Synopsis – Study 11915A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bifeprunox: a Novel Antipsychotic Agent with Partial Agonist Properties at Dopamine D2 and Serotonin 5-HT1A Receptors
DRUG EVALUATION Bifeprunox: a novel antipsychotic agent with partial agonist properties at dopamine D2 and serotonin 5-HT1A receptors Marie-Louise G Most second-generation, atypical, dopamine (DA) D2/5-HT2 blocking antipsychotics still Wadenberg induce extrapyramidal side effects (EPS) in higher doses. Weight gain and metabolic University of Kalmar, disturbances are also a problem, and negative and cognitive symptoms have not been Department of Natural Sciences, Norra Vagen 49, sufficiently addressed. The current brain DA mesolimbic hyperactive/mesocortical SE-391 82 Kalmar, Sweden hypoactive hypothesis of schizophrenia suggests that DA D2/5-HT1A receptor partial agonist Tel.: +46 480 446 277; properties may be more efficacious with less side effects. DA D2 receptor partial agonists Fax: +46 480 446 244; may stabilize a hyperactive/hypoactive DA condition. Additional 5-HT stimulation may marie-louise.wadenberg@ 1A hik.se enhance therapeutic efficacy and also improve EPS liability profile. In clinical trials in schizophrenic patients, the novel DA D2/5-HT1A partial agonist bifeprunox indeed demonstrates therapeutic efficacy, a safe EPS profile and appears beneficial regarding weight gain, prolactin, blood lipid and glucose levels and cardiac rhythm. The data on bifeprunox are promising and suggest that combined DA D2/5-HT1A partial agonism may well be important properties for future-generation antipsychotics. Bifeprunox, a novel antipsychotic agent with a (DA D1, D2, D4, 5-HT2A/C, 5-HT1A, hista- so-called third-generation atypical pharmacolog- mine H1, α1, α2, cholinergic muscarinic recep- ical profile, is currently in clinical trials and tor affinity) and comparatively lower affinity for expected to launch as a schizophrenia therapy in the DA D2 receptor than traditional APDs. -

HTR1A Polymorphisms and Clinical Efficacy Of
International Journal of Neuropsychopharmacology, (2016) 19(5): 1–10 doi:10.1093/ijnp/pyv125 Advance Access publication November 14, 2015 Research Article research article HTR1A Polymorphisms and Clinical Efficacy of Antipsychotic Drug Treatment in Schizophrenia: A Meta-Analysis Yoshiteru Takekita, MD, PhD; Chiara Fabbri, MD; Masaki Kato, MD, PhD; Yosuke Koshikawa, MA; Aran Tajika, MD; Toshihiko Kinoshita, MD, PhD; Alessandro Serretti, MD, PhD Department of Biomedical and NeuroMotor Sciences, University of Bologna, Bologna, Italy (Drs Takekita, Fabbri, and Serretti); Department of Neuropsychiatry, Kansai Medical University, Osaka, Japan (Drs Takekita, Kato, Koshikawa, and Kinoshita); Department of Health Promotion and Human Behavior, Kyoto University Graduate School of Medicine/School of Public Health, Kyoto, Japan (Dr Tajika). Correspondence: Yoshiteru Takekita, MD, PhD, Department of Biomedical and NeuroMotor Sciences, University of Bologna, Bologna, Viale Carlo Pepoli 5, Bologna, 40123, Italy ([email protected]). Abstract Background: This meta-analysis was conducted to evaluate whether HTR1A gene polymorphisms impact the efficacy of antipsychotic drugs in patients with schizophrenia. Methods: Candidate gene studies that were published in English up to August 6, 2015 were identified by a literature search of PubMed, Web of Science, and Google scholar. Data were pooled from individual clinical trials considering overall symptoms, positive symptoms and negative symptoms, and standard mean differences were calculated by applying a random-effects model. Results: The present meta-analysis included a total of 1281 patients from 10 studies. Three polymorphisms of HTR1A (rs6295, rs878567, and rs1423691) were selected for the analysis. In the pooled data from all studies, none of these HTR1A polymorphisms correlated significantly with either overall symptoms or positive symptoms. -

The Role of Kinetic Context in Apparent Biased Agonism at Gpcrs
ARTICLE Received 2 Jul 2015 | Accepted 27 Jan 2016 | Published 24 Feb 2016 DOI: 10.1038/ncomms10842 OPEN The role of kinetic context in apparent biased agonism at GPCRs Carmen Klein Herenbrink1, David A. Sykes2, Prashant Donthamsetti3,4, Meritxell Canals1, Thomas Coudrat1, Jeremy Shonberg5, Peter J. Scammells5, Ben Capuano5, Patrick M. Sexton1, Steven J. Charlton2, Jonathan A. Javitch3,4,6, Arthur Christopoulos1 & J Robert Lane1 Biased agonism describes the ability of ligands to stabilize different conformations of a GPCR linked to distinct functional outcomes and offers the prospect of designing pathway-specific drugs that avoid on-target side effects. This mechanism is usually inferred from pharmaco- logical data with the assumption that the confounding influences of observational (that is, assay dependent) and system (that is, cell background dependent) bias are excluded by experimental design and analysis. Here we reveal that ‘kinetic context’, as determined by ligand-binding kinetics and the temporal pattern of receptor-signalling processes, can have a profound influence on the apparent bias of a series of agonists for the dopamine D2 receptor and can even lead to reversals in the direction of bias. We propose that kinetic context must be acknowledged in the design and interpretation of studies of biased agonism. 1 Drug Discovery Biology, Monash Institute of Pharmaceutical Sciences, Monash University, 381 Royal Parade, Parkville, Victoria 3052, Australia. 2 Cell Signalling Research Group, School of Life Sciences, University of Nottingham, Queen’s Medical Centre, Nottingham NG7 2UH, UK. 3 Departments of Psychiatry, College of Physicians and Surgeons, Columbia University, New York, New York 10032, USA. 4 Department of Pharmacology, College of Physicians and Surgeons, Columbia University, New York, New York 10032, USA. -

Symposium: the Role of 5-HT1AR in Pathophysiology and Treatment Of
Abstracts for oral sessions / European Psychiatry 23 (2008) S1eS80 S61 S51.05 Our transgenic mice showed no overall cognitive deficit. As a ten- Treatment-seeking gamblers and Parkinson’s disease: Case reports dency, inhibitory avoidance retention was impaired in transgenic mice compared to wild-type controls. Both genotypes showed similar O. Simon. Center for Pathological Gambling, Community Psychiatry spatial learning abilities in the Morris water maze and habituated to Services, Department of Adult Psychiatry, University Hospital of the hole-board in a comparable manner. Anterograde amnesia in- Lausanne, Lausanne, Switzerland duced by 8-OH-DPAT was in transgenic mice already apparent in a third of the dose used for wild-type mice. Retrograde amnesia could Pathological gambling (PG) is a rare but well-established behavioural not be triggered. disorders of Parkinson’s disease (PD) patients treated with dopamine agonist. We investigate the chronological relationship between PD Since the transgenic mice show untreated a rather normal be- and diagnosis of PG within treatment-seeking gamblers. haviour, we assume that they possess compensatory mechanisms. However, after activation of the postsynaptic 5-HT1A-receptors Sample and Methods: From 174 consecutively admitted patho- the differences between wild-type and transgenic mice became logical gamblers we identified 4 patients with PD. Standardized med- more clear. Hence, our findings suggest that the cortical and hip- ical records include socio-demographic characteristics, past gaming pocampal 5-HT1A-receptors play rather a modulatory role in behaviours and gambling-treatment modalities as well as the evolu- learning. tion of PD and the pro-dopaminergic medication history. Results: All four patients developed PG after the onset of PD S48.02 treatment. -

Antipsychotics
The Fut ure of Antipsychotic Therapy (page 7 in syllabus) Stepp,,hen M. Stahl, MD, PhD Adjunct Professor, Department of Psychiatry Universityyg of California, San Diego School of Medicine Honorary Visiting Senior Fellow, Cambridge University, UK Sppyonsored by the Neuroscience Education Institute Additionally sponsored by the American Society for the Advancement of Pharmacotherapy This activity is supported by an educational grant from Sunovion Pharmaceuticals Inc. Copyright © 2011 Neuroscience Education Institute. All rights reserved. Individual Disclosure Statement Faculty Editor / Presenter Stephen M. Stahl, MD, PhD, is an adjunct professor in the department of psychiatry at the University of California, San Diego School of Medicine, and an honorary visiting senior fellow at the University of Cambridge in the UK. Grant/Research: AstraZeneca, BioMarin, Dainippon Sumitomo, Dey, Forest, Genomind, Lilly, Merck, Pamlab, Pfizer, PGxHealth/Trovis, Schering-Plough, Sepracor/Sunovion, Servier, Shire, Torrent Consultant/Advisor: Advent, Alkermes, Arena, AstraZeneca, AVANIR, BioMarin, Biovail, Boehringer Ingelheim, Bristol-Myers Squibb, CeNeRx, Cypress, Dainippon Sumitomo, Dey, Forest, Genomind, Janssen, Jazz, Labopharm, Lilly, Lundbeck, Merck, Neuronetics, Novartis, Ono, Orexigen, Otsuka, Pamlab, Pfizer, PGxHealth/Trovis, Rexahn, Roche, Royalty, Schering-Plough, Servier, Shire, Solvay/Abbott, Sunovion/Sepracor, Valeant, VIVUS, Speakers Bureau: Dainippon Sumitomo, Forest, Lilly, Merck, Pamlab, Pfizer, Sepracor/Sunovion, Servier, Wyeth Copyright © 2011 Neuroscience Education Institute. All rights reserved. Learninggj Objectives • Differentiate antipsychotic drugs from each other on the basis of their pharmacological mechanisms and their associated therapeutic and side effects • Integrate novel treatment approaches into clinical practice according to best practices guidelines • Identify novel therapeutic options currently being researched for the treatment of schizophrenia Copyright © 2011 Neuroscience Education Institute. -

Maintenance Treatment with Antipsychotic Drugs for Schizophrenia (Review)
Maintenance treatment with antipsychotic drugs for schizophrenia (Review) Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Davis JM This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2012, Issue 5 http://www.thecochranelibrary.com Maintenance treatment with antipsychotic drugs for schizophrenia (Review) Copyright © 2012 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 3 BACKGROUND .................................... 5 OBJECTIVES ..................................... 5 METHODS ...................................... 5 RESULTS....................................... 10 Figure1. ..................................... 12 Figure2. ..................................... 15 Figure3. ..................................... 16 Figure4. ..................................... 18 Figure5. ..................................... 23 Figure6. ..................................... 24 Figure7. ..................................... 26 DISCUSSION ..................................... 27 AUTHORS’CONCLUSIONS . 32 ACKNOWLEDGEMENTS . 32 REFERENCES ..................................... 33 CHARACTERISTICSOFSTUDIES . 43 DATAANDANALYSES. 143 Analysis 1.1. Comparison 1 Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 1 Relapse:upto3months.. 147 Analysis -

United States Patent (10 ) Patent No.: US 10,660,887 B2 Javitt (45 ) Date of Patent: *May 26 , 2020
US010660887B2 United States Patent (10 ) Patent No.: US 10,660,887 B2 Javitt (45 ) Date of Patent : *May 26 , 2020 (54 ) COMPOSITION AND METHOD FOR (56 ) References Cited TREATMENT OF DEPRESSION AND PSYCHOSIS IN HUMANS U.S. PATENT DOCUMENTS 6,228,875 B1 5/2001 Tsai et al. ( 71 ) Applicant : Glytech , LLC , Ft. Lee , NJ (US ) 2004/0157926 A1 * 8/2004 Heresco - Levy A61K 31/198 514/561 (72 ) Inventor: Daniel C. Javitt , Ft. Lee , NJ (US ) 2005/0261340 Al 11/2005 Weiner 2006/0204486 Al 9/2006 Pyke et al . 2008/0194631 Al 8/2008 Trovero et al. ( 73 ) Assignee : GLYTECH , LLC , Ft. Lee , NJ (US ) 2008/0194698 A1 8/2008 Hermanussen et al . 2010/0069399 A1 * 3/2010 Gant CO7D 401/12 ( * ) Notice : Subject to any disclaimer, the term of this 514 / 253.07 patent is extended or adjusted under 35 2010/0216805 Al 8/2010 Barlow 2011/0207776 Al 8/2011 Buntinx U.S.C. 154 ( b ) by 95 days . 2011/0237602 A1 9/2011 Meltzer This patent is subject to a terminal dis 2011/0306586 Al 12/2011 Khan claimer . 2012/0041026 A1 2/2012 Waizumi ( 21 ) Appl. No.: 15 /650,912 FOREIGN PATENT DOCUMENTS CN 101090721 12/2007 ( 22 ) Filed : Jul. 16 , 17 KR 2007 0017136 2/2007 WO 2005/065308 7/2005 (65 ) Prior Publication Data WO 2005/079756 9/2005 WO 2011044089 4/2011 US 2017/0312275 A1 Nov. 2 , 2017 WO 2012/104852 8/2012 WO 2005/000216 9/2013 WO 2013138322 9/2013 Related U.S. Application Data (63 ) Continuation of application No. -
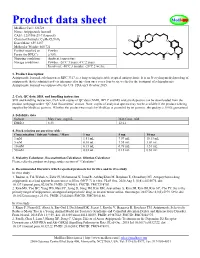
Product Data Sheet
Product data sheet MedKoo Cat#: 326728 Name: Aripiprazole lauroxil CAS#: 1259305-29-7 (lauroxil) Chemical Formula: C36H51Cl2N3O4 Exact Mass: 659.3257 Molecular Weight: 660.721 Product supplied as: Powder Purity (by HPLC): ≥ 98% Shipping conditions Ambient temperature Storage conditions: Powder: -20°C 3 years; 4°C 2 years. In solvent: -80°C 3 months; -20°C 2 weeks. 1. Product description: Aripiprazole lauroxil, aslo known as RDC 3317, is a long-acting injectable atypical antipsychotic. It is an N-acyloxymethyl prodrug of aripiprazole that is administered via intramuscular injection once every four to six weeks for the treatment of schizophrenia. Aripiprazole lauroxil was approved by the U.S. FDA on 5 October 2015. 2. CoA, QC data, SDS, and handling instruction SDS and handling instruction, CoA with copies of QC data (NMR, HPLC and MS analytical spectra) can be downloaded from the product web page under “QC And Documents” section. Note: copies of analytical spectra may not be available if the product is being supplied by MedKoo partners. Whether the product was made by MedKoo or provided by its partners, the quality is 100% guaranteed. 3. Solubility data Solvent Max Conc. mg/mL Max Conc. mM DMSO 8.33 12.61 4. Stock solution preparation table: Concentration / Solvent Volume / Mass 1 mg 5 mg 10 mg 1 mM 1.51 mL 7.57 mL 15.13 mL 5 mM 0.30 mL 1.51 mL 3.03 mL 10 mM 0.15 mL 0.76 mL 1.51 mL 50 mM 0.03 mL 0.15 mL 0.30 mL 5. -

Current Topics in Medicinal Chemistry, 2016, 16, 3385-3403 REVIEW ARTICLE
Send Orders for Reprints to [email protected] 3385 Cur rent Topics in Medicinal Chemistry, 2016, 16, 3385-3403 REVIEW ARTICLE ISSN: 1568-0266 eISSN: 1873-5294 Dopamine Targeting Drugs for the Treatment of Schizophrenia: Past, Impact Factor: 2.9 The international Present and Future journal for in-depth reviews on Current Topics in Medicinal Chemistry BENTHAM SCIENCE Peng Li*, Gretchen L. Snyder and Kimberly E. Vanover Intra-Cellular Therapies Inc, 430 East 29th Street, Suite 900, New York, NY 10016, USA Abstract: Schizophrenia is a chronic and debilitating neuropsychiatric disorder affecting approxi- mately 1% of the world’s population. This disease is associated with considerable morbidity placing a major financial burden on society. Antipsychotics have been the mainstay of the pharmacological treatment of schizophrenia for decades. The traditional typical and atypical antipsychotics demon- strate clinical efficacy in treating positive symptoms, such as hallucinations and delusions, while are A R T I C L E H I S T O R Y largely ineffective and may worsen negative symptoms, such as blunted affect and social withdrawal, as well as cognitive function. The inability to treat these latter symptoms may contribute to social Received: April 07, 2016 Revised: May 20, 2016 function impairment associated with schizophrenia. The dysfunction of multiple neurotransmitter Accepted: May 23, 2016 systems in schizophrenia suggests that drugs selectively targeting one neurotransmission pathway DOI: 10.2174/1568026616666160608 are unlikely to meet all the therapeutic needs of this heterogeneous disorder. Often, however, the un- 084834 intentional engagement of multiple pharmacological targets or even the excessive engagement of in- tended pharmacological targets can lead to undesired consequences and poor tolerability. -

Drug Delivery System for Use in the Treatment Or Diagnosis of Neurological Disorders
(19) TZZ __T (11) EP 2 774 991 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.09.2014 Bulletin 2014/37 C12N 15/86 (2006.01) A61K 48/00 (2006.01) (21) Application number: 13001491.3 (22) Date of filing: 22.03.2013 (84) Designated Contracting States: • Manninga, Heiko AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 37073 Göttingen (DE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO •Götzke,Armin PL PT RO RS SE SI SK SM TR 97070 Würzburg (DE) Designated Extension States: • Glassmann, Alexander BA ME 50999 Köln (DE) (30) Priority: 06.03.2013 PCT/EP2013/000656 (74) Representative: von Renesse, Dorothea et al König-Szynka-Tilmann-von Renesse (71) Applicant: Life Science Inkubator Betriebs GmbH Patentanwälte Partnerschaft mbB & Co. KG Postfach 11 09 46 53175 Bonn (DE) 40509 Düsseldorf (DE) (72) Inventors: • Demina, Victoria 53175 Bonn (DE) (54) Drug delivery system for use in the treatment or diagnosis of neurological disorders (57) The invention relates to VLP derived from poly- ment or diagnosis of a neurological disease, in particular oma virus loaded with a drug (cargo) as a drug delivery multiple sclerosis, Parkinsons’s disease or Alzheimer’s system for transporting said drug into the CNS for treat- disease. EP 2 774 991 A1 Printed by Jouve, 75001 PARIS (FR) EP 2 774 991 A1 Description FIELD OF THE INVENTION 5 [0001] The invention relates to the use of virus like particles (VLP) of the type of human polyoma virus for use as drug delivery system for the treatment or diagnosis of neurological disorders. -

Handbook of Experimental Pharmacology Volume
Handbook of Experimental Pharmacology Volume 212 Editor-in-Chief F.B. Hofmann, München Editorial Board J.A. Beavo, Seattle J.E. Barrett, Philadelphia D. Ganten, Berlin P. Geppetti, Florence M.C. Michel, Ingelheim C.P. Page, London W. Rosenthal, Berlin For further volumes: http://www.springer.com/series/164 . Gerhard Gross • Mark A. Geyer Editors Current Antipsychotics Editors Gerhard Gross Mark A. Geyer Abbott, Neuroscience Research, GPRD University of California San Diego Ludwigshafen, Germany Department of Psychiatry Institut fu¨r Pharmakologie La Jolla Universita¨t Duisburg-Essen California Universita¨tsklinikum Essen USA Essen Germany ISSN 0171-2004 ISSN 1865-0325 (electronic) ISBN 978-3-642-25760-5 ISBN 978-3-642-25761-2 (eBook) DOI 10.1007/978-3-642-25761-2 Springer Heidelberg New York Dordrecht London Library of Congress Control Number: 2012952465 # Springer-Verlag Berlin Heidelberg 2012 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. -
Handbook of Schizophrenia Spectrum Disorders, Volume III
Handbook of Schizophrenia Spectrum Disorders, Volume III Michael S. Ritsner Editor Handbook of Schizophrenia Spectrum Disorders, Volume III Therapeutic Approaches, Comorbidity, and Outcomes 123 Editor Michael S. Ritsner Technion – Israel Institute of Technology Rappaport Faculty of Medicine Haifa Israel [email protected] ISBN 978-94-007-0833-4 e-ISBN 978-94-007-0834-1 DOI 10.1007/978-94-007-0834-1 Springer Dordrecht Heidelberg London New York Library of Congress Control Number: 2011924745 © Springer Science+Business Media B.V. 2011 No part of this work may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording or otherwise, without written permission from the Publisher, with the exception of any material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) Foreword Schizophrenia Spectrum Disorders: Insights from Views Across 100 years Schizophrenia spectrum and related disorders such as schizoaffective and mood dis- orders, schizophreniform disorders, brief psychotic disorders, delusional and shared psychotic disorders, and personality (i.e., schizotypal, paranoid, and schizoid per- sonality) disorders are the most debilitating forms of mental illness, worldwide. There are 89,377 citations (including 10,760 reviews) related to “schizophrenia” and 2118 (including 296 reviews) related to “schizophrenia spectrum” in PubMed (accessed on August 12, 2010). The classification of these disorders, in particular, of schizophrenia, schizoaf- fective and mood disorders (referred to as functional psychoses), has been debated for decades, and its validity remains controversial.