Pharmaceutical Compositions Resistant to Abuse
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ERJ-01090-2018.Supplement
Shaheen et al Online data supplement Prescribed analgesics in pregnancy and risk of childhood asthma Seif O Shaheen, Cecilia Lundholm, Bronwyn K Brew, Catarina Almqvist. 1 Shaheen et al Figure E1: Data available for analysis Footnote: Numbers refer to adjusted analyses (complete data on covariates) 2 Shaheen et al Table E1. Three classes of analgesics included in the analyses ATC codes Generic drug name Opioids N02AA59 Codeine, combinations excluding psycholeptics N02AA79 Codeine, combinations with psycholeptics N02AA08 Dihydrocodeine N02AA58 Dihydrocodeine, combinations N02AC04 Dextropropoxyphene N02AC54 Dextropropoxyphene, combinations excluding psycholeptics N02AX02 Tramadol Anti-migraine N02CA01 Dihydroergotamine N02CA02 Ergotamine N02CA04 Methysergide N02CA07 Lisuride N02CA51 Dihydroergotamine, combinations N02CA52 Ergotamine, combinations excluding psycholeptics N02CA72 Ergotamine, combinations with psycholeptics N02CC01 Sumatriptan N02CC02 Naratriptan N02CC03 Zolmitriptan N02CC04 Rizatriptan N02CC05 Almotriptan N02CC06 Eletriptan N02CC07 Frovatriptan N02CX01 Pizotifen N02CX02 Clonidine N02CX03 Iprazochrome N02CX05 Dimetotiazine N02CX06 Oxetorone N02CB01 Flumedroxone Paracetamol N02BE01 Paracetamol N02BE51 Paracetamol, combinations excluding psycholeptics N02BE71 Paracetamol, combinations with psycholeptics 3 Shaheen et al Table E2. Frequency of analgesic classes prescribed to the mother during pregnancy Opioids Anti- Paracetamol N % migraine No No No 459,690 93.2 No No Yes 9,091 1.8 Yes No No 15,405 3.1 No Yes No 2,343 0.5 Yes No -

Medicines Regulations 1984 (SR 1984/143)
Reprint as at 1 July 2014 Medicines Regulations 1984 (SR 1984/143) David Beattie, Governor-General Order in Council At the Government House at Wellington this 5th day of June 1984 Present: His Excellency the Governor-General in Council Pursuant to section 105 of the Medicines Act 1981, and, in the case of Part 3 of the regulations, to section 62 of that Act, His Excellency the Governor-General, acting on the advice of the Minister of Health tendered after consultation with the organisations and bodies that ap- peared to the Minister to be representatives of persons likely to be substantially affected, and by and with the advice and consent of the Executive Council, hereby makes the following regulations. Contents Page 1 Title and commencement 5 Note Changes authorised by subpart 2 of Part 2 of the Legislation Act 2012 have been made in this official reprint. Note 4 at the end of this reprint provides a list of the amendments incorporated. These regulations are administered by the Ministry of Health. 1 Reprinted as at Medicines Regulations 1984 1 July 2014 2 Interpretation 5 Part 1 Classification of medicines 3 Classification of medicines 11 Part 2 Standards 4 Standards for medicines, related products, medical 11 devices, cosmetics, and surgical dressings 5 Pharmacist may dilute medicine in particular case 12 6 Colouring substances [Revoked] 12 Part 3 Advertisements 7 Advertisements not to claim official approval 13 8 Advertisements for medicines 13 9 Advertisements for related products 15 10 Advertisements for medical devices 15 11 Advertisements -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Curriculum Vitae April 2013
Curriculum Vitae April 2013 NAME Michael Jeffrey Aminoff CONTACT Box 0114, Room 795-M, Dept of Neurology, 505 Parnassus Ave., San Francisco, CA 94143-0114 Tel: 415 353-1940; Fax 415 353-3289 [email protected] PLACE OF BIRTH England NATIONALITY British and US MARITAL STATUS Married, with three children CURRENT TITLE Endowed Chair in Parkinson’s Disease Research Distinguished Professor of Neurology & Executive Vice Chair, Department of Neurology, School of Medicine University of California, San Francisco Attending Physician (Neurologist) University of California Medical Center, San Francisco Director, Parkinson's Disease & Movement Disorders Clinic University of California Medical Center, San Francisco EDUCATION AND TRAINING EARLY EDUCATION Caterham School, Surrey, England MEDICAL SCHOOL University College, London, England, 1959-1962 University College Hospital, England, 1962-1965 QUALIFICATIONS 1962 B.Sc. Special (London) 1965 L.R.C.P., M.R.C.S., M.B., B.S. [Equivalent to MD degree in USA] 1968 M.R.C.P. (London) [Similar to Board Certification in Internal Medicine in USA] 1973 M.D. (London) [Advanced Research Thesis similar to Ph.D. in USA] 1976 Federal Licensing Examination and California Medical License 1977 Membership by examination, American Association of Electromyography & Electrodiagnosis, leading in 1989 to Certification by American Board of Electrodiagnostic Medicine. 1980 Certification by the American Board of Clinical Neurophysiology (ABQEEG) 1982 Certification in Neurology, American Board of Psychiatry & Neurology; recertified voluntarily, 2004 1984 F.R.C.P. (London) 1992 Subspecialty certification in Clinical Neurophysiology, American Board of Psychiatry & Neurology (new subspecialty); recertified 2002 1 2000 D.Sc. (London) [Higher doctorate in Faculty of Science, London University, London, UK] PRINCIPAL POSITIONS HELD 1965-1966 House physician & house surgeon, University College Hospital, London, U.K. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

(12) United States Patent (10) Patent No.: US 8,603,526 B2 Tygesen Et Al
USOO8603526B2 (12) United States Patent (10) Patent No.: US 8,603,526 B2 Tygesen et al. (45) Date of Patent: Dec. 10, 2013 (54) PHARMACEUTICAL COMPOSITIONS 2008. O152595 A1 6/2008 Emigh et al. RESISTANT TO ABUSE 2008. O166407 A1 7/2008 Shalaby et al. 2008/0299.199 A1 12/2008 Bar-Shalom et al. 2008/0311205 A1 12/2008 Habib et al. (75) Inventors: Peter Holm Tygesen, Smoerum (DK); 2009/0022790 A1 1/2009 Flath et al. Jan Martin Oevergaard, Frederikssund 2010/0203129 A1 8/2010 Andersen et al. (DK); Karsten Lindhardt, Haslev (DK); 2010/0204259 A1 8/2010 Tygesen et al. Louise Inoka Lyhne-versen, Gentofte 2010/0239667 A1 9/2010 Hemmingsen et al. (DK); Martin Rex Olsen, Holbaek 2010, O291205 A1 11/2010 Downie et al. (DK); Anne-Mette Haahr, Birkeroed 2011 O159100 A1 6/2011 Andersen et al. (DK); Jacob Aas Hoellund-Jensen, FOREIGN PATENT DOCUMENTS Frederikssund (DK); Pemille Kristine Hoeyrup Hemmingsen, Bagsvaerd DE 20 2006 014131 1, 2007 (DK) EP O435,726 8, 1991 EP O493513 7, 1992 EP O406315 11, 1992 (73) Assignee: Egalet Ltd., London (GB) EP 1213014 6, 2002 WO WO 89,09066 10, 1989 (*) Notice: Subject to any disclaimer, the term of this WO WO91,040 15 4f1991 patent is extended or adjusted under 35 WO WO95/22962 8, 1995 U.S.C. 154(b) by 489 days. WO WO99,51208 10, 1999 WO WOOOf 41704 T 2000 WO WO 03/024426 3, 2003 (21) Appl. No.: 12/701,429 WO WOO3,O24429 3, 2003 WO WOO3,O24430 3, 2003 (22) Filed: Feb. -
A Systematic Review of Combination and High-Dose Atypical
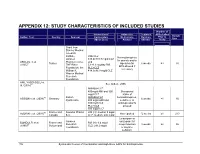
APPENDIX 12: STUDY CHARACTERISTICS OF INCLUDED STUDIES Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study Grant from Stanley Medical research Institute, RIS+CLZ Benzodiazepines Janssen 515.6±138.7 mg/d CLZ for anxiety and/or AKDEDE et al. Pharmaceutica, and 42 Turkey biperiden for 6 weeks ≥3 30 (2005) THE Ritter 5.1±1.3 mg/day RIS EPS allowed if Foundation, the PLC+CLZ necessary William K. 414.3±96.9 mg/d CLZ Warren Medical Research Foundation ANIL YAGCIOGLU et 45 See Akdede 2006 al. (2005) AMI400+CLZ 400mg/d AMI and 300 Occasional mg/d CLZ intake of 49 Sanofi- AMI600+CLZ benzodiazepines, ASSION et al. (2008) Germany 6 weeks ≥1 16 Synthelabo 600 mg/d AMI and sedatives, or 300mg/d CLZ antidepressants PLC+CLZ allowed 300 mg/d CLZ 60 France and Novartis Phama RIS (H): median 9 mg/d AZORIN et al. (2001) Not reported 12 weeks ≥1 273 Canada S.A. CLZ: median: 600 mg/d Lorazepam or Janssen oxazepam for BONDOLFI et al. France and RIS (H): 6.4 mg/d 66 Research sleep induction 8 weeks ≥2 86 (1998) Switzerland CLZ: 291.2 mg/d Foundation or daytime sedation; 156 Systematic Review of Combination and High-Dose AAPs for Schizophrenia Number of Interventions/ Adjunctive Treatment APDs Failed Sample Author, Year Country Sponsor Comparators Medications Duration Prior to Size (Mean Dose) Allowed (Weeks) Study biperiden and procyclidine for EPS Supported by grants from Brain Research center, funded by the ARI+CLZ Antidepressants, Ministry of 15.5±7.1 mg/d ARI and 38 anticholinergics CHANG et al. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

UNIVERSITE DE NANTES Thomas Gelineau
UNIVERSITE DE NANTES __________ FACULTE DE MEDECINE __________ Année 2011 N° 139 THESE pour le DIPLÔME D’ÉTAT DE DOCTEUR EN MÉDECINE DES de médecine générale par Thomas Gelineau né le 29 janvier 1983 à Cholet __________ Présentée et soutenue publiquement le 06/12/2011 __________ LE RHUME DE L'ENFANT ET SON TRAITEMENT: DECISION PARTAGEE AVEC LES PARENTS D'APRES UN QUESTIONNAIRE __________ Président : Monsieur le Professeur Olivier MALARD Directeur de thèse : Madame le Professeur Jacqueline LACAILLE 1 Table des matières IIntroduction................................................................................................................ 7 IIDéfinition, état des connaissances...........................................................................8 1Le rhume.......................................................................................................................................8 APhysiopathologie............................................................................................................................. 8 aL'origine virale.................................................................................................................................... 8 bLa saisonnalité................................................................................................................................... 8 cL'âge de survenue.............................................................................................................................. 9 dLe sexe.................................................................................................................................................. -

Partial Agreement in the Social and Public Health Field
COUNCIL OF EUROPE COMMITTEE OF MINISTERS (PARTIAL AGREEMENT IN THE SOCIAL AND PUBLIC HEALTH FIELD) RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies, and superseding Resolution AP (82) 2) AND APPENDIX I Alphabetical list of medicines adopted by the Public Health Committee (Partial Agreement) updated to 1 July 1988 APPENDIX II Pharmaco-therapeutic classification of medicines appearing in the alphabetical list in Appendix I updated to 1 July 1988 RESOLUTION AP (88) 2 ON THE CLASSIFICATION OF MEDICINES WHICH ARE OBTAINABLE ONLY ON MEDICAL PRESCRIPTION (superseding Resolution AP (82) 2) (Adopted by the Committee of Ministers on 22 September 1988 at the 419th meeting of the Ministers' Deputies) The Representatives on the Committee of Ministers of Belgium, France, the Federal Republic of Germany, Italy, Luxembourg, the Netherlands and the United Kingdom of Great Britain and Northern Ireland, these states being parties to the Partial Agreement in the social and public health field, and the Representatives of Austria, Denmark, Ireland, Spain and Switzerland, states which have participated in the public health activities carried out within the above-mentioned Partial Agreement since 1 October 1974, 2 April 1968, 23 September 1969, 21 April 1988 and 5 May 1964, respectively, Considering that the aim of the Council of Europe is to achieve greater unity between its members and that this -

(12) United States Patent (10) Patent No.: US 9,005,660 B2 Tygesen Et Al
USOO9005660B2 (12) United States Patent (10) Patent No.: US 9,005,660 B2 Tygesen et al. (45) Date of Patent: Apr. 14, 2015 (54) IMMEDIATE RELEASE COMPOSITION 4,873,080 A 10, 1989 Bricklet al. RESISTANT TO ABUSEBY INTAKE OF 4,892,742 A 1, 1990 Shah 4,898,733. A 2f1990 DePrince et al. ALCOHOL 5,019,396 A 5/1991 Ayer et al. 5,068,112 A 11/1991 Samejima et al. (75) Inventors: Peter Holm Tygesen, Smoerum (DK); 5,082,655 A 1/1992 Snipes et al. Jan Martin Oevergaard, Frederikssund 5,102,668 A 4, 1992 Eichel et al. 5,213,808 A 5/1993 Bar Shalom et al. (DK); Joakim Oestman, Lomma (SE) 5,266,331 A 11/1993 Oshlack et al. 5,281,420 A 1/1994 Kelmet al. (73) Assignee: Egalet Ltd., London (GB) 5,352.455 A 10, 1994 Robertson 5,411,745 A 5/1995 Oshlack et al. (*) Notice: Subject to any disclaimer, the term of this 5,419,917 A 5/1995 Chen et al. patent is extended or adjusted under 35 5,422,123 A 6/1995 Conte et al. U.S.C. 154(b) by 473 days. 5,460,826 A 10, 1995 Merrill et al. 5,478,577 A 12/1995 Sackler et al. 5,508,042 A 4/1996 OShlack et al. (21) Appl. No.: 12/701.248 5,520,931 A 5/1996 Persson et al. 5,529,787 A 6/1996 Merrill et al. (22) Filed: Feb. 5, 2010 5,549,912 A 8, 1996 OShlack et al. -

Chlorpromazine(BAN, Rinn)
Carpipramine Hydrochloride/Chlorpromazine 969 2. Stubb S, et al. Fixed drug eruptions: 77 cases from 1981 to 1985. Chlorpromazine Embonate (BANM, rINNM) mazine. Photosensitivity reactions are more common Br J Dermatol 1989; 120: 583. 3. Roujeau J-C, et al. Medication use and the risk of Stevens-John- Chlorpromazine, Embonate de; Chlorpromazine Pamoate; with chlorpromazine than with other antipsychotics. son syndrome or toxic epidermal necrolysis. N Engl J Med 1995; Chlorpromazini Embonas; Embonato de clorpromazina. Haematological disorders, including haemolytic anae- 333: 1600–7. Хлорпромазина Эмбонат mia, aplastic anaemia, thrombocytopenic purpura, Porphyria. Chlormezanone has been associated with acute at- (C H ClN S) ,C H O = 1026.1. tacks of porphyria and is considered unsafe in porphyric patients. 17 19 2 2 23 16 6 eosinophilia, and a potentially fatal agranulocytosis ATC — N05AA01. have occasionally been reported; they may be manifes- Preparations ATC Vet — QN05AA01. tations of a hypersensitivity reaction. Most cases of Proprietary Preparations (details are given in Part 3) agranulocytosis have occurred within 4 to 10 weeks of Chile: Cardiosedantol; Restoril†. Chlorpromazine Hydrochloride (BANM, rINNM) starting treatment, and symptoms such as sore throat or Multi-ingredient: Chile: Adalgen†; Calmosedan; Diapam; Dioran†; Dol- Aminazine; Chloropromazyny chlorowodorek; Chlorpromazin nix; Dolonase; Dolorelax†; Fibrorelax; Mesolona†; Multisedil; Neo Butar- fever should be watched for and white cell counts insti- trol; Promidan; Sedantol; Sedilit; Silrelax†; Sin-Algin; Hong Kong: Parazone; hydrochlorid; Chlorpromazine, chlorhydrate de; Chlorpromazini S.Afr.: Myoflex. hydrochloridum; Chlorpromazino hidrochloridas; Hidrocloruro tuted should they appear. Mild leucopenia has been de clorpromazina; Klooripromatsiinihydrokloridi; Klorpromazin stated to occur in up to 30% of patients on prolonged Hidroklorür; Klórpromazin-hidroklorid; Klorpromazinhydro- high dosage.