EXTRAS Trial Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Student Protection Plan
Nottingham Trent University Student Protection Plan UKPRN: 10004797 Legal Address: 50 Shakespeare Street, Nottingham, NG1 4FQ, UK Contact Point for Enquires about this Plan: Deputy Vice Chancellor (Academic Development and Performance) Student Protection Plan for 2020/21 academic year: Nottingham Trent University 1. Scope and identification of Risks Introduction: In accordance with the requirements of the Higher Education and Research Act 2017, this plan inform students of what they can expect should a course, campus or institution close. This Student Protection Plan (hereafter “the Plan”) aims to demonstrate that Nottingham Trent University (NTU) has considered how students can continue or complete their studies or be compensated if this is not possible. The University recognises that in the event of a significant course or campus closure it will be expected to work closely with the Office for Students and its own student body to ensure that students’ interests are protected through any such change. Nottingham Trent University is a large, established, high performing and financially stable provider. We would like to reassure both our students and applicants that the risks outlined in this Plan are all very low and in the case of closure extremely low. Examples of risks to which this Plan would apply: • Loss or restriction of University status or its degree awarding powers or its designation for student support or student intake; • Decision to close the institution, a campus or a specialist facility; • Long term disruption to your course -

Engagement with North America Brochure
Our engagement with North America 2 North America A warm welcome from the University of the Year At Birmingham, we are proud not only of our roots but of our ambition. Our recent recognition as University of the Year 2014 by The Times and The Sunday Times cements our place in the top 100 universities in the world; acknowledging Birmingham as a forward-thinking institution with civic roots, national eminence and global reach. We believe Birmingham is a truly global Our international strategy is evidenced to date are varied, ranging from student exchanges and university; a prestigious institution boasting by numerous significant initiatives including our teaching partnerships to joint research on global global experts who address the future challenges landmark Birmingham Guangzhou Centre, a issues and cultural engagement. facing the modern-day world. Our global novel partnership with the municipal government footprint is both distinctive and expanding. We in Guangzhou; our considerable joint investment As the world of higher education continues are developing our international presence and with The University of Nottingham in Brazil; to change at an unprecedented rate, collaborations across academia, industry, culture extensive engagement with partners in Chicago Birmingham continues to adapt to meet the and government across all continents. and the American Midwest; and our permanent global challenges and opportunities ahead. presence in New Delhi, Shanghai, We will continue to develop the quality and With almost 5,000 international students from Nigeria and Brussels. distinctiveness which defines us locally more than 150 countries, and a third of our and represents us as a global university. academic staff from overseas, our campus is Our ties with North America are of key truly a diverse and global place. -

Curriculum Vitae (Curriculum Vitae)
Kostas Vasilopoulos Teaching Associate Lancaster University kvasilopoulos.com | R [email protected] | kvasilopoulos | ¯ kvasilopoulos Q [email protected] | Ó+44 (0) 7392971743 Research Interests Macroeconomics, Real Estate Markets, Time Series Modeling, Credit Frictions, Dynamic Stochastic General Equilibrium (DSGE) modelling Employment Teaching Associate Nov 2020 - Lancaster University Lancaster, UK Research Assistant, UK Housing Observatory Mar 2019 - Sep 2020 Lancaster University Lancaster, UK Graduate Teaching Assistant Oct 2016 - Sep 2020 Lancaster University Lancaster, UK Education Ph.D. Economics Oct 2016 - Nov 2020 Lancaster University Lancaster, UK M.Sc. Economics Sept 2014 - March 2016 University of Macedonia Thessaloniki, Greece B.Sc. Economics Sept 2009 - Aug 2014 University of Macedonia Thessaloniki, Greece Research Publications • Pavlidis E., Vasilopoulos K. (2020). Speculative Bubbles in Segmented Markets: Evidence from Chinese Cross-Listed Stocks. Journal of International Money and Finance . Submitted • Vasilopoulos K., Pavlidis E., Martínez-García E.(2020). exuber: Recursive Right-Tailed Unit Root Testing with R. Dallas Fed Working Paper. • Vasilopoulos K., Tayler W. (2020). Real Estate and Construction Sector Dynamics in the Business Cycle. Working Paper 1 1/4 Work in Progress • Pavlidis E., Vasilopoulos K. (2020). Sentimental Housing Markets. • Vasilopoulos K. (2020). Real Estate and Monetary Policy: Residential and Commercial. • Skouralis A., Vasilopoulos K. (2020). Asymmetries Effects of Housing -

Newsletter: Special Issue Connected Everything Conference 2018 Manufacturing a Brave New World Newcastle University, 26Th and 27Th June 2018
Newsletter: Special Issue Connected Everything Conference 2018 Manufacturing a Brave New World Newcastle University, 26th and 27th June 2018 Connected Everything's second annual conference was hosted by Newcastle University's School of Computing in its newest and smartest building - the Urban Sciences Building (USB). The 2018 conference brought together people from 41 institutions, including representatives from industry, Research Technology Organisations such as the HVM Catapult and TWI, and people from as far afield as the USA, Singapore, Australia and China. In total, 92 delegates spent two days enjoying presentations and stimulating discussions about the current challenges in digital manufacturing. 30 posters were on display in the atrium. The venue, USB, is part of Newcastle Helix, a unique urban development focused on research and innovation in tech businesses. The site has been built to serve as laboratories and act as an urban repository, with sensors around the city feeding data into the building. It could hardly have been a more fitting venue for the conference. This Special Issue of the Connected Everything Newsletter provides links to presenters' slides, which are given below in a sequence consistent with the conference proceedings. Available slides can also be viewed on the Connected Everything website, along with the conference programme, abstract booklet and the posters displayed at the event. We look forward to convening once again at Connected Everything's next annual conference, which will take place at the Jubilee Conference -
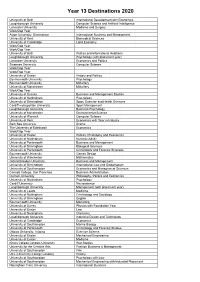
2020 Destinations
Year 13 Destinations 2020 University of Bath International Development with Economics Loughborough University Computer Science and Artificial Intelligence Lancaster University Medicine and Surgery Work/Gap Year Aston University, Birmingham International Business and Management University of Kent Biomedical Sciences University of Cambridge Land Economy Work/Gap Year Work/Gap Year University of Bath Politics and International Relations Loughborough University Psychology (with placement year) Lancaster University Economics and Politics Swansea University Computer Science Work/Gap Year Work/Gap Year University of Exeter History and Politics Bournemouth University Psychology Bournemouth University Midwifery University of Manchester Midwifery Work/Gap Year University of Sussex Business and Management Studies University of Nottingham Psychology University of Birmingham Sport, Exercise and Health Sciences Cardiff metropolitan University Sport Management Loughborough University Business Psychology University of Manchester Environmental Science University of Warwick Computer Science University of Kent Economics with Year in Industry Bath Spa University Drama The University of Edinburgh Economics Work/Gap Year University of Exeter Politics, Philosophy and Economics University of Nottingham Nursing (Adult) University of Portsmouth Business and Management University of Birmingham Biological Sciences University of Portsmouth Criminology and Forensic Sciences Bournemouth University Games Design University of Winchester Mathematics Oxford Brookes University -

CURRICULUM VITAE Dr Vivien Rolfe Bsc Phd FHEA MIBMS LEARNING
Curriculum Vitae, CC0 https://creativecommons.org/choose/zero/ CURRICULUM VITAE Dr Vivien Rolfe BSc PhD FHEA MIBMS Associate Head of Department of Biological, Biomedical and Analytical Science, UWE National Teaching Fellow (Higher Education Academy teaching excellence award, 2012) Learning Technologist of the Year (Association of Learning Technology, 2009) Principal Fellowship HEA (submitted for review July 2015) Twitter: @vivienrolfe Blog : vivrolfe.com Abbreviations: UWE = University of the West of England DMU = De Montfort University TEL = technology enhanced learning OER = open educational resources LEARNING AND TEACHING PROFILE I am a versatile academic with an international reputation in open education research and practice. I champion Learning and Teaching innovation and practice Nationally through being committee member of the Association of National Teaching Fellows, and also through working with the Association of Learning Technology (ALT), the Higher Education Academy (HEA) and Jisc. I closely follow Higher Education policy and participate in consultations and working groups. I am passionate about open education and have grown my research profiles at three UK universities. At De Montfort I led the academic community in enhancing their curricula and approaches through embedding open practice, and such work has had a sustained impact on staff and student experience several years on. Page 1 of 11 Curriculum Vitae, CC0 https://creativecommons.org/choose/zero/ EDUCATION AND EMPLOYMENT Aug 2013 - Associate Head of Department University -

Cardiff University International Prospectus 2021
Cardiff University International Prospectus 2021 www.cardiff.ac.uk/international www.cardiff.ac.uk/international bienvenue The photographs in this prospectus are of Cardiff University students, locations at Cardiff University and the city of Cardiff. studying at cardiff university www.cardiff.ac.uk/international welcome Cardiff University has been producing successful Contents graduates since 1883, combining a prestigious About Us heritage with modern and innovative facilities. 04 #WeAreInternational 06 Research The University has changed dramatically over the 08 Studying at Cardiff University last 137 years, but the 10 About Cardiff University commitment to quality 12 Career prospects education and a rewarding 14 Cardiff, the capital city of Wales university experience remains. 16 Accommodation 18 University life 20 The future Course List 21 Courses and Schools directory Enhancing Your Studies 42 Study Abroad 43 Global Opportunities 44 English Language Programme Next Steps 47 How to apply 49 Money and living expenses 50 University map 3 3 studying at cardiff university #WeAreInternational Cardiff University is truly international. With over 8,600 international students from more than 130 countries stepping through our doors each year, our student population is diverse and multicultural. We recruit worldwide for the best academic talent who help to deliver a rich and engaging study environment. The University reaches far beyond its home in Wales, with hundreds of overseas partnerships and research projects around the world, contributing to our ever-growing global community. University of Bremen Cardiff Carlos Jiminez Santillan, University * Mexico MSc Operational Research and Applied Statistics, 2018 Discovery Partners “Cardiff is such an amazing city to Institute (DPI) live in . -

Intelligent Mobility
@IMPETUS_UK ©SHUTTERSTOCK CONTACT US IMPETUS Innovate Research Technology Centre INTELLIGENT (Room B03) University Park Nottingham MOBILITY NG7 2RD Telephone: +44 (0)115 748 6068 THE OPTIMISED Email: [email protected] MOVEMENT www.nottingham.ac.uk/impetus OF GOODS AND PEOPLE © Copyright IMPETUS June 2016. All rights reserved. REF: 060616-V3.1 Contents About IMPETUS 4 PROSPECT – proactive safety for pedestrians and cyclists 6 “Encompassing everything from Estimating subsidence risk across an entire rail network from space 7 autonomous vehicles to seamless Telematics based predictive maintenance system for commercial vehicles 8 journey systems and multi-modal The effect of urban infrastructure on wireless network performance 10 modelling software, Intelligent Mobility uses emerging technologies Dynamic Modelling of Demand (D-MoD) 11 to enable the smarter, greener and Limits of the predictability of human travel 12 more efficient movement of people and goods around the world” Mapping obscuration of GNSS in urban landscapes (MOGUL) 13 PASSME (Personalised Airport Sytems for Seamless Mobility and Experience) 14 Transport Systems Catapult A Petri-Net modelling appraoch to railway bridge asset management 16 Variation of pollutant concentrations with road infrastructure interventions 17 Estimating public transport topology from existing supply data 18 Twitter and Passenger Disruption (TaPD) 19 Real time structural health monitoring 20 How the extremes of wireless network size affect data delivery 22 A Hansel and Gretel approach -

The University of Nottingham Ningbo, China Exchange Information Sheet 2014
The University of Nottingham Ningbo, China Exchange Information Sheet 2014 All study programmes are delivered entirely in English Friendly and vibrant international community from over 60 different countries Dedicated on campus International student support (including International Office, buddy system, guaranteed on campus accommodation etc.) Over 100 student societies and a range of cultural activities including weekend trips Free Chinese Language lessons for new international students Chance to travel and explore the vast array of history, beauty and entertainment in China Scholarship opportunities for international exchange students About UNNC The University of Nottingham Ningbo, China is the first Sino-Foreign University in China with approval from the Chinese Ministry of Education. The University of Nottingham Ningbo's mission statement is "Academic Excellence in the Service of Global Citizenship". All undergraduate and postgraduate programmes in Ningbo are conducted entirely in English with the same teaching and evaluation standards as at Nottingham UK by staff either seconded from Nottingham UK or appointed internationally to the University of Nottingham standards. The University is located in Ningbo Higher Education Park on a newly built and dedicated campus with a land area of 887mu. It currently has over 5400 undergraduate and postgraduate students and more than 600 teaching and administrative staff from over 40 countries in the world. Further information is available on: www.nottingham.edu.cn About Ningbo, China Located in the middle of China's coast (2.5 hours by bus from Shanghai), it is the cradle of the cultures in Yangtze River Delta and also a portal city equipped with modern port facilities and airport. -

SDAI Phase 3 Funded Projects
SDAI Phase 3 – funded projects The adequacy and optimality of retirement provision: household behaviour and the design of pensions Dr Cormac O’Dea, Institute for Fiscal Studies Email: [email protected] Prevalence and variation in antidepressant prescribing across Northern Ireland: a longitudinal administrative data linkage study for targeted support Professor Mark Shevlin, University of Ulster Email: [email protected] Technical change, employment and inequality. A spatial analysis of households and plant data Professor Maria Savona, University of Sussex Email: [email protected] The prevalence and persistence of ethnic and racial harassment and its impact on health: A longitudinal analysis Dr Alita Nandi, University of Essex Email: [email protected] Evaluating the use of contextual data in undergraduate admissions Dr Vikki Boliver, Durham University Email: [email protected] The taxation of human capital Mr Jonathan Shaw, Institute for Fiscal Studies Email: [email protected] Pathways to socio-economic and civic-political inclusion of ethnic minorities in Britain and Canada: The influence of family capital Dr Laurence Lessard-Phillips, University of Birmingham Email: [email protected] Which fathers are involved in looking after their children? Identifying the conditions associated with paternal involvement Dr Helen Norman, The University of Manchester Email: [email protected] Have socio-economic inequalities in childhood cognitive test scores changed? A secondary analysis of three British birth -

Opportunities for Language Learning – a Guide for Students and Parents
Opportunities for language learning – a guide for students and parents East Midlands Routes into Languages Consortium Opportunities at University Language skills are so important in the world we live in today and you don’t have to be fluent to experience the benefits – even knowing a little can go a long way and provide many opportunities for any future study and your career. Contents This booklet tells you all about the wide range of language opportunities Why languages? available to you at university. To enable you to access the information easily, Some facts and figures 1 these are split into those for single honours, combined and joint degrees, opportunities for beginners, short courses or modules and studying abroad Specialist Language Degrees 2 options. Please bear in mind, however, that these opportunities are often Combined and Joint Degrees 3 linked or overlap. You can also read about the experiences of students who have studied languages in different ways. Beginners 3 Short courses & modules 4 Also included are a number of specific examples of study options at universities in the East Midlands, which, if you are planning to study outside Which level is right for you 4 of the region, will still give you a good idea of what might be available at Studying or working universities you are interested in. The universities featured in this guide offer abroad options 5 a wide range of language provision in addition to the examples outlined, so check out their prospectuses or websites to find out more. You can also find Want to find out more? 6 full course listings on the UCAS (University and Colleges Admission Service) website www.ucas.com At the back of this booklet you will find a list of useful organisations and For further information and to receive sources of information. -

Challenging Existing Views of the Role of School Counsellors in the Kingdom of Saudi Arabia
Challenging Existing Views of the Role of School Counsellors in the Kingdom of Saudi Arabia Mr. Turki Aziz Mohammed Al Osaimi Al Otaibi Director of the Student Counselling Programme, The Education Department, Afif, Saudi Arabia PhD Candidate, The University of Nottingham, Nottingham, United Kingdom Research Paper Presentation 8th Annual Keele Counselling Conference 'Daring to Make an Impact: Dynamic Qualitative Research' 22nd - 23rd March 2014 Challenging Existing Views of the Role of School 22nd March 2014 1 Counsellors in the Kingdom of Saudi Arabia Background Overview of the Researcher EDUCATION • PhD in Education(School Counselling in the Kingdom of Saudi Arabia (KSA)) • The University of Nottingham • M. Sc. Degree in Educati onal Counselli ng and Psych ol ogy (With Merit) The University of Nottingham • B.Sc. in Social Sciences (With Distinction and Honor) • The College of Teacher Preparation in Makkah EMPLOYMENT • Director of the Student Counselling (2009- 2013) • Afif Education Department, KSA • Supervisor for Student Counselling (2003-2007) • Afif Education Department, KSA • Stud ent Counsell or (1996-2003) – Intermediate Secondary Schools (Afif) (2 years) – Secondary School (Afif) (6 years) – Primary School (Afif) (2 years) Challenging Existing Views of the Role of School 22nd March 2014 2 Counsellors in the Kingdom of Saudi Arabia Researcher’s Personal Positioning and Narrative “Many people measure success by how much money they have, or how many cars or houses they own. But for me, I measure success by the number of people I have been able to help in my life. My name is Turki Al Otaibi. I am the Director of the Student Counselling Programme at the Education Department in 'Afif', a city geographically located in central Saudi Arabia in the Najd region.