Effect of Standard Treatment Guidelines with Or Without
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fire and Other Health and Safety Incidents in the Bangladesh Garment Sector November 2012-March 2018
Fire and Other Health and Safety Incidents in the Bangladesh Garment Sector November 2012-March 2018 5,178 worker injuries and deaths (3,875 injuries; 1,303 deaths) Safety Factory Incident Incidents Name Location Date Injuries Deaths Cause/Outcome Description 1 Tazreen 252, 253 & 258, 11/24/12 200 112 The fire, presumably caused by a short circuit, started on the ground floor of the nine-story factory, trapping the Fashions Ltd. Monoshontuspur, workers on the floors above. Because of the large amount of fabric and yarn in the factory, the fire was able to Nishenantopur, quickly spread to other floors, complicating the firefighting operations. The fire burned for more than seventeen Ashulia hours before the firefighters were successful in extinguishing it. http://www.shahidulnews.com/bangladesh-textile- factory-fire-leaves-more-than-100-dead 2 Swan Dakkin 11/26/12 0 1 The fire originated from the warehouse of Swan Garments Ltd on the 1st floor of Afnan Plaza at Mollartek around Garments Ltd Khan,Uttara, 9:30am. It was doused around 12:00 noon after hectic efforts by 13 firefighting units. Dhaka Except for the second floor, the blaze could not spread through the building. Some workers sustained minor injuries as they rushed to the main staircase to get out of the building. Bundles of threads and clothes kept in the warehouse were also gutted. 3 Al-Shahriar Palashbari, 11/27/12 0 0 Fire might have originated from an electrical short circuit at the warehouse. Fabrics was burnt. No Injury Fabric Ltd. Ashulia 4 Section Seven Chittagong EPZ 11/28/12 50 0 Power generator of the factory caught fire due to a mechanical glitch. -
Bangladesh, Year 2019: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED)
BANGLADESH, YEAR 2019: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 29 June 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015b; administrative divisions: GADM, November 2015a; China/India border status: CIA, 2006; geodata of disputed borders: GADM, November 2015b; Natural Earth, undated; incident data: ACLED, 20 June 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 BANGLADESH, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 29 JUNE 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Protests 930 1 1 Conflict incidents by category 2 Riots 405 107 122 Development of conflict incidents from 2010 to 2019 2 Violence against civilians 257 184 195 Battles 99 43 63 Methodology 3 Strategic developments 15 0 0 Conflict incidents per province 4 Explosions / Remote 7 2 2 violence Localization of conflict incidents 4 Total 1713 337 383 Disclaimer 6 This table is based on data from ACLED (datasets used: ACLED, 20 June 2020). Development of conflict incidents from 2010 to 2019 This graph is based on data from ACLED (datasets used: ACLED, 20 June 2020). 2 BANGLADESH, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 29 JUNE 2020 Methodology GADM. Incidents that could not be located are ignored. -

Psychosocial Wellbeing of the LGBTIQ+ Community in Bangladesh
BRAC JPGSPH COVID-19 individuals who live in their own communities criminalizing same-sex activities under the Bangladesh RESEARCH REPORT structured by a well-defined guru-chela12 structure. Penal Code (BPC 377), which carries a maximum Transgender women and men in this research are not sentence of 10 years in prison. part of any guru-chela structure and hence are not part of the hijra community or the profession of hijragiri, The last decade observed several initiatives by LGBTQ and hence do not identify as hijras. 1 participant activist groups, and organizations working in sexual identified as ‘Koti’13 a localized expression for gender and reproductive health and rights (SRHR) and law to variant identity which does not find a place within the further the rights of individuals with diverse universal English acronym LGBTIQ+, which shows that sexualities, genders, and sex characteristics. the acronym does not always fully represent the Particularly between the years 2014-2016, several various identities situated in specific geographies. We visible activist works such as printing of a magazine, chose to keep terms/labels that the participants used rainbow rally, a lesbian comic flashcard and queer to describe their identities without imposing other theatre production made it into the public domain. interpretation or any kind of judgement. Such visible forms of activism however came to a sudden halt in 2016, after the brutal killings of queer The Impact of COVID-19 activists Xulhaz Mannan and Mahbub Rabbi Tonoy by INFORMED CONSENT AND Ansar Al-Islam militants. Having had experienced ETHICS instability, disconnections, relative hiatus, and a real sense of threat for one’s life, LGBTIQ+ activists have on the Psychosocial Wellbeing started to resume organizing in safe and discreet Participants were fully explained the purpose and manner once again. -

Checklist of the Pteridophytes of Narsingdi District, Bangladesh
Jahangirnagar University J. Biol. Sci. 8(2): 13-24, 2019 (December) Checklist of the pteridophytes of Narsingdi District, Bangladesh Robayda Khanam, Saleh Ahammad Khan and Mohammod Abdur Rahim Plant Systematics and Biodiversity Laboratory, Department of Botany, Jahangirnagar University, Savar, Dhaka-1342, Bangladesh Abstract The occurrence of a total of 31 species of pteridophytes under 20 genera and 13 families in Narsingdi district were confirmed. Pteridaceae with 11 species was found as the largest family, which was followed by Salviniaceae and Polypodiaceae consisted of four species each and Thelypteridaceae with three species. Each of the rest nine families was represented by only one species. Pteris with six species was found as the largest genus, which was followed by Salvinia with three species, and Adiantum, Ceratopteris, Pyrrosia and Cyclosorus with two species each. Each of the rest 14 genera was represented by only one species. Among these species, 21 were found as terrestrial, two as both terrestrial and semiaquatic, four as aquatic and other four as epiphytic. The occurrence of Tectaria chattagrammica Ching, listed as DD (Data Deficient) in Red Data Book of Bangladesh, was common with natural regeneration in this district. Key words: Checklist, Pteridophyte, Narsingdi district, Bangladesh. INTRODUCTION Pteridophytes or the ferns and fern-allies are the most primitive vascular plants in the plant world. They were a major part of the earth’s luxuriant vegetation during the Carboniferous period (The Columbia Electronic Encyclopedia, 2012). In the modern era, the pteridophytes are an important component of the flora of any area. They have been used as ornamentals and medicinals (Nayar, 1957; Benerjee & Sen, 1980; Dhiman, 1998; Dixit, 1974 and 1975; Hodge, 1973; Kaushik, 1998; Singh, et al., 1989; Benjamin & Manickam, 2007; Kavitha et al., 2017; Singh & Rajkumar, 2017). -

Division Name District Name Upazila Name 1 Dhaka 1 Dhaka 1 Dhamrai 2 Dohar 3 Keraniganj 4 Nawabganj 5 Savar
Division name District Name Upazila Name 1 Dhaka 1 Dhamrai 1 Dhaka 2 Dohar 3 Keraniganj 4 Nawabganj 5 Savar 2 Faridpur 1 Alfadanga 2 Bhanga 3 Boalmari 4 Char Bhadrasan 5 Faridpur Sadar 6 Madhukhali 7 Nagarkanda 8 Sadarpur 9 Saltha 3 Gazipur 1 Gazipur Sadar 2 Kaliakoir 3 Kaliganj 4 Kapasia 5 Sreepur 4 Gopalganj 1 Gopalganj Sadar 2 Kasiani 3 Kotalipara 4 Maksudpur 5 Tungipara 5 Jamalpur 1 Bakshiganj 2 Dewanganj 3 Islampur 4 Jamalpur Sadar 5 Madarganj 6 Melandah 7 Sharishabari 6 Kishoreganj 1 Austogram 2 Bajitpur 3 Bhairab 4 Hosainpur 5 Itna 6 Karimganj 7 Katiadi 8 Kishoreganj Sadar 9 Kuliarchar 10 Mithamain 11 Nikli 12 Pakundia 13 Tarail 7 Madaripur 1 Kalkini 2 Madaripur Sadar 3 Rajoir 4 Shibchar 8 Manikganj 1 Daulatpur 2 Ghior 3 Harirampur 4 Manikganj Sadar 5 Saturia 6 Shibalaya 7 Singair 9 Munshiganj 1 Gazaria 2 Lauhajang 3 Munshiganj Sadar 4 Serajdikhan 5 Sreenagar 6 Tangibari 10 Mymensingh 1 Bhaluka 2 Dhubaura 3 Fulbaria 4 Fulpur 5 Goffargaon 6 Gouripur 7 Haluaghat 8 Iswarganj 9 Mymensingh Sadar 10 Muktagacha 11 Nandail 12 Trishal 11 Narayanganj 1 Araihazar 2 Bandar 3 Narayanganj Sadar 4 Rupganj 5 Sonargaon 12 Norshingdi 1 Belabo 2 Monohardi 3 Norshingdi Sadar 4 Palash 5 Raipura 6 Shibpur 13 Netrokona 1 Atpara 2 Barhatta 3 Durgapur 4 Kalmakanda 5 Kendua 6 Khaliajuri 7 Madan 8 Mohanganj 9 Netrokona Sadar 10 Purbadhala 14 Rajbari 1 Baliakandi 2 Goalunda 3 Pangsha 4 Rajbari Sadar 5 Kalukhale 15 Shariatpur 1 Bhedarganj 2 Damudiya 3 Gosairhat 4 Zajira 5 Naria 6 Shariatpur Sadar 16 Sherpur 1 Jhenaigati 2 Nakla 3 Nalitabari 4 Sherpur Sadar -

Leaf Epidermal Anatomy of Cynodon Dactylon (L.) Pers
Bangladesh J. Plant Taxon. 28(1): 171‒193, 2021 (June) https://doi.org/10.3329/bjpt.v28i1.54216 © 2021 Bangladesh Association of Plant Taxonomists LEAF EPIDERMAL ANATOMY OF CYNODON DACTYLON (L.) PERS. IN RELATION TO ECOTYPIC ADAPTATION 1,2 3 1 S.K. NITU , H. TARIQUE AND S.M.S. ISLAM * Plant Biotechnology and Genetic Engineering Lab., Institute of Biological Sciences, University of Rajshahi, Rajshahi-6205, Bangladesh Keywords: Anatomy; Cynodon dactylon; Leaf epidermis; Stomatal features. Abstract Qualitative and quantitative studies were done on leaf epidermal characteristics with special reference to stomatal features to find out the impact of environmental condition on twenty four accessions of Cynodon dactylon (L.) Pers. collected from different ecological habitats of Bangladesh. The foliar epidermal peels from both surfaces of mature leaves were observed under microscope. The leaves were found to be amphistomatic and stomata were paracytic type. The epidermal cells in this study were found to be sinuous. Silica bodies were found to be saddle and cross shaped. Prickles angular were pointed at the tip. Macro-hairs were present in all the accessions, but no micro-hair was found both adaxially or abaxially. Stomatal frequency and stomatal index were found to vary from accession to accession on both adaxial and abaxial surface of leaves, and the differences were statistically significant in most of the cases. Introduction Cynodon dactylon (L.) Pers is a typical warm season turfgrass belongs to the family of Poaceae and this grass species is widely adapted to various environments of tropical and sub- tropical regions around the world. There are some ways for genetic diversity and population structure analysis of C. -

Quantification of Pesticide Residues in Fresh Vegetables Available
agronomy Article Quantification of Pesticide Residues in Fresh Vegetables Available in Local Markets for Human Consumption and the Associated Health Risks Umme Salma Nisha 1, Md. Sirajul Islam Khan 1,* , Mohammad Dalower Hossain Prodhan 2 , Islam Md Meftaul 1,3,* , Noorjahan Begum 1, Aney Parven 1,3, Syfullah Shahriar 3, Abdul Shukor Juraimi 4 and Md. Abdul Hakim 5 1 Department of Agricultural Chemistry, Sher-e-Bangla Agricultural University, Dhaka 1207, Bangladesh; [email protected] (U.S.N.); [email protected] (N.B.); [email protected] (A.P.) 2 Pesticide Research & Environmental Toxicology Section, Entomology Division, Bangladesh Agricultural Research Institute, Gazipur 1701, Bangladesh; [email protected] 3 Global Centre for Environmental Remediation (GCER), College of Engineering, Science and Environment, The University of Newcastle, Callaghan, NSW 2308, Australia; [email protected] 4 Faculty of Agriculture, Universiti Putra Malaysia, Serdang 43400, Malaysia; [email protected] 5 Department of Agricultural Chemistry, Hajee Mohammad Danesh Science and Technology University, Dinajpur 5200, Bangladesh; [email protected] * Correspondence: [email protected] (M.S.I.K.); [email protected] (I.M.M.) Abstract: Human health risks as a result of consuming pesticide residues in fresh vegetables have drawn serious attention to the scientific community, particularly in developing countries. This study Citation: Nisha, U.S.; Khan, M.S.I.; analyzed country bean (Lablab purpureus L.) and eggplant (Solanum melongena L.) for widely used Prodhan, M.D.H.; Meftaul, I.M.; neonicotinoid, synthetic pyrethroid, and dithiocarbamate pesticide residues in order to ensure food Begum, N.; Parven, A.; Shahriar, S.; safety. -
Download File
Cover and section photo credits Cover Photo: “Untitled” by Nurus Salam is licensed under CC BY-SA 2.0 (Shangu River, Bangladesh). https://www.flickr.com/photos/nurus_salam_aupi/5636388590 Country Overview Section Photo: “village boy rowing a boat” by Nasir Khan is licensed under CC BY-SA 2.0. https://www.flickr.com/photos/nasir-khan/7905217802 Disaster Overview Section Photo: Bangladesh firefighters train on collaborative search and rescue operations with the Bangladesh Armed Forces Division at the 2013 Pacific Resilience Disaster Response Exercise & Exchange (DREE) in Dhaka, Bangladesh. https://www.flickr.com/photos/oregonmildep/11856561605 Organizational Structure for Disaster Management Section Photo: “IMG_1313” Oregon National Guard. State Partnership Program. Photo by CW3 Devin Wickenhagen is licensed under CC BY 2.0. https://www.flickr.com/photos/oregonmildep/14573679193 Infrastructure Section Photo: “River scene in Bangladesh, 2008 Photo: AusAID” Department of Foreign Affairs and Trade (DFAT) is licensed under CC BY 2.0. https://www.flickr.com/photos/dfataustralianaid/10717349593/ Health Section Photo: “Arsenic safe village-woman at handpump” by REACH: Improving water security for the poor is licensed under CC BY 2.0. https://www.flickr.com/photos/reachwater/18269723728 Women, Peace, and Security Section Photo: “Taroni’s wife, Baby Shikari” USAID Bangladesh photo by Morgana Wingard. https://www.flickr.com/photos/usaid_bangladesh/27833327015/ Conclusion Section Photo: “A fisherman and the crow” by Adnan Islam is licensed under CC BY 2.0. Dhaka, Bangladesh. https://www.flickr.com/photos/adnanbangladesh/543688968 Appendices Section Photo: “Water Works Road” in Dhaka, Bangladesh by David Stanley is licensed under CC BY 2.0. -
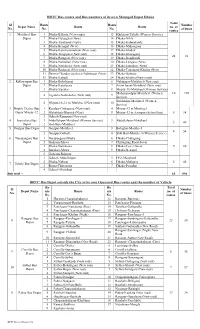
BRTC Bus Routes and Bus Numbers of Its Own Managed Depot Dhaka Total Sl Routs Routs Number Depot Name Routs Routs No
BRTC Bus routes and Bus numbers of its own Managed Depot Dhaka Total Sl Routs Routs Number Depot Name Routs Routs no. of No. No. No. of buses routes 1. Motijheel Bus 1 Dhaka-B.Baria (New routs) 13 Khilgoan-Taltola (Women Service) Depot 2 Dhaka-Haluaghat (New) 14 Dhaka-Nikli 3 Dhaka-Tarakandi (New) 15 Dhaka-Kalmakanda 4 Dhaka-Benapul (New) 16 Dhaka-Muhongonj 5 Dhaka-Kutichowmuhoni (New rout) 17 Dhaka-Modon 6 Dhaka-Tongipara (New rout) 18 Dhaka-Ishoregonj 24 82 7 Dhaka-Ramgonj (New rout) 19 Dhaka-Daudkandi 8 Dhaka-Nalitabari (New rout) 20 Dhaka-Lengura (New) 9 Dhaka-Netrakona (New rout) 21 Dhaka-Jamalpur (New) 10 Dhaka-Ramgonj (New rout) 22 Dhaka-Tongipara-Khulna (New) 11 Demra-Chandra via Savar Nabinagar (New) 23 Dhaka-Bajitpur 12 Dhaka-Katiadi 24 Dhaka-Khulna (New routs) 2. Kallayanpur Bus 1 Dhaka-Bokshigonj 6 Nabinagar-Motijheel (New rout) Depot 2 Dhaka-Kutalipara 7 Zirani bazar-Motijheel (New rout) 3 Dhaka-Sapahar 8 Mirpur-10-Motijheel (Women Service) Mohammadpur-Motijheel (Women 10 198 4 Zigatola-Notunbazar (New rout) 9 Service) Siriakhana-Motijheel (Women 5 Mirpur-10-2-1 to Motijheel (New rout) 10 Service) 3. Double Decker Bus 1 Kendua-Chittagong (New rout) 4 Mirpur-12 to Motijheel Depot Mirpur-12 2 Mohakhali-Bhairob (New) 5 Mirpur-12 to Azimpur (School bus) 5 38 3 Gabtoli-Rampura (New rout) 4. Joarsahara Bus 1 Abdullahpur-Motijheel (Women Service) 3 Abdullahpur-Motijheel 5 49 Depot 2 Shib Bari-Motijheel 5. Gazipur Bus Depot 1 Gazipur-Motijheel 3 Balughat-Motijheel 4 54 2 Gazipur-Gabtoli 4 Shib Bari-Motijheel (Women Service) 6. -
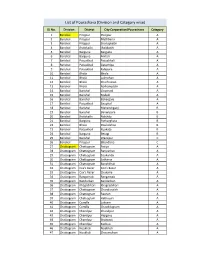
List of Pourashava (Division and Category Wise)
List of Pourashava (Division and Category wise) SL No. Division District City Corporation/Pourashava Category 1 Barishal Pirojpur Pirojpur A 2 Barishal Pirojpur Mathbaria A 3 Barishal Pirojpur Shorupkathi A 4 Barishal Jhalokathi Jhalakathi A 5 Barishal Barguna Barguna A 6 Barishal Barguna Amtali A 7 Barishal Patuakhali Patuakhali A 8 Barishal Patuakhali Galachipa A 9 Barishal Patuakhali Kalapara A 10 Barishal Bhola Bhola A 11 Barishal Bhola Lalmohan A 12 Barishal Bhola Charfession A 13 Barishal Bhola Borhanuddin A 14 Barishal Barishal Gournadi A 15 Barishal Barishal Muladi A 16 Barishal Barishal Bakerganj A 17 Barishal Patuakhali Bauphal A 18 Barishal Barishal Mehendiganj B 19 Barishal Barishal Banaripara B 20 Barishal Jhalokathi Nalchity B 21 Barishal Barguna Patharghata B 22 Barishal Bhola Doulatkhan B 23 Barishal Patuakhali Kuakata B 24 Barishal Barguna Betagi B 25 Barishal Barishal Wazirpur C 26 Barishal Pirojpur Bhandaria C 27 Chattogram Chattogram Patiya A 28 Chattogram Chattogram Bariyarhat A 29 Chattogram Chattogram Sitakunda A 30 Chattogram Chattogram Satkania A 31 Chattogram Chattogram Banshkhali A 32 Chattogram Cox's Bazar Cox’s Bazar A 33 Chattogram Cox's Bazar Chakaria A 34 Chattogram Rangamati Rangamati A 35 Chattogram Bandarban Bandarban A 36 Chattogram Khagrchhari Khagrachhari A 37 Chattogram Chattogram Chandanaish A 38 Chattogram Chattogram Raozan A 39 Chattogram Chattogram Hathazari A 40 Chattogram Cumilla Laksam A 41 Chattogram Cumilla Chauddagram A 42 Chattogram Chandpur Chandpur A 43 Chattogram Chandpur Hajiganj A -

Evaluation of Netherlands-Funded Ngos in Bangladesh
Evaluation of Netherlands-funded NGOs in Bangladesh Ministry of Foreign Affairs, Policy and Operations Evaluation Department (IOB) ISBN 90-5328-163-0 Photographs: Ron Giling/LINEAIR Maps and figures: Geografiek, Amsterdam Pre-press services: Transcripta, Beerzerveld Printed by: Ridderprint BV, Ridderkerk Preface The evaluation of Netherlands supported NGOs in Bangladesh forms part of a study undertaken by the Policy and Operations Evaluation Department (IOB) on the Netherlands bi-lateral aid programme for Bangladesh in the period 1972–96. The support to NGOs through the regular aid programme and through the Co-financing Programme has been important to the Netherlands’ pursuance of poverty alleviation objectives in Bangladesh. A total of Dfl. .247 million has been disbursed through these channels, some three quarters of which after 1990. The position of NGOs in Bangladeshi society is quite unique. Bangladesh is home to the largest national NGOs in the world, as well as to a multitude of middle- and small-sized NGOs that operate on a national, regional or local level. The Bangladeshi NGOs literally reach out to millions of people in both rural and urban areas. This study comprises extensive case studies of a cross section of NGOs in Bangladesh. Both the Bangladeshi NGOs that were subject of study and their partners in the Netherlands, Bilance (formerly Cebemo), ICCO and Novib, have been closely involved in the various stages of the study. The study has concentrated on the credit and training activities that constitute the mainstay of NGO programmes. It is concluded that these activities effectively target the poorer sections of the population, particularly women. -

Curriculum Vitae of Mohammad Shameem Al Mamun
CURRICULUM VITAE OF MOHAMMAD SHAMEEM AL MAMUN Contact Address: Senior Scientific Officer & Head, Entomology Division Bangladesh Tea Research Institute Srimangal-3210, Moulvibazar, Bangladesh Phone: +880862671225 (Office) Fax: +880862671930 Cell: +8801712119843 E-mail: [email protected] Web: http://shameembtri.webs.com http://bau.academia.edu/msamamun http://facebook.com/shameembtri http://publicationslist.org/shameembtri http://orcid.org/0000-0002-6322-0348 http://livedna.org/880.5244 http://btri.gov.bd Career Objective To develop my career as a good scientist as well as a successful researcher from where I will have the scope to utilize my potentiality & skills to do something innovative and I will be able to enhance my knowledge. Field of Research Bio-ecology of pests, Distributional pattern & seasonal abundance of pests, Crop loss assessment, Bioassay and resistance of pests, Integrated pest management (IPM) in tea, Bio- pesticides & Bio-control as IPM component, Screening of tea clones for pest susceptibility, Screening and standardizing of pesticides for tea and Pesticide residue in tea. Special Qualification Integrated Pest Management, Bio-pesticides and Pesticide residue in tea Key Qualifications Planning, formulating, guiding and conducting entomological researches for tea. Pesticide residue detection and analysis of made tea is another specialized field of work. Conducting laboratory and field trial related to pest management in tea. Analyzing nematodes from the nursery soils of the tea estates. Rendering all sorts of advisory services to the tea estates on the problems arising out of pests of tea. Resource person of Management Training Centre, Project Development Unit, Bangladesh Tea Board. Conducting workshop on tea pest management for planters, managers & staffs of the tea estates.