BRACHIAL PLEXUS ANATOMY, INJURIES and MANAGEMENT • Brachial Plexus Is Network of Nerves That Supply Sensation and Motor Function to Upper Extremity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anatomical Variations of the Brachial Plexus Terminal Branches in Ethiopian Cadavers
ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2017. Vol 6 (1): 896 – 905. ANATOMICAL VARIATIONS OF THE BRACHIAL PLEXUS TERMINAL BRANCHES IN ETHIOPIAN CADAVERS Edengenet Guday Demis*, Asegedeche Bekele* Corresponding Author: Edengenet Guday Demis, 196, University of Gondar, Gondar, Ethiopia. Email: [email protected] ABSTRACT Anatomical variations are clinically significant, but many are inadequately described or quantified. Variations in anatomy of the brachial plexus are important to surgeons and anesthesiologists performing surgical procedures in the neck, axilla and upper limb regions. It is also important for radiologists who interpret plain and computerized imaging and anatomists to teach anatomy. This study aimed to describe the anatomical variations of the terminal branches of brachial plexus on 20 Ethiopian cadavers. The cadavers were examined bilaterally for the terminal branches of brachial plexus. From the 40 sides studied for the terminal branches of the brachial plexus; 28 sides were found without variation, 10 sides were found with median nerve variation, 2 sides were found with musculocutaneous nerve variation and 2 sides were found with axillary nerve variation. We conclude that variation in the median nerve was more common than variations in other terminal branches. Key words: INTRODUCTION The brachial plexus is usually formed by the may occur (Moore and Dalley, 1992, Standring fusion of the anterior primary rami of the C5-8 et al., 2005). and T1 spinal nerves. It supplies the muscles of the back and the upper limb. The C5 and C6 fuse Most nerves in the upper limb arise from the to form the upper trunk, the C7 continues as the brachial plexus; it begins in the neck and extends middle trunk and the C8 and T1 join to form the into the axilla. -

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Study of Brachial Plexus with Regards to Its Formation, Branching Pattern and Variations and Possible Clinical Implications of Those Variations
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 4 Ver. VII (Apr. 2016), PP 23-28 www.iosrjournals.org Study of Brachial Plexus With Regards To Its Formation, Branching Pattern and Variations and Possible Clinical Implications of Those Variations. Dr. Shambhu Prasad1, Dr. Pankaj K Patel2 1 (Assistant Professor , Department of Anatomy , NMCH , Sasaram , India ) 2 (Assistant Professor , Department of Pathology , NMCH , Sasaram , India ) Abstract: Aim of the study: to search variations in formation and branching pattern of brachial plexus and correlate them with possible clinical and surgical implications. Materials and Methods: 25human bodies were dissected for this study. Dissection was started in posterior triangle of neck and extended to distal part of upper limb passing through axilla . Photographs were taken and data was tabulated and analyzed . Observations: All 50 plexuses had origin from C5 – T1 . Dorsal scapular nerve was absent in 2 plexuses. Long thoracic nerve was made of C5,C6 fibers in one and of C6,C7 fibers in another . Lower trunk was abnormal in 2 plexuses both of same body, their was no contribution from T1 fibers to posterior cord in one of these plexus. One plexus had double lateral pectoral nerve , communication between lateral and medial pectoral nerves , lateral pectoral and medial root of median nerve also between musculocutaneous and lateral root of median nerve . 2 more plexuses had communication between lateral and medial pectoral nerves. One plexus showed 2 branches coming from posterior division of upper trunk itself before formation of posterior cord. -

Bilateral Presence of a Variant Subscapularis Muscle
CASE REPORT Bilateral presence of a variant subscapularis muscle Krause DA and Youdas JW Krause DA, Youdas JW. Bilateral presence of a variant subscapularis the lateral subscapularis inserting into the proximal humerus with the tendon of muscle. Int J Anat Var. 2017;10(4):79-80. the subscapularis. The axillary and lower subscapular nerves coursed between the observed muscle and the subscapularis. The presence of the muscle has potential ABSTRACT to entrap the axillary nerve and the lower subscapular nerve. We describe the presence of an accessory subscapularis muscle observed bilaterally Key Words: Accessory subscapularis; Axillary nerve; Lower subscapular nerve; in a human anatomy laboratory. The muscle originated from the mid-region of Entrapment INTRODUCTION everal anatomic variations in axillary musculature have been reported (1- S4). One of the more common variations is the axillary arch muscle, also known as Langer’s muscle, the axillopectoral muscle, and the pectordorsal muscle (3,4). This muscle typically arises from the lateral aspect of the latissimus dorsi inserting deep to the pectoralis major on the humerus. Several variations of the axillary arch muscle are described with a reported incidence of 6-9% (4-6). Less frequent and distinctly different than the axillary arch muscle, is a variant muscle associated with the subscapularis. This has been termed the subscapulo-humeral muscle, subscapularis minor, subscapularis-teres-latissimus muscle, and the accessory subcapularis muscle (1,2,7). Reported incidence ranges from 0.45 to 2.6% (2,7). CASE REPORT A variant muscle associated with the subscapularis bilaterally was observed on a Caucasian female embalmed cadaver during routine dissection in a human anatomy class for first year physical therapy students. -
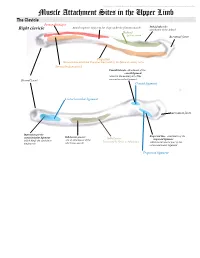
Muscle Attachment Sites in the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Muscle Attachment Sites in the Upper Limb The Clavicle Pectoralis major Smooth superior surface of the shaft, under the platysma muscle Deltoid tubercle: Right clavicle attachment of the deltoid Deltoid Axillary nerve Acromial facet Trapezius Sternocleidomastoid and Trapezius innervated by the Spinal Accessory nerve Sternocleidomastoid Conoid tubercle, attachment of the conoid ligament which is the medial part of the Sternal facet coracoclavicular ligament Conoid ligament Costoclavicular ligament Acromial facet Impression for the Trapezoid line, attachment of the costoclavicular ligament Subclavian groove: Subclavius trapezoid ligament which binds the clavicle to site of attachment of the Innervated by Nerve to Subclavius which is the lateral part of the the first rib subclavius muscle coracoclavicular ligament Trapezoid ligament This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. The Scapula Trapezius Right scapula: posterior Levator scapulae Supraspinatus Deltoid Deltoid and Teres Minor are innervated by the Axillary nerve Rhomboid minor Levator Scapulae, Rhomboid minor and Rhomboid Major are innervated by the Dorsal Scapular Nerve Supraspinatus and Infraspinatus innervated by the Suprascapular nerve Infraspinatus Long head of triceps Rhomboid major Teres Minor Teres Major Teres Major -
Brachial Plexus Injury Investigation , Localization and Treatment
BRACHIAL PLEXUS INJURY INVESTIGATION , LOCALIZATION AND TREATMENT EMBRYOLOGY § Brachial plexus (BP) is developed at 5 weeks of gestation § Afferent fibers develop from neuroblast located alongside neural tube § Efferent fibers originate from neuroblast in the basal plate of tube from where they grow outside § Afferent and efferent fibers join to form the nerve § Nerves divide into anterior and posterior divisions § There are connections between these nerves in the brachial plexus commons.wikimedia.org/wiki/File:Brachial_plexus.jpg ANATOMY lFormed by ventral primary rami of lower four cervical and first thoracic nerve root. l Frequently have contributions from C4(pre-fixed) or T2 (post-fixed). PREFIXED BRACHIAL PLEXUS http://www.msdlatinamerica.com/ebooks/HandSurgery/sid744608.html Post-fixed plexus http://www.msdlatinamerica.com/ebooks/HandSurgery/sid744608.html RELATIONS OF BRACHIAL PLEXUS Fig. 4. The reIationship of the axillary artery to the cords is an important anatomic relationship. The cords surround the axiIIary artery and are named for their position with respect to the axillary artery. L.C. lateral cord MC. Medial cord: PC . posterior Cord. Levels § Roots § Real § Trunks § Texans § Divisions § Drink § Cords § Cold § Branches § Beer § C5 and C6 roots form upper trunk § C8 and T1 roots the lower trunk § C7 forms the middle trunk § Joining point of C5-C6 roots is ERB”S POINT § Each trunk divides into an anterior and a posterior division and passes beneath the clavicle § All 3 posterior divisions merge to form the posterior cord § Anterior division of the upper and middle trunk merge to form the lateral cord § Anterior division of lower trunk forms the medial cord § Lateral cord splits into 2 terminal branches: a) Musculocutaneous nerve b) Lateral cord contribution to median nerve (sensory) § Posterior cord splits into a)axillary nerve and b)radial nerve § Medial cord gives off a) medial cord contribution to the median nerve(motor) and b)ulnar nerve § There are few terminal branches of the roots trunks and cords. -

Examination of the Shoulder Bruce S
Examination of the Shoulder Bruce S. Wolock, MD Towson Orthopaedic Associates 3 Joints, 1 Articulation 1. Sternoclavicular 2. Acromioclavicular 3. Glenohumeral 4. Scapulothoracic AC Separation Bony Landmarks 1. Suprasternal notch 2. Sternoclavicular joint 3. Coracoid 4. Acromioclavicular joint 5. Acromion 6. Greater tuberosity of the humerus 7. Bicipital groove 8. Scapular spine 9. Scapular borders-vertebral and lateral Sternoclavicular Dislocation Soft Tissues 1. Rotator Cuff 2. Subacromial bursa 3. Axilla 4. Muscles: a. Sternocleidomastoid b. Pectoralis major c. Biceps d. Deltoid Congenital Absence of Pectoralis Major Pectoralis Major Rupture Soft Tissues (con’t) e. Trapezius f. Rhomboid major and minor g. Latissimus dorsi h. Serratus anterior Range of Motion: Active and Passive 1. Abduction - 90 degrees 2. Adduction - 45 degrees 3. Extension - 45 degrees 4. Flexion - 180 degrees 5. Internal rotation – 90 degrees 6. External rotation – 45 degrees Muscle Testing 1. Flexion a. Primary - Anterior deltoid (axillary nerve, C5) - Coracobrachialis (musculocutaneous nerve, C5/6 b. Secondary - Pectoralis major - Biceps Biceps Rupture- Longhead Muscle Testing 2. Extension a. Primary - Latissimus dorsi (thoracodorsal nerve, C6/8) - Teres major (lower subscapular nerve, C5/6) - Posterior deltoid (axillary nerve, C5/6) b. Secondary - Teres minor - Triceps Abduction Primary a. Middle deltoid (axillary nerve, C5/6) b. Supraspinatus (suprascapular nerve, C5/6) Secondary a. Anterior and posterior deltoid b. Serratus anterior Deltoid Ruputure Axillary Nerve Palsy Adduction Primary a. Pectoralis major (medial and lateral pectoral nerves, C5-T1 b. Latissimus dorsi (thoracodorsal nerve, C6/8) Secondary a. Teres major b. Anterior deltoid External Rotation Primary a. Infraspinatus (suprascapular nerve, C5/6) b. Teres minor (axillary nerve, C5) Secondary a. -

Pectoral Nerves – a Third Nerve and Clinical Implications Kleehammer, A.C., Davidson, K.B., and Thompson, B.J
Pectoral Nerves – A Third Nerve and Clinical Implications Kleehammer, A.C., Davidson, K.B., and Thompson, B.J. Department of Anatomy, DeBusk College of Osteopathic Medicine, Lincoln Memorial University Introduction Summary Table 1. Initial Dataset and Observations The textbook description of the pectoral nerves A describes a medial and lateral pectoral nerve arising A from the medial and lateral cords, respectively, to innervate the pectoralis major and minor muscles. Studies have described variations in the origins and branching of the pectoral nerves and even in the muscles they innervate (Porzionato et al., 2011, Larionov et al., 2020). There have also been reports of three pectoral nerves with distinct origins (Aszmann et Table 1: Initial Dataset and Observations Our initial dataset consisted of 31 anatomical donors, dissected bilaterally, Each side was considered an al., 2000) and variability of the spinal nerve fibers Independent observation. Of the 62 brachial plexuses, 50 met our inclusion criteria. contributing to these nerves (Lee, 2007). Given the Table 2. Branching Patterns of Pectoral Nerves frequency of reported variation from the textbook description, reexamining the origin, course and B branching of the pectoral nerves could prove useful for B students and clinicians alike. The pectoral nerves are implicated in a variety of cases including surgeries of the breast, pectoral, and axillary region (David et al., 2012). Additionally, the lateral pectoral nerve has recently gained attention for potential use as a nerve graft for other damaged nerves such as the spinal accessory nerve (Maldonado, et al., 2017). The objective of this study was to assess the frequency and patterns of pectoral nerve branching in order to more accurately describe their orientation and implications in clinical cases. -

Brachial Plexus Posterior Cord Variability: a Case Report and Review
CASE REPORT Brachial plexus posterior cord variability: a case report and review Edward O, Arachchi A, Christopher B Edward O, Arachchi A, Christopher B. Brachial plexus posterior cord anatomical variability. This case report details the anatomical variants discovered variability: a case report and review. Int J Anat Var. 2017;10(3):49-50. in the posterior cord of the brachial plexus in a routine cadaveric dissection at the University of Melbourne, Australia. Similar findings in the literature are reviewed ABSTRACT and the clinical significance of these findings is discussed. The formation and distribution of the brachial plexus is a source of great Key Words: Brachial plexus; Posterior cord; Axillary nerve; Anatomical variation INTRODUCTION he brachial plexus is the neural network that supplies motor and sensory Tinnervation to the upper limb. It is typically composed of anterior rami from C5 to T1 spinal segments, which subsequently unite to form superior, middle and inferior trunks. These trunks divide and reunite to form cords 1 surrounding the axillary artery, which terminate in branches of the plexus. The posterior cord is classically described as a union of the posterior divisions from the superior, middle and inferior trunks of the brachial plexus, with fibres from all five spinal segments. The upper subscapular, thoracodorsal and lower subscapular nerves propagate from the cord prior to the axillary and radial nerves forming terminal branches. Variability in the brachial plexus is frequently reported in the literature. It is C5 nerve root Suprascapular nerve important for clinicians to be aware of possible variations when considering Posterior division of C5-C6 injuries or disease of the upper limb. -

Axilla & Brachial Plexus
Anatomy Guy Dissection Sheet Axilla & Brachial Plexus Dr. Craig Goodmurphy Anatomy Guy Major Dissection Objectives 1. Review some of the superficial veins and nerves and extrapolate skin incisions down the arm while sparing the cephalic and basilic veins 2. Secure the upper limb in an abducted position and review the borders of the axilla while reflecting pec major and minor. 3. You may need to remove the middle third of the clavicle with bone cutters or oscillating saw 4. Identify and open the axillary sheath to find the axillary vein and separate it away from the arteries and nerves 5. Once it is mobilized remove smaller veins and reflect the axillary vein medially Major Dissection Objectives Arteries 6. Locate and clean the subclavian artery as it becomes the axillary a. at the first rib. 7. Identifying part 1, 2 and 3 of the axillary artery as they relate to pectoralis minor 8. Identify & clean the thoracoacromial trunk and its branches along with the lateral thoracic artery 9. Clean the subscapular artery and follow it to the circumflex scapular and thoracodorsal branches removing the fat of the region and noting variations and lymph nodes that may be present. 10. Locate the posterior and anterior humeral circumflex arteries and the brachial artery Eastern Virginia Medical School 1 Anatomy Guy Dissection Sheet Axilla & Brachial Plexus Major Dissection Objectives Nerves 11. Review the parts of the brachial plexus with roots in the scalene gap, trunks superior to the clavicle, divisions posterior to the clavicle, cords and branches inferior to the clavicle. 12. Locate the musculocutaneous nerve laterally as it pierces the coracobrachialis m. -
Pectoral Region and Axilla Doctors Notes Notes/Extra Explanation Editing File Objectives
Color Code Important Pectoral Region and Axilla Doctors Notes Notes/Extra explanation Editing File Objectives By the end of the lecture the students should be able to : Identify and describe the muscles of the pectoral region. I. Pectoralis major. II. Pectoralis minor. III. Subclavius. IV. Serratus anterior. Describe and demonstrate the boundaries and contents of the axilla. Describe the formation of the brachial plexus and its branches. The movements of the upper limb Note: differentiate between the different regions Flexion & extension of Flexion & extension of Flexion & extension of wrist = hand elbow = forearm shoulder = arm = humerus I. Pectoralis Major Origin 2 heads Clavicular head: From Medial ½ of the front of the clavicle. Sternocostal head: From; Sternum. Upper 6 costal cartilages. Aponeurosis of the external oblique muscle. Insertion Lateral lip of bicipital groove (humerus)* Costal cartilage (hyaline Nerve Supply Medial & lateral pectoral nerves. cartilage that connects the ribs to the sternum) Action Adduction and medial rotation of the arm. Recall what we took in foundation: Only the clavicular head helps in flexion of arm Muscles are attached to bones / (shoulder). ligaments / cartilage by 1) tendons * 3 muscles are attached at the bicipital groove: 2) aponeurosis Latissimus dorsi, pectoral major, teres major 3) raphe Extra Extra picture for understanding II. Pectoralis Minor Origin From 3rd ,4th, & 5th ribs close to their costal cartilages. Insertion Coracoid process (scapula)* 3 Nerve Supply Medial pectoral nerve. 4 Action 1. Depression of the shoulder. 5 2. Draw the ribs upward and outwards during deep inspiration. *Don’t confuse the coracoid process on the scapula with the coronoid process on the ulna Extra III. -

Axillary Nerve Injury Associated with Sports
Neurosurg Focus 31 (5):E10, 2011 Axillary nerve injury associated with sports SANGKOOK LEE, M.D.,1 KRIANGSAK SAETIA, M.D.,2 SUPARNA SAHA, M.D.,1 DAVID G. KLINE, M.D.,3 AND DANIEL H. KIM, M.D.1 1Department of Neurosurgery, Baylor College of Medicine, Houston, Texas; 2Division of Neurosurgery, Department of Surgery, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; and 3Department of Neurosurgery, Louisiana State University Health Sciences Center, New Orleans, Louisiana Object. The aim of this retrospective study was to present and investigate axillary nerve injuries associated with sports. Methods. This study retrospectively reviewed 26 axillary nerve injuries associated with sports between the years 1985 and 2010. Preoperative status of the axillary nerve was evaluated by using the Louisiana State University Health Science Center (LSUHSC) grading system published by the senior authors. Intraoperative nerve action potential recordings were performed to check nerve conduction and assess the possibility of resection. Neurolysis, suture, and nerve grafts were used for the surgical repair of the injured nerves. In 9 patients with partial loss of function and 3 with complete loss, neurolysis based on nerve action potential recordings was the primary treatment. Two patients with complete loss of function were treated with resection and suturing and 12 with resection and nerve grafting. The minimum follow-up period was 16 months (mean 20 months). Results. The injuries were associated with the following sports: skiing (12 cases), football (5), rugby (2), base- ball (2), ice hockey (2), soccer (1), weightlifting (1), and wrestling (1). Functional recovery was excellent. Neurolysis was performed in 9 cases, resulting in an average functional recovery of LSUHSC Grade 4.2.