entire reconstruction including bladder, bladder neck, pelvic bones, and urethra are closed all in one surgery. Both these techniques require an experienced surgeon. Both techniques will require the child to go to the intensive care unit (ICU) immediately after surgery for a few days. The child is then followed for a few more days in the regular (non ICU) part of the pediatric hospital before the child is ready for discharge. Hernia repairs will need to be performed later and often the child has vesicoureteral reflux, which may need to be corrected. Depending on the initial size of the bladder continence can be achieved up to 70% of the time. However, often these children require further surgeries to manage the bladder neck and treat incontinence. Often these children need to catheterize. Epispadias occurs in males and females. It occurs in bladder exstrophy and without bladder exstrophy. In males it occurs when the penis does not properly form a tube out to the tip of the penis and the opening is along the shaft of the penis. It can occur from the tip of the penis all the way to the bladder and depending on the position of the opening it can be associated with urinary incontinence (urine leakage) and retrograde ejaculation (ejaculate going backward toward the bladder instead out the urethra). -

Congenital Anomalies of Kidney and Ureter
ogy: iol Cu ys r h re P n t & R y e s Anatomy & Physiology: Current m e o a t Mittal et al., Anat Physiol 2016, 6:1 r a c n h A Research DOI: 10.4172/2161-0940.1000190 ISSN: 2161-0940 Review Article Open Access Congenital Anomalies of Kidney and Ureter Mittal MK1, Sureka B1, Mittal A2, Sinha M1, Thukral BB1 and Mehta V3* 1Department of Radiodiagnosis, Safdarjung Hospital, India 2Department of Paediatrics, Safdarjung Hospital, India 3Department of Anatomy, Safdarjung Hospital, India Abstract The kidney is a common site for congenital anomalies which may be responsible for considerable morbidity among young patients. Radiological investigations play a central role in diagnosing these anomalies with the screening ultrasonography being commonly used as a preliminary diagnostic study. Intravenous urography can be used to specifically identify an area of obstruction and to determine the presence of duplex collecting systems and a ureterocele. Computed tomography and magnetic resonance (MR) imaging are unsuitable for general screening but provide superb anatomic detail and added diagnostic specificity. A sound knowledge of the anatomical details and familiarity with these anomalies is essential for correct diagnosis and appropriate management so as to avoid the high rate of morbidity associated with these malformations. Keywords: Kidney; Ureter; Intravenous urography; Duplex a separate ureter is seen then the supernumerary kidney is located cranially in relation to the normal kidney. In such a case the ureter Introduction enters the bladder ectopically and according to the Weigert-R Meyer Congenital anomalies of the kidney and ureter are a significant cause rule the ureter may insert medially and inferiorly into the bladder [2]. -

Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017
Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017 Participating members of the Birth Defects Definitions Group: Lorenzo Botto (UT) John Carey (UT) Cynthia Cassell (CDC) Tiffany Colarusso (CDC) Janet Cragan (CDC) Marcia Feldkamp (UT) Jamie Frias (CDC) Angela Lin (MA) Cara Mai (CDC) Richard Olney (CDC) Carol Stanton (CO) Csaba Siffel (GA) Table of Contents LIST OF BIRTH DEFECTS ................................................................................................................................................. I DETAILED DESCRIPTIONS OF BIRTH DEFECTS ...................................................................................................... 1 FORMAT FOR BIRTH DEFECT DESCRIPTIONS ................................................................................................................................. 1 CENTRAL NERVOUS SYSTEM ....................................................................................................................................... 2 ANENCEPHALY ........................................................................................................................................................................ 2 ENCEPHALOCELE ..................................................................................................................................................................... 3 HOLOPROSENCEPHALY............................................................................................................................................................. -

OEIS Complex (Omphalocele, Exstrophy of Bladder, Imperforate Anus and Spine Defects)
Journal of Human Anatomy OEIS Complex (Omphalocele, Exstrophy of Bladder, Imperforate Anus and Spine Defects) Kandavadivelu M* Mini Review PSG Institute of Medical Sciences & Research, India Volume 2 Issue 1 Received Date: January 22, 2018 *Corresponding author: Manickavasuki Kandavadivelu, PSG Institute of Medical Published Date: February 16, 2018 Sciences & Research, India, Tel: 9842766782; E-mail: [email protected] Abstract OEIS complex comprises of a combination of defects including Omphalocele, Exstrophy of bladder, Imperforate anus and Spinal defects. The prenatal ultrasound of the fetus may show grossly malformed fetus. It may be provisionally diagnosed as OEIS complex by Non - visualization of urinary bladder, presence of Omphalocele, limb and spine defects in the ultrasound. During dissection of the fetus short umbilical cord and adherent amniotic membrane may be observed. On opening the sac, liver, intestines and cloaca were found to be contents. External genitalia and anal opening may not be seen. There may be an imperforate anus. Fetal spine may shows scoliosis, hemivertebrae or any other vertebral anomalies. Prognosis of the fetus depends on the associated anomalies and its severity. Serial ultrasonography may be used to accurately diagnose abdominal wall defect in utero and to diagnose the associated anomalies. The possibility of correction of the defects after birth of the fetus or termination of the fetus may be determined by the Ultrasound. Keywords: Exstrophy of bladder; Omphalocele; Scoliosis; Umbilical cord Introduction of the herniation of the abdominal contents into the proximal part of the umbilical cord. Herniation of the OEIS complex comprises of a combination of defects intestines into the cord occurs in approximately 1 in 5000 including Omphalocele, Exstrophy of bladder, Imperforate births and herniation of liver and intestines occur in 1 in anus and Spine defects. -
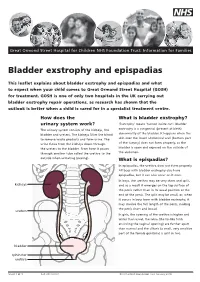
Bladder Exstrophy and Epispadias
Great Ormond Street Hospital for Children NHS Foundation Trust: Information for Families Bladder exstrophy and epispadias This leaflet explains about bladder exstrophy and epispadias and what to expect when your child comes to Great Ormond Street Hospital (GOSH) for treatment. GOSH is one of only two hospitals in the UK carrying out bladder exstrophy repair operations, as research has shown that the outlook is better when a child is cared for in a specialist treatment centre. How does the What is bladder exstrophy? urinary system work? ‘Exstrophy’ means ‘turned inside out’. Bladder The urinary system consists of the kidneys, the exstrophy is a congenital (present at birth) bladder and ureters. The kidneys filter the blood abnormality of the bladder. It happens when the to remove waste products and form urine. The skin over the lower abdominal wall (bottom part urine flows from the kidneys down through of the tummy) does not form properly, so the the ureters to the bladder. From here it passes bladder is open and exposed on the outside of through another tube called the urethra to the the abdomen. outside when urinating (peeing). What is epispadias? In epispadias, the urethra does not form properly. All boys with bladder exstrophy also have epispadias, but it can also occur on it own. In boys, the urethra may be very short and split, kidneys and as a result it emerges on the top surface of the penis rather than in its usual position at the end of the penis. The split may be small, or, when it occurs in boys born with bladder exstrophy, it may involve the full length of the penis, making the penis short and broad. -

Abdominal Wall Defects
FETAL MRI OF ABDOMINAL WALL DEFECTS Teresa Victoria MD PhD Children’s Hospital of Philadelphia PRENATAL WORK UP AWD • AWD range • very simple (umbilical cord defect) • highly complex (cloacal exstrophy or LBWC) • all: abd content herniation through ventral wall • Correct dx, vital: 1. Appropriate management and referral 2. Accurate parental counseling KEY TO DX: UMBILICAL CORD INSERTION OBJECTIVES • Fetal MR review of abdominal wall defects 1. Umbilical cord defect 2. Gastroschisis 3. Omphalocele 4. Bladder exstrophy 5. Cloacal exstrophy 6. Limb body wall complex 1. UMBILICAL CORD DEFECT Defect of the abdominal wall muscles Skin covered SSFP ssTSE UMBILICAL CORD DEFECT OB MUST KNOW! or the bowel will be cut ssTSE T1FLASH 2. GASTROSCHISIS • Full thickness abd. wall defect • Usually RIGHT-sided paraumbilical defect Survival: 95% if uncomplicated SSFP GASTROSCHISIS-COMPLICATED ssTSE T1FLASH • Survival decreases (~70%) if: ischemia perforation atresia 3. OMPHALOCELE • Herniation abd contents into base of umb cord • Usually membrane covered Peritoneum Wharton’s jelly Amnion • Etiology, uncertain • Cord insertion, at base/apex of AWD 20 wk fetus OMPHALOCELE • Herniation abd contents into base of umb cord • Usually membrane covered Peritoneum Wharton’s jelly Amnion • Etiology, uncertain • Cord insertion, at base/apex of AWD OMPHALOCELE-”TYPES” Giant omph Bowel only with ascites (>75% herniated liver) OMPHALOCELE “TYPES” Ruptured OMPHALOCELE “TYPES” L B Ruptured Syndromic Beckwith-Wiedemann 4. BLADDER EXSTROPHY • Failure of ant abd wall and ant bladder wall to close normally • AWD INFERIOR to the cord insertion site • Hallmark of BE: “Absent” urinary bladder INFRAumbilical “mass” represents the everted bladder Bladder is everted and open to the abd wall Urine is released directly to amniotic cavity • Normal amniotic fluid and hindgut • Usually abnormal genitalia BLADDER EXSTROPHY L 29 wk fetus BLADDER EXSTROPHY ♀ 29 wk fetus BLADDER EXSTROPHY 29 wk fetus ♂ 5.