Natural Killer Cell-Based Immunotherapy for Acute Myeloid Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genmab and ADC Therapeutics Announce Amended Agreement for Camidanlumab Tesirine (Cami)
Genmab and ADC Therapeutics Announce Amended Agreement for Camidanlumab Tesirine (Cami) Media Release Copenhagen, Denmark and Lausanne, Switzerland, October 30, 2020 • ADC Therapeutics to continue the development and commercialization of Cami • Genmab to receive mid-to-high single-digit tiered royalty Genmab A/S (Nasdaq: GMAB) and ADC Therapeutics SA (NYSE: ADCT) today announced that they have executed an amended agreement for ADC Therapeutics to continue the development and commercialization of camidanlumab tesirine (Cami). The parties first entered into a collaboration and license agreement in June 2013 for the development of Cami, an antibody drug conjugate (ADC) which combines Genmab’s HuMax®-TAC antibody targeting CD25 with ADC Therapeutics’ highly potent pyrrolobenzodiazepine (PBD) warhead technology. Under the terms of the 2013 agreement, the parties were to determine the path forward for continued development and commercialization of Cami upon completion of a Phase 1a/b clinical trial. ADC Therapeutics previously announced that Cami achieved an overall response rate of 86.5%, including a complete response rate of 48.6%, in Hodgkin lymphoma patients in this trial who had received a median of five prior lines of therapy. Cami is currently being evaluated in a 100-patient pivotal Phase 2 clinical trial intended to support the submission of a Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA). The trial is more than 50 percent enrolled and ADC Therapeutics anticipates reporting interim results in the first half of 2021. “We have a long-standing relationship with the ADC Therapeutics team and believe they are an ideal partner for the ongoing development and potential commercialization of Cami,” said Jan van de Winkel, Ph.D., Chief Executive Officer of Genmab. -

(PDCO) Minutes of the Meeting on 29 January - 01 February 2019
1 March 2019 EMA/PDCO/56017/2019 Inspections, Human Medicines Pharmacovigilance and Committees Division Paediatric Committee (PDCO) Minutes of the meeting on 29 January - 01 February 2019 Chair: Dirk Mentzer – Vice-Chair: Koenraad Norga 29 January 2019, 14:00- 19:00, room 3A 30 January 2019, 08:30- 19:00, room 3A 31 January 2019, 08:30- 19:00, room 3A 01 February 2019, 08:30- 13:00, room 3A Disclaimers Some of the information contained in this set of minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the PDCO Committee meeting reports (after the PDCO Opinion is adopted), and on the Opinions and decisions on paediatric investigation plans webpage (after the EMA Decision is issued). Of note, this set of minutes is a working document primarily designed for PDCO members and the work the Committee undertakes. Further information with relevant explanatory notes can be found at the end of this document. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on-going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). -

For Acute Myeloid Leukemia
Published OnlineFirst September 21, 2010; DOI: 10.1158/1078-0432.CCR-10-0382 Published OnlineFirst on September 21, 2010 as 10.1158/1078-0432.CCR-10-0382 Clinical Therapy Clinical Cancer Research Sequential Cytarabine and α-Particle Immunotherapy with Bismuth-213–Lintuzumab (HuM195) for Acute Myeloid Leukemia Todd L. Rosenblat1, Michael R. McDevitt1, Deborah A. Mulford1, Neeta Pandit-Taskar1, Chaitanya R. Divgi1, Katherine S. Panageas1, Mark L. Heaney1, Suzanne Chanel1, Alfred Morgenstern2, George Sgouros1, Steven M. Larson1, David A. Scheinberg1, and Joseph G. Jurcic1 Abstract Purpose: Lintuzumab (HuM195), a humanized anti-CD33 antibody, targets myeloid leukemia cells and has modest single-agent activity against acute myeloid leukemia (AML). To increase the potency of the antibody without the nonspecific cytotoxicity associated with β-emitters, the α-particle–emitting ra- dionuclide bismuth-213 (213Bi) was conjugated to lintuzumab. This phase I/II trial was conducted to determine the maximum tolerated dose (MTD) and antileukemic effects of 213Bi-lintuzumab, the first targeted α-emitter, after partially cytoreductive chemotherapy. Experimental Design: Thirty-one patients with newly diagnosed (n = 13) or relapsed/refractory (n = 18) AML (median age, 67 years; range, 37-80) were treated with cytarabine (200 mg/m2/d) for 5 days followed by 213Bi-lintuzumab (18.5-46.25 MBq/kg). Results: The MTD of 213Bi-lintuzumab was 37 MB/kg; myelosuppression lasting >35 days was dose limiting. Extramedullary toxicities were primarily limited to grade ≤2 events, including infusion-related reactions. Transient grade 3/4 liver function abnormalities were seen in five patients (16%). Treatment- related deaths occurred in 2 of 21 (10%) patients who received the MTD. -

ADC Therapeutics SA (Exact Name of Registrant As Specified in Its Charter)
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 6-K REPORT OF FOREIGN PRIVATE ISSUER PURSUANT TO RULE 13a-16 OR 15d-16 UNDER THE SECURITIES EXCHANGE ACT OF 1934 For the month of July, 2020. Commission File Number: 001-39071 ADC Therapeutics SA (Exact name of registrant as specified in its charter) Biopôle Route de la Corniche 3B 1066 Epalinges Switzerland (Address of principal executive office) Indicate by check mark whether the registrant files or will file annual reports under cover of Form 20-F or Form 40-F: Form 20-F ☒ Form 40-F Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(1): ☐ Indicate by check mark if the registrant is submitting the Form 6-K in paper as permitted by Regulation S-T Rule 101(b)(7): ☐ SIGNATURE Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized. ADC Therapeutics SA Date: July 6, 2020 By: /s/ Dominique Graz Name: Dominique Graz Title: General Counsel EXHIBIT INDEX Exhibit No. Description 99.1 Press release dated July 6, 2020 Exhibit 99.1 ADC Therapeutics Announces U.S. Food and Drug Administration Has Lifted Partial Clinical Hold on Pivotal Phase 2 Clinical Trial of Camidanlumab Tesirine Lausanne, Switzerland — July 6, 2020 — ADC Therapeutics SA (NYSE:ADCT), a clinical-stage oncology-focused biotechnology company leading the development and commercialization of next-generation antibody drug conjugates (ADCs) with highly potent and targeted pyrrolobenzodiazepine (PBD) dimer technology, today announced that the U.S. -

Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model
Downloaded from http://www.jimmunol.org/ by guest on September 25, 2021 T + is online at: average * The Journal of Immunology , 34 of which you can access for free at: 2016; 197:1477-1488; Prepublished online 1 July from submission to initial decision 4 weeks from acceptance to publication 2016; doi: 10.4049/jimmunol.1600589 http://www.jimmunol.org/content/197/4/1477 Molecular Profile of Tumor-Specific CD8 Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. Waugh, Sonia M. Leach, Brandon L. Moore, Tullia C. Bruno, Jonathan D. Buhrman and Jill E. Slansky J Immunol cites 95 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2016/07/01/jimmunol.160058 9.DCSupplemental This article http://www.jimmunol.org/content/197/4/1477.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 25, 2021. The Journal of Immunology Molecular Profile of Tumor-Specific CD8+ T Cell Hypofunction in a Transplantable Murine Cancer Model Katherine A. -
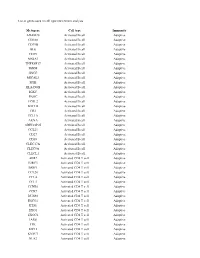
List of Genes Used in Cell Type Enrichment Analysis
List of genes used in cell type enrichment analysis Metagene Cell type Immunity ADAM28 Activated B cell Adaptive CD180 Activated B cell Adaptive CD79B Activated B cell Adaptive BLK Activated B cell Adaptive CD19 Activated B cell Adaptive MS4A1 Activated B cell Adaptive TNFRSF17 Activated B cell Adaptive IGHM Activated B cell Adaptive GNG7 Activated B cell Adaptive MICAL3 Activated B cell Adaptive SPIB Activated B cell Adaptive HLA-DOB Activated B cell Adaptive IGKC Activated B cell Adaptive PNOC Activated B cell Adaptive FCRL2 Activated B cell Adaptive BACH2 Activated B cell Adaptive CR2 Activated B cell Adaptive TCL1A Activated B cell Adaptive AKNA Activated B cell Adaptive ARHGAP25 Activated B cell Adaptive CCL21 Activated B cell Adaptive CD27 Activated B cell Adaptive CD38 Activated B cell Adaptive CLEC17A Activated B cell Adaptive CLEC9A Activated B cell Adaptive CLECL1 Activated B cell Adaptive AIM2 Activated CD4 T cell Adaptive BIRC3 Activated CD4 T cell Adaptive BRIP1 Activated CD4 T cell Adaptive CCL20 Activated CD4 T cell Adaptive CCL4 Activated CD4 T cell Adaptive CCL5 Activated CD4 T cell Adaptive CCNB1 Activated CD4 T cell Adaptive CCR7 Activated CD4 T cell Adaptive DUSP2 Activated CD4 T cell Adaptive ESCO2 Activated CD4 T cell Adaptive ETS1 Activated CD4 T cell Adaptive EXO1 Activated CD4 T cell Adaptive EXOC6 Activated CD4 T cell Adaptive IARS Activated CD4 T cell Adaptive ITK Activated CD4 T cell Adaptive KIF11 Activated CD4 T cell Adaptive KNTC1 Activated CD4 T cell Adaptive NUF2 Activated CD4 T cell Adaptive PRC1 Activated -

Finding Drug Targeting Mechanisms with Genetic Evidence for Parkinson’S Disease
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.24.208975; this version posted July 24, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Finding drug targeting mechanisms with genetic evidence for Parkinson’s disease Catherine S. Storm1,*, Demis A. Kia1, Mona Almramhi1, Sara Bandres-Ciga2, Chris Finan3, Aroon D. Hingorani3,4,5, International Parkinson’s Disease Genomics Consortium (IPDGC), Nicholas W. Wood1,6,* 1 Department of Clinical and Movement Neurosciences, University College London Queen Square Institute of Neurology, London, WC1N 3BG, United Kingdom 2 Molecular Genetics Section, Laboratory of Neurogenetics, National Institute on Aging, National Institutes of Health, Bethesda, MD 20892, United States of America 3 Institute of Cardiovascular Science, Faculty of Population Health, University College London, London WC1E 6BT, United Kingdom 4 University College London British Heart Foundation Research Accelerator Centre, New Delhi, India 5 Health Data Research UK, 222 Euston Road, London, United Kingdom 6 Lead Contact * Correspondence: [email protected] (CSS), [email protected] (NWW) Summary Parkinson’s disease (PD) is a neurodegenerative movement disorder that currently has no disease-modifying treatment, partly owing to inefficiencies in drug target identification and validation using human evidence. Here, we use Mendelian randomization to investigate more than 3000 genes that encode druggable proteins, seeking to predict their efficacy as drug targets for PD. We use expression and protein quantitative trait loci for druggable genes to mimic exposure to medications, and we examine the causal effect on PD risk (in two large case-control cohorts), PD age at onset and progression. -

A Molecular Switch from STAT2-IRF9 to ISGF3 Underlies Interferon-Induced Gene Transcription
ARTICLE https://doi.org/10.1038/s41467-019-10970-y OPEN A molecular switch from STAT2-IRF9 to ISGF3 underlies interferon-induced gene transcription Ekaterini Platanitis 1, Duygu Demiroz1,5, Anja Schneller1,5, Katrin Fischer1, Christophe Capelle1, Markus Hartl 1, Thomas Gossenreiter 1, Mathias Müller2, Maria Novatchkova3,4 & Thomas Decker 1 Cells maintain the balance between homeostasis and inflammation by adapting and inte- grating the activity of intracellular signaling cascades, including the JAK-STAT pathway. Our 1234567890():,; understanding of how a tailored switch from homeostasis to a strong receptor-dependent response is coordinated remains limited. Here, we use an integrated transcriptomic and proteomic approach to analyze transcription-factor binding, gene expression and in vivo proximity-dependent labelling of proteins in living cells under homeostatic and interferon (IFN)-induced conditions. We show that interferons (IFN) switch murine macrophages from resting-state to induced gene expression by alternating subunits of transcription factor ISGF3. Whereas preformed STAT2-IRF9 complexes control basal expression of IFN-induced genes (ISG), both type I IFN and IFN-γ cause promoter binding of a complete ISGF3 complex containing STAT1, STAT2 and IRF9. In contrast to the dogmatic view of ISGF3 formation in the cytoplasm, our results suggest a model wherein the assembly of the ISGF3 complex occurs on DNA. 1 Max Perutz Labs (MPL), University of Vienna, Vienna 1030, Austria. 2 Institute of Animal Breeding and Genetics, University of Veterinary Medicine Vienna, Vienna 1210, Austria. 3 Institute of Molecular Biotechnology of the Austrian Academy of Sciences (IMBA), Vienna 1030, Austria. 4 Research Institute of Molecular Pathology (IMP), Vienna Biocenter (VBC), Vienna 1030, Austria. -

Systemic Immunotherapy for Urothelial Cancer: Current Trends and Future Directions
Review Systemic Immunotherapy for Urothelial Cancer: Current Trends and Future Directions Shilpa Gupta 1,†, David Gill 2,†, Austin Poole 2 and Neeraj Agarwal 2,* 1 Masonic Cancer Center, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] 2 Huntsman Cancer Institute, University of Utah, Salt Lake City, UT 84112, USA; [email protected] (D.G.); [email protected] (A.P.) * Correspondence: [email protected]; Tel.: +1-801-213-5658; Fax: +1-801-585-0124 † These authors contributed equally to this work. Academic Editor: Vita Golubovskaya Received: 14 December 2016; Accepted: 18 January 2017; Published: 27 January 2017 Abstract: Urothelial cancer of the bladder, renal pelvis, ureter, and other urinary organs is the fifth most common cancer in the United States, and systemic platinum-based chemotherapy remains the standard of care for first-line treatment of advanced/metastatic urothelial carcinoma (UC). Until recently, there were very limited options for patients who are refractory to chemotherapy, or do not tolerate chemotherapy due to toxicities and overall outcomes have remained very poor. While the role of immunotherapy was first established in non-muscle invasive bladder cancer in the 1970s, no systemic immunotherapy was approved for advanced disease until the recent approval of a programmed death ligand-1 (PD-L1) inhibitor, atezolizumab, in patients with advanced/metastatic UC who have progressed on platinum-containing regimens. This represents a significant milestone in this disease after a void of over 30 years. In addition to atezolizumab, a variety of checkpoint inhibitors have shown a significant activity in advanced/metastatic urothelial carcinoma and are expected to gain Food and Drug Administration (FDA) approval in the near future. -

LAG-3: from Molecular Functions to Clinical Applications
Open access Review J Immunother Cancer: first published as 10.1136/jitc-2020-001014 on 13 September 2020. Downloaded from LAG-3: from molecular functions to clinical applications Takumi Maruhashi , Daisuke Sugiura , Il- mi Okazaki , Taku Okazaki To cite: Maruhashi T, Sugiura D, ABSTRACT (PD-1) and cytotoxic T lymphocyte antigen Okazaki I, et al. LAG-3: from To prevent the destruction of tissues owing to excessive 4 (CTLA-4) significantly improved the molecular functions to clinical and/or inappropriate immune responses, immune outcomes of patients with diverse cancer applications. Journal for cells are under strict check by various regulatory ImmunoTherapy of Cancer types, revolutionizing cancer treatment. The mechanisms at multiple points. Inhibitory coreceptors, 2020;8:e001014. doi:10.1136/ success of these therapies verified that inhib- including programmed cell death 1 (PD-1) and cytotoxic jitc-2020-001014 itory coreceptors serve as critical checkpoints T lymphocyte antigen 4 (CTLA-4), serve as critical checkpoints in restricting immune responses against for immune cells to not attack the tumor Accepted 29 July 2020 self- tissues and tumor cells. Immune checkpoint inhibitors cells as well as self-tissues. However, response that block PD-1 and CTLA-4 pathways significantly rates are typically lower and immune-related improved the outcomes of patients with diverse cancer adverse events (irAEs) are also observed in types and have revolutionized cancer treatment. However, patients administered with immune check- response rates to such therapies are rather limited, and point inhibitors. This is indicative of the immune-rela ted adverse events are also observed in a continued need to decipher the complex substantial patient population, leading to the urgent need biology of inhibitory coreceptors to increase for novel therapeutics with higher efficacy and lower response rates and prevent such unwanted toxicity. -

9.0 Bn 23 000 200 +
42 | Novartis Annual Report 2017 Innovation The Novartis Institutes for BioMedical Research works in concert with our Global Drug Development group to bring innovative treatments to patients around the world. In 2017, we advanced our drug discovery and development efforts by encouraging greater collaboration and out-of-the-box thinking, exploring new approaches that could improve how we work, and investing in promising tools and technologies. We made progress in priority disease areas with high unmet medical needs. We also marked several key milestones, including US FDA approval – the first of its kind – for a type of personalized cell therapy that could change the course of cancer care. 9.0 bn 23 000 200 + Research and development Scientists, physicians and business Projects in clinical development spending in 2017, amounting to professionals working in research 18.3% of net sales (USD) and development worldwide Collaborative Efficient, effective Progress in important science drug development disease areas We are increasing collaboration We are using digital technology We highlight areas of our work where in research as we try to leverage and data analysis to make drug we are driving significant innovation, innovation from a variety of sources. development swifter and more or where we can potentially have an We are also exploring ways to effective. And we are taking steps important impact on patients and harness digital technology in drug to strengthen our pipeline. public health. discovery, as well as new therapeutic k page 46 k Immuno-oncology page 48 approaches such as cell therapies. k Multiple sclerosis page 50 k page 43 k Liver disease page 52 k Ophthalmology page 53 k Asthma page 55 k Malaria page 56 INNOVATION Novartis Annual Report 2017 | 43 Discovery For new treatments, the journey from laboratory to patient Promoting open innovation starts in the discovery phase where researchers try to Our efforts to increase the flow of ideas between identify potentially groundbreaking therapies. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products.