PCCC Agenda and Papers July 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Handforth, Bollin Fee, Chelford, Chorley, Styal, Dean Row, Hough, Fulshaw and Morley
• ' With Alderley (Nether and Over), Handforth, Bollin Fee, Chelford, Chorley, Styal, Dean Row, Hough, Fulshaw and Morley. l~TIL"MSLOW is a town and very large parish, on the I vestry adjoining the north transept, built in I 878 at a cost f f river Bollin and the high road from Congleton to fo £700 : the south transept, or Hawthorn chapel, originally Stockport and Manchester, with a station on the Manchester 1 attached to Hawthorn Hall, but recently acquired for the and Crewe section of the London and North Western rail- parish, was erected by the Leigh family, formerly way, which crosses the vale of the Bollin by a via.duct of resident at the Hall, and their arms are displayed in the II arches ; it is 176! miles from London, I9 from windows: at an earlier period it was known as Ryle's Crewe, 7 east from Knutsford, 40 from Chester, I4± north chapel : at the west end are memorial windows to George from Sandbach, 12 south from Manchester, 6 south-west Bower, of London and Hostol, Kent, d. rs June, 1865; and from Stockport, I2 by rnil and 7 by road north-west from to Joshua Bower, surgeon, d. 7 Sept. I875, at the west end of Macclesfield, and 7 by road south-east from Altrincham, in the north aisle; and in the south aisle another, placed by the Knutsford division of the county of Cheshire, Macclesfield Edmund Ash ton esq. of Hatfield, in memory of his wife, d. hundred, Prestbury petty sessional division, Bucklow union 17 Feb. -

Appendix 4 Detailed Proposals for Each Ward – Organised by Local Area Partnership (LAP)
Appendix 4 Detailed proposals for each Ward – organised by Local Area Partnership (LAP) Proposed Wards within the Knutsford Local Area Partnership Knutsford Local Area Partnership (LAP) is situated towards the north-west of Cheshire East, and borders Wilmslow to the north-east, Macclesfield to the south-east and Congleton to the south. The M6 and M56 motorways pass through this LAP. Hourly train services link Knutsford, Plumley and Mobberley to Chester and Manchester, while in the east of this LAP hourly trains link Chelford with Crewe and Manchester. The town of Knutsford was the model for Elizabeth Gaskell's novel Cranford and scenes from the George C. Scott film Patton were filmed in the centre of Knutsford, in front of the old Town Hall. Barclays Bank employs thousands of people in IT and staff support functions at Radbroke Hall, just outside the town of Knutsford. Knutsford is home to numerous sporting teams such as Knutsford Hockey Club, Knutsford Cricket Club, Knutsford Rugby Club and Knutsford Football Club. Attractions include Tatton Park, home of the RHS Flower show, the stately homes Arley Hall, Tabley House and Peover Hall, and the Cuckooland Museum of cuckoo clocks. In detail, the proposals are: Knutsford is a historic, self-contained urban community with established extents and comprises the former County Ward of Knutsford, containing 7 polling districts. The Parish of Knutsford also mirrors the boundary of this proposal. Knutsford Town is surrounded by Green Belt which covers 58% of this proposed division. The proposed ward has excellent communications by road, motorway and rail and is bounded to the north by Tatton Park and to the east by Birkin Brook. -

Information About the Alderley Unit
If you require translation services or a copy of this document in other languages, audio tape, Braille or larger print, please speak to a member of CWP staff, e-mail [email protected] or write to: Communications, Chesh- ire and Wirral Partnership NHS Foundation Trust, Upton Lea, Countess of Chester Health Park, Liverpool Road, Chester, CH2 1BQ. Information about the Alderley Unit Information for patients, carers and families Jeśli wymagane jest tłumaczenie lub kopia niniejszego dokumentu w innych językach, na taśmie magnetofonowej, w języku Braille’a lub dużym drukiem, prosimy o skontaktowanie się z członkiem personelu CWP (Organizacja partnerska krajowego systemu zdrowia regionów Cheshire i Wirral) lub przez pocztę elektroniczną: [email protected] lub na adres: Communications, Cheshire and Wirral Partnership NHS Foundation Trust, Upton Lea, Countess of Chester Health Park, Liverpool Road, Chester, CH2 1BQ. Os oes arnoch angen gwasanaeth cyfiethu neu gopi o'r ddogfen hon mewn ieithoedd eraill, tâp sain, Braille neu brint mawr, siaradwch ag aelod o staff CWP, e-bost [email protected] neu ysgrifennwch i: Communica- tions, Cheshire and Wirral Partnership NHS Foundation Trust, Upton Lea, Countess of Chester Health Park, Liverpool Road, Chester, CH2 1BQ. For more information see www.cwp.nhs.uk. © CWP NHS FoundationTrust The information in this leaflet was valid at the date of production June 2015 and is due for review in June 2017 Leaflet code: E/MD/05-001 12 Introduction Useful contact numbers The Alderley Unit is a regional Alderley Unit 01625 862500 Low Secure Unit for people with learning disabilities who have Social Services 0300 123 5010 committed an offence or are assessed as likely to commit an Benefit Advice Line 0800 88 22 00 offence. -

CHESHIRE. FAR 753 Barber William, Astbury, Congleton Barratt .Ambrose, Brookhouse Green, Ibay!Ey :Mrs
TRADES DlliECTORY. J CHESHIRE. FAR 753 Barber William, Astbury, Congleton Barratt .Ambrose, Brookhouse green, IBay!ey :Mrs. Mary Ann, The Warren, Barber William, Applet-on, Warrington Smallwo'Jd, Stoke-·on-Trent Gawsworth, Macclesfield Barber William, Buxton stoops. BarraH Clement, Brookhouse green, Beach J. Stockton Heath, Warrington Rainow, Macolesfield Sr.aallwood, Stoke-on-Trent Bean William, Acton, Northwich Barber W. Cheadle Hulme, Stockport Barratt Daniel. Brookhouse green, Beard· Misses Catherine & Ann, Pott; Bard'sley D. Hough hill, Dukinfield Smallwood, Stoke-on-Trent • Shrigley, Macclesfield Bardsley G. Oheadle Hulme, Stockprt Bal"''att J. Bolt's grn.Betchton,Sndbch Beard J. Harrop fold, Harrop,Mcclsfld Bardsley Jas, Heat<m Moor, Stockport Barratt Jn. Lindow common, :Marley, Beard James, Upper end, LymeHand- Bardsley Ralph, Stocks, :Kettleshulme, Wilmslow, Manchester ley, Stockport Macclesfield Barratt J. Love la. Betchton,Sand'bch Beard James, Wrights, Kettleshulme, Bardsley T. Range road, Stalybrid•ge Barratt T.Love la. Betchton, Sandb~h Macclesfield Bardsley W. Cheadle Hulme, Stckpri Barrow Mrs. A. Appleton, Warrington Beard James, jun. Lowe!l" end, Lyme Barff Arthnr, Warburton, Wa"flringtn Barrow Jn.Broom gn. Marthall,Kntsfd Handley, Stockport Barker E. Ivy mnt. Spurstow,Tarprly Ball'row Jonathan, BroadJ lane, Grap- Beard J.Beacon, Compstall, Stockport Barker M~. G. Brereton, Sandbach penhall, Warrington Beard R. Black HI. G~. Tascal,Stckpr1i Barker Henry, Wardle, Nantwich Barrow J. Styal, Handforth, )I'chestr Beard Samuel, High lane, StockpGri Barker Jas. Alsager, Stoke-upon-Trnt Barton Alfred, Roundy lane, .Adling- Be<bbington E. & Son, Olucastle, Malps Barker John, Byley, :Middlewich ton, :Macclesfield Bebbington Oha.rles, Tarporley Barker John, Rushton, Tall'porley Barton C.Brown ho. -

Index of Cheshire Place-Names
INDEX OF CHESHIRE PLACE-NAMES Acton, 12 Bowdon, 14 Adlington, 7 Bradford, 12 Alcumlow, 9 Bradley, 12 Alderley, 3, 9 Bradwall, 14 Aldersey, 10 Bramhall, 14 Aldford, 1,2, 12, 21 Bredbury, 12 Alpraham, 9 Brereton, 14 Alsager, 10 Bridgemere, 14 Altrincham, 7 Bridge Traffbrd, 16 n Alvanley, 10 Brindley, 14 Alvaston, 10 Brinnington, 7 Anderton, 9 Broadbottom, 14 Antrobus, 21 Bromborough, 14 Appleton, 12 Broomhall, 14 Arden, 12 Bruera, 21 Arley, 12 Bucklow, 12 Arrowe, 3 19 Budworth, 10 Ashton, 12 Buerton, 12 Astbury, 13 Buglawton, II n Astle, 13 Bulkeley, 14 Aston, 13 Bunbury, 10, 21 Audlem, 5 Burton, 12 Austerson, 10 Burwardsley, 10 Butley, 10 By ley, 10 Bache, 11 Backford, 13 Baddiley, 10 Caldecote, 14 Baddington, 7 Caldy, 17 Baguley, 10 Calveley, 14 Balderton, 9 Capenhurst, 14 Barnshaw, 10 Garden, 14 Barnston, 10 Carrington, 7 Barnton, 7 Cattenhall, 10 Barrow, 11 Caughall, 14 Barthomley, 9 Chadkirk, 21 Bartington, 7 Cheadle, 3, 21 Barton, 12 Checkley, 10 Batherton, 9 Chelford, 10 Bebington, 7 Chester, 1, 2, 3, 6, 7, 10, 12, 16, 17, Beeston, 13 19,21 Bexton, 10 Cheveley, 10 Bickerton, 14 Chidlow, 10 Bickley, 10 Childer Thornton, 13/; Bidston, 10 Cholmondeley, 9 Birkenhead, 14, 19 Cholmondeston, 10 Blackden, 14 Chorley, 12 Blacon, 14 Chorlton, 12 Blakenhall, 14 Chowley, 10 Bollington, 9 Christleton, 3, 6 Bosden, 10 Church Hulme, 21 Bosley, 10 Church Shocklach, 16 n Bostock, 10 Churton, 12 Bough ton, 12 Claughton, 19 171 172 INDEX OF CHESHIRE PLACE-NAMES Claverton, 14 Godley, 10 Clayhanger, 14 Golborne, 14 Clifton, 12 Gore, 11 Clive, 11 Grafton, -

37 CHELFORD ROAD, MACCLESFIELD, Macclesfield 37 Chelford Road, Macclesfield, Cheshire SK10 3LQ £119,950
Macclesfield 37 CHELFORD ROAD, MACCLESFIELD, ROAD, CHELFORD 37 These particulars are believed to be accurate but they are not guaranteed and do not form a contract. Neither Jordan Fishwick nor the vendor or lessor accept any responsibility in respect of these particulars, which are not intended to be statements or representations of fact and any intending purchaser or lessee must satisfy himself by inspection or otherwise as to the correctness of each of the statements contained in these particulars. Any floorplans on this brochure are for 01625 434000 illustrative purposes only and are not necessarily to scale. [email protected] www.jordanfishwick.co.uk Offices at: Chorlton, Didsbury, Disley, Glossop, Hale, Macclesfield, Manchester, Sale, Salford, Wilmslow, Whithington. 37 Chelford Road, Macclesfield, Cheshire SK10 3LQ £119,950 The Property Locality ** NO ONWARD CHAIN ** A delightful two bedroom mid terrace property offering well presented accommodation including a modern kitchen and bathroom. Convenience also features given the close proximity of the local shops at Broken Cross, excellent schools and leisure centre as well as within a short stroll of bus services that operates the short journey into the centre of town and surround areas. In brief the accommodation comprises living room and breakfast kitchen with access to the private courtyard. To the first floor are two bedrooms and a modern bathroom. The property has recently been decorated in neutral colours and comes with new carpets. Postcode - SK10 3LQ Location, Directions, Living Room 12'2 x 11'6 (3.71m x 3.51m ), Breakfast EPC Rating - C Kitchen 10'2 x 6'10 (3.10m x 2.08m ), First Floor, Bedroom One 14'1 x 7'6 Floor Area - sq ft (4.29m x 2.29m ), Bedroom Two 12'1 x Local Authority - 6'0 (3.68m x 1.83m ), Bathroom, Outside, Private Courtyard, Tenure Council Tax - Band. -
Spatial Distribution Update Report
Design, Planning + Prepared for: Submitted by Cheshire East Council AECOM Economics Bridgewater House, Whitworth Street, Manchester, M1 6LT July 2015 Spatial Distribution Update Report Final Report United Kingdom & Ireland AECOM Spatial Distribution Support TC-i Table of contents 1 Executive Summary 1 1.1 Introduction 1 1.2 Approach 1 1.3 Key findings 2 1.4 Options for testing the spatial distribution 5 1.5 Options analysis 10 1.6 Sustainability Appraisal and Habitats Regulation Assessment 13 1.7 Habitats Regulation Assessment 13 1.8 Recommendations 13 1.9 Implications for site allocations 15 2 Introduction and scope 17 2.1 Background to the commission 17 2.2 Council’s approach to date 17 2.3 Key objectives/issues that the commission must respond to 20 2.4 Key Requirements and Outputs 23 3 Methodology 24 3.1 Approach 24 4 Alternative spatial distribution options 27 4.2 Options for testing the spatial distribution 27 4.3 Options analysis 33 5 Summary of issues identified through the Settlement Profiles 36 5.2 Principal Towns 37 5.3 Key Service Centres 38 5.4 Local Service Centres 41 5.5 Conclusions 44 6 Vision and Strategic Priorities 47 7 Consultation and the Duty to Cooperate 49 7.1 Consultation Responses 49 7.2 Duty to Cooperate 50 8 Infrastructure 53 8.2 Public transport 53 8.3 Utilities 54 8.4 Emergency Services 54 8.5 Health facilities 54 8.6 Education 55 8.7 Leisure and culture 56 8.8 Community facilities 57 9 Highways modelling 58 10 Deliverability and Viability 62 10.2 Residential Development 62 10.3 Commercial Development 64 -

Hawthorne House, Lowndes Farm, Lower Withington
Hawthorne House, Lowndes Farm, Lower Withington Hawthorne House, Lowndes Farm, Lower Withington AN EXCITING OPPORTUNITY TO ACQUIRE THE LAST REMAINING BESPOKE COUNTRY PROPERTY BEING DEVELOPED BY CRANFORD ESTATES, SET AT THE END OF A LONG PRIVATE DRIVEWAY WITH ITS OWN GROUNDS AND ADJOINING PADDOCK OF APPROXIMATELY HALF AN ACRE OR THEREABOUTS. DIRECTIONS SK11 9HT This unique development is set at the end of its From our Alderley Edge office proceed out of long private driveway with total grounds for the the village towards Wilmslow. After passing four properties of approximately 4.3 acres or over the railway bridge take the first turning thereabouts. The properties enjoy wonderful left into Ryleys Lane which becomes the open views across the surrounding countryside. Chelford Road to Chelford roundabout (approx Lower Withington is a charming rural 2 miles). At the Chelford roundabout proceed community with local public houses, wonderful straight across towards Holmes Chapel and walks and within ten to fifteen minutes' drive of after approximately 2.5 miles turn left where the centres of Alderley Edge, Wilmslow, the road bends sharply to the right into Long Knutsford and Macclesfield. These centres Shoot Road. At the end of Long Shoot Road offer an excellent range of shopping, turn left into Salters Lane and after educational and recreational facilities with a approximately 0.5 miles turn right, which is wealth of quality restaurants. The motorway signposted to Lower Withington/Swettenham. network system, Manchester International Bear right again past The Red Lion and first Airport, local and inter-city rail links are within left into Trap Street. -

Mottram St Andrew, Macclesfield for Sale Guide Price £80,000-£100,000
pri MOTTRAM ST ANDREW, MACCLESFIELD FOR SALE GUIDE PRICE £80,000-£100,000 LAND OFF WILMSLOW OLD ROAD, MOTTRAM ST ANDREW, MACCLESFIELD, CHESHIRE SK10 4QS Located near the centre of this highly sought after village this parcel of land extends to approximately 0.48 hectares (1.2 acres) and could be used for a variety of purposes (subject to planning permission). Road frontage, near to mains services. GENERAL REMARKS This parcel of amenity land was previously used by a nursery business in the village but since it has been vacated it has been left to become overgrown. It has frontage to two roads in the centre of the village and could have future development potential. The great location and road frontage are considered excellent factors when selling land parcels of this size. It is the wish of the vendors that the land is sold to a group of local residents looking to use it for community purposes however offers from other purchasers will definitely be considered. DIRECTIONS From Alderley Edge take the Chapel Road signposted Mottram and Prestbury. Continue for exactly 2 miles and take the left turn towards Wilmslow and the Village Hall. The land is situated on the right hand side before the Moss Lane turning. TOWN AND COUNTRY PLANNING The property is sold notwithstanding any description contained in these particulars subject to any Development Plan, Tree Preservation Order, Town Planning Scheme or Agreement Resolution or Agreement, or Notice which may be or may come to be in force subject to any statutory powers or bye-laws without obligation on behalf of the vendors to specify the same. -

CHESHIRE EAST LOCAL PLAN MOTTRAM St. ANDREW PARISH
CHESHIRE EAST LOCAL PLAN MOTTRAM St. ANDREW PARISH COUNCIL RESPONSE TO THE SITE ALLOCATIONS AND DEVELOPMENT POLICIES ISSUES PAPER CHAIRMAN WILLIAM PILKINGTON I.D.481351 Issue 1 The layout of the SADPD Question 1. How do you think that the SADPD should be laid out? a. Under topic-based chapters such as 'Housing', 'Employment' and 'Transport and Infrastructure', or b. Under chapter headings that reflect those in the Local Plan Strategy? Feel free to highlight the benefits and disadvantages of each approach. Response. The approach under chapter headings makes cross reference between the two documents more straight forward. Issue 2 Determining whether further specific guidance is needed in the SADPD regarding Sustainable Development Question 2. Do you agree with this approach or do you think that further guidance is required in the SADPD specifically regarding sustainable development? If you think further guidance is required, please explain what that should be. Response. We agree with the approach proposed. Issue 3 Meeting the development requirements identified for Local Service Centres and Other Settlements and Rural Areas Question 3a. What approach do you think should be taken towards the apportionment of the overall development requirement across Local Service Centres? In particular what factors or considerations should guide this distribution and how should they be applied? Response. The criteria outlined are considered appropriate. Question 3b. What approach do you think should be taken towards meeting development requirements across Other Settlements and Rural Areas? Response. Application of green belt protections, no development unless there are special circumstances. Any development must be consistent with sustainable development policies contained in the Local Plan. -

Lower Withington Parish Council Agenda
LOWER WITHINGTON PARISH COUNCIL AGENDA PARISH COUNCIL MEETING DATE: MONDAY 24TH JUNE, 2019 TIME: 7:30p.m. VENUE: LOWER WITHINGTON PARISH HALL To Members of Lower Withington Parish Council, You are hereby summoned to attend the Parish Council Meeting, as shown above, to consider and determine the following business: 1. APOLOGIES FOR ABSENCE - 2. CODE OF CONDUCT - i) To receive Register of Interests forms from Members. 3. DECLARATIONS OF INTEREST - i) To receive Declarations of Interest in any items on the agenda. 4. MINUTES - i) To approve the Minutes of the Extraordinary Parish Council meeting held 20th May, 2019 as a correct record and authorise signing by the Chairman. ii) To approve the Minutes of the Parish Council meeting held 28th May, 2019 as a correct record and authorise signing by the Chairman. iii) To approve the Minutes of the Extraordinary Parish Council meeting held 9th June, 2019 as a correct record and authorise signing by the Chairman. 5. PUBLIC FORUM FOR QUESTIONS - 6. REPORTS FROM EXTERNAL ORGANISATIONS - i) Gawsworth & Chelford Wards Policing Team - Report on matters of interest / concern within the Parish. ii) Cheshire East Ward Member Cllr. L. Smetham - Report on items of interest to the Parish Council. 7. FINANCE - i) To receive and consider the Financial Statement 2019/20 as at 24th June, 2019. (Appendix A) ii) To authorise the following payments - a) Cheque No. 000434 E. M. Maddock £202.25 Salary - June, 2019. b) Cheque No. 000435 H.M. Revenue & Customs £50.60 Employee Income Tax. c) Cheque No. 000436 Brocklehurst Contractors Ltd. £84.00 Drainage work at Dicklow Cob. -
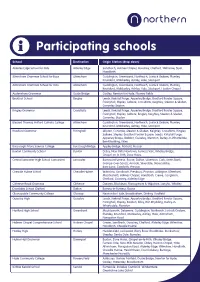
Participating Schools
Participating schools School Destination Origin Station (drop down) Alderley Edge School for Girls Alderley Edge Sandbach, Holmes Chapel, Goostrey, Chelford, Wilmslow, Styal, Handforth Altrincham Grammar School for Boys Altrincham Cuddington, Greenbank, Northwich, Lostock Gralam, Plumley, Knutsford, Mobberley, Ashley, Hale, Stockport Altrincham Grammar School for Girls Altrincham Cuddington, Greenbank, Northwich, Lostock Gralam, Plumley, Knutsford, Mobberley, Ashley, Hale, Stockport, Heaton Chapel Audenshaw Grammar Guide Bridge Godley, Newton for Hyde, Flowery Fields Beckfoot School Bingley Leeds, Kirkstall Forge, Apperley Bridge, Bradford Forster Square, Frizinghall, Shipley, Saltaire, Crossflatts, Keighley, Steeton & Silsden, Cononley Skipton Bingley Grammar Crossflatts Leeds, Kirkstall Forge, Apperley Bridge, Bradford Forster Square, Frizinghall, Shipley, Saltaire, Bingley, Keighley, Steeton & Silsden, Cononley, Skipton Blessed Thomas Holford Catholic College Altrincham Cuddington, Greenbank, Northwich, Lostock Gralam, Plumley, Knutsford, Mobberley, Ashley, Hale, Stockport Bradford Grammar Frizinghall Skipton, Cononley, Steeton & Silsden, Keighley, Crossflatts, Bingley, Saltaire, Shipley, Bradford Forster Square, Leeds, Kirkstall Forge, Apperley Bridge, Baildon, Guiseley, Menston, Burley-in-Wharfedale, Ben Rhydding, Ilkley Burscough Priory Science College Burscough Bridge Appley Bridge, Parbold, Hoscar Buxton Community School Buxton Disley, New Mills Newtown, Furness Vale, Whaley Bridge, Chapel-en-le-Frith, Dove Holes Central Lancaster