Coronary Circulation and Hemodynamics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School
Distance Learning Program Anatomy of the Human Heart/Pig Heart Dissection Middle School/ High School This guide is for middle and high school students participating in AIMS Anatomy of the Human Heart and Pig Heart Dissections. Programs will be presented by an AIMS Anatomy Specialist. In this activity students will become more familiar with the anatomical structures of the human heart by observing, studying, and examining human specimens. The primary focus is on the anatomy and flow of blood through the heart. Those students participating in Pig Heart Dissections will have the opportunity to dissect and compare anatomical structures. At the end of this document, you will find anatomical diagrams, vocabulary review, and pre/post tests for your students. National Science Education (NSES) Content Standards for grades 9-12 • Content Standard:K-12 Unifying Concepts and Processes :Systems order and organization; Evidence, models and explanation; Form and function • Content Standard F, Science in Personal and Social Perspectives: Personal and community health • Content Standard C, Life Science: Matter, energy and organization of living systems • Content Standard A Science as Inquiry National Science Education (NSES) Content Standards for grades 5-8 • Content Standard A Science as Inquiry • Content Standard C, Life Science: Structure and function in living systems; Diversity and adaptations of organisms • Content Standard F, Science in Personal and Social Perspectives: Personal Health Show Me Standards (Science and Health/Physical Education) • Science 3. Characteristics and interactions of living organisms • Health/Physical Education 1. Structures of, functions of and relationships among human body systems Objectives: The student will be able to: 1. -

Physiology of Heart Unit-4 (ZOOA-CC4-9-TH)
Physiology of Heart Unit-4 (ZOOA-CC4-9-TH) Coronary Circulation: The heart muscle, like every other organ or tissue in your body, needs oxygen-rich blood to survive. Blood is supplied to the heart by its own vascular system, called coronary circulation. The aorta (the main blood supplier to the body) branches off into two main coronary blood vessels (also called arteries). These coronary arteries branch off into smaller arteries, which supply oxygen-rich blood to the entire heart muscle. The right coronary artery supplies blood mainly to the right side of the heart. The right side of the heart is smaller because it pumps blood only to the lungs. The left coronary artery, which branches into the left anterior descending artery and the circumflex artery, supplies blood to the left side of the heart. The left side of the heart is larger and more muscular because it pumps blood to the rest of the body. Coronary circulation is the circulation of blood in the blood vessels that supply the heart muscle (myocardium). Coronary arteries supply oxygenated blood to the heart muscle, and cardiac veins drain away the blood once it has been deoxygenated. Because the rest of the body, and most especially the brain, needs a steady supply of oxygenated blood that is free of all but the slightest interruptions, the heart is required to function continuously. Therefore its circulation is of major importance not only to its own tissues but to the entire body and even the level of consciousness of the brain from moment to moment. -

Blood Vessels
BLOOD VESSELS Blood vessels are how blood travels through the body. Whole blood is a fluid made up of red blood cells (erythrocytes), white blood cells (leukocytes), platelets (thrombocytes), and plasma. It supplies the body with oxygen. SUPERIOR AORTA (AORTIC ARCH) VEINS & VENA CAVA ARTERIES There are two basic types of blood vessels: veins and arteries. Veins carry blood back to the heart and arteries carry blood from the heart out to the rest of the body. Factoid! The smallest blood vessel is five micrometers wide. To put into perspective how small that is, a strand of hair is 17 micrometers wide! 2 BASIC (ARTERY) BLOOD VESSEL TUNICA EXTERNA TUNICA MEDIA (ELASTIC MEMBRANE) STRUCTURE TUNICA MEDIA (SMOOTH MUSCLE) Blood vessels have walls composed of TUNICA INTIMA three layers. (SUBENDOTHELIAL LAYER) The tunica externa is the outermost layer, primarily composed of stretchy collagen fibers. It also contains nerves. The tunica media is the middle layer. It contains smooth muscle and elastic fiber. TUNICA INTIMA (ELASTIC The tunica intima is the innermost layer. MEMBRANE) It contains endothelial cells, which TUNICA INTIMA manage substances passing in and out (ENDOTHELIUM) of the bloodstream. 3 VEINS Blood carries CO2 and waste into venules (super tiny veins). The venules empty into larger veins and these eventually empty into the heart. The walls of veins are not as thick as those of arteries. Some veins have flaps of tissue called valves in order to prevent backflow. Factoid! Valves are found mainly in veins of the limbs where gravity and blood pressure VALVE combine to make venous return more 4 difficult. -

Abnormally Enlarged Singular Thebesian Vein in Right Atrium
Open Access Case Report DOI: 10.7759/cureus.16300 Abnormally Enlarged Singular Thebesian Vein in Right Atrium Dilip Kumar 1 , Amit Malviya 2 , Bishwajeet Saikia 3 , Bhupen Barman 4 , Anunay Gupta 5 1. Cardiology, Medica Institute of Cardiac Sciences, Kolkata, IND 2. Cardiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 3. Anatomy, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 4. Internal Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, IND 5. Cardiology, Vardhman Mahavir Medical College (VMMC) and Safdarjung Hospital, New Delhi, IND Corresponding author: Amit Malviya, [email protected] Abstract Thebesian veins in the heart are subendocardial venoluminal channels and are usually less than 0.5 mm in diameter. The system of TV either opens a venous (venoluminal) or an arterial (arterioluminal) channel directly into the lumen of the cardiac chambers or via some intervening spaces (venosinusoidal/ arteriosinusoidal) termed as sinusoids. Enlarged thebesian veins are reported in patients with congenital heart disease and usually, multiple veins are enlarged. Very few reports of such abnormal enlargement are there in the absence of congenital heart disease, but in all such cases, they are multiple and in association with coronary artery microfistule. We report a very rare case of a singular thebesian vein in the right atrium, which was abnormally enlarged. It is important to recognize because it can be confused with other cardiac structures like coronary sinus during diagnostic or therapeutic catheterization and can lead to cardiac injury and complications if it is attempted to cannulate it or pass the guidewires. -

Cardiology Self Learning Package
Cardiology Self Learning Package Module 1: Anatomy and Physiology of the Module 1: Anatomy and Physiology of the Heart Heart. Page 1 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) CONTENT Introduction…………………………………………………………………………………Page 3 How to use the ECG Self Learning package………………………………………….Page 4 Overview of the Heart…………………………………………………...…………..…….Page 5 Location, Size and Shape of the Heart…………………………………………………Page 5 The Chambers of the Heart…………….………………………………………..……….Page 7 The Circulation System……………………………………….………………..…………Page 8 The Heart Valve Anatomy………………………….…………………………..…………Page 9 Coronary Arteries…………………………………………….……………………..……Page 10 Coronary Veins…………………………………………………………………..……….Page 11 Cardiac Muscle Tissue……………………………………………………………..……Page 12 The Conduction System………………………………………………………………...Page 13 Cardiac Cycle……………………………………………………………………………..Page 15 References…………………………………………………………………………………Page 18 Module Questions………………………………………………………………………..Page 19 Module Evaluation Form………………………………………………………………..Page 22 [Module 1: Anatomy and Physiology of the Heart Page 2 Developed by Tony Curran (Clinical Nurse Educator) and Gill Sheppard (Clinical Nurse Specialist) Cardiology (October 2011) INTRODUCTION Welcome to Module 1: Anatomy and Physiology of the Heart. This self leaning package is designed to as tool to assist nurse in understanding the hearts structure and how the heart works. The goal of this module is to review: Location , size and shape of the heart The chambers of the heart The circulation system of the heart The heart’s valve anatomy Coronary arteries and veins Cardiac muscle tissue The conduction system The cardiac cycle This module will form the foundation of your cardiac knowledge and enable you to understand workings of the heart that will assist you in completing other modules. Learning outcomes form this module are: To state the position of the heart, the size and shape. -

REVIEW ARTICLE Anatomy and Physiology of Coronary Blood Flow
REVIEW ARTICLE Anatomy and physiology of coronary blood flow Heinrich R. Schelbert, MD, PhD INTRODUCTION hypertrophic cardiomyopathy, or coronary artery disease, resting myocardial blood flows frequently are similar to Regional myocardial blood flow can now be mea- those in normal individuals.17-19 It is the response of sured noninvasively in units of milliliters blood per myocardial blood flow to specifically-targeted pharma- minute per gram myocardium. These noninvasive mea- cological or physiological interventions that can uncover surements are not confined to a specific imaging the presence of functional or structural disease-related modality but are available with MRI, CT, and PET, alterations of the coronary circulation. This then under- although, thus far, most investigations of the coronary scores the need for closely examining these targets and circulation in humans have employed PET flow mea- how they relate to anatomical and functional determi- surements. Flow estimates with these different imaging nants of coronary blood flow and, by inference, to modalities were found in animal experiments to correlate myocardial blood flow and their alterations in cardio- well with invasive flow estimates by the arterial blood vascular disease. Local and systemic mechanisms sampling-microsphere technique widely considered as regulate the complex interactions between flow and the ‘‘gold standard’’ of flow measurements.1-11 In these anatomy in order to meet the heart’s energy needs. comparison studies, noninvasively-derived estimates A comprehensive description of the coronary circulatory corresponded linearly with invasively-measured myo- function and its control exceeds the scope of this review cardial blood flows over a wide flow range, i.e., from as so that the interested reader is referred to detailed reviews low as 0.3 mL/minute/g to as high as 5-6 mL/minute/g. -

Coronary Artery Disease
Coronary Artery Disease Your heart is a muscle — a very important muscle that your entire body depends on. As with all muscles, the heart is dependent on blood supply to provide necessary nutrients, fuel and oxygen. The heart gets its blood supply from the coronary arteries. The coronary arteries surround the heart. When the coronary arteries become blocked, narrowed or completely obstructed, the heart cannot get the nutrients, fuel and oxygen it needs. This can cause the heart to become weak or stop altogether or cause a heart attack. This blockage, narrowing or obstruction is known as coronary artery disease (CAD). Who Gets Coronary Artery Disease? Worldwide, coronary artery disease is responsible for over one-third of deaths in adults over age 35! Coronary artery disease is also the number one killer in the United States. For persons aged 40 years, the lifetime risk of developing coronary artery disease is 49 percent in men and 32 percent in women. For those reaching age 70 years, the lifetime risk is 35 percent in men and 24 percent in women. For total coronary events, the incidence rises steeply with age, with women lagging behind men by 10 years. A variety of other factors can increase risk of developing coronary aretery disease including: • Excess fats and cholesterol in the blood • High blood pressure • Excess sugar in the blood (high blood glucose, often due to diabetes) • Early onset of coronary disease in the family history • Sedentary lifestyle (sitting a lot) • Poor diet (higher in processed foods, animal-based proteins and fats) What are the Symptoms? Coronary artery disease (CAD) makes it more difficult for oxygen-rich blood to move through arteries supplying the heart. -

13-Coronary Anatomy
Atualização Anatomia coronária com angiografia por tomografia computadorizada multicorte ANATOMIA CORONÁRIA COM ANGIOGRAFIA POR TOMOGRAFIA COMPUTADORIZADA MULTICORTE* Joalbo Matos Andrade1 Resumo Com o rápido crescimento do uso da tomografia computadorizada multicorte no estudo das doenças coro- nárias, é de fundamental importância o conhecimento da anatomia arterial e venosa coronária. Unitermos: Artéria coronária; Anatomia; Angiografia; Tomografia computadorizada multidetectores. Abstract Coronary anatomy with multidetector computed tomography angiography. Multidetector computed tomography has been progressively used for evaluation of coronary artery disease, so the knowledge about the anatomy of coronary arteries and veins is of fundamental importance. Keywords: Coronary artery; Anatomy; Angiography; Multidetector computed tomography. INTRODUÇÃO da anatomia coronária arterial e venosa relho de 16 fileiras de detectores Mx 8000 (Figuras 1 e 2). IDT (Philips; Holanda). As imagens angio- As técnicas de detecção e quantificação gráficas foram adquiridas em apnéia e sin- de cálcio coronário e a angiografia coroná- MATERIAIS E MÉTODOS cronizadas ao eletrocardiograma, com re- ria por tomografia computadorizada vêm construção retrospectiva a cada 10% den- sendo utilizadas de modo crescente(1–4). A Tomografia computadorizada multicorte tro do intervalo R-R. Os parâmetros técni- avaliação adequada requer conhecimento (TCMC) coronariana foi obtida com apa- cos são mostrados na Tabela 1. Figura 1. Artérias e veias coronárias. Sistema ar- AB terial. -

22. Heart.Pdf
CARDIOVASCULAR SYSTEM OUTLINE 22.1 Overview of the Cardiovascular System 657 22.1a Pulmonary and Systemic Circulations 657 22.1b Position of the Heart 658 22 22.1c Characteristics of the Pericardium 659 22.2 Anatomy of the Heart 660 22.2a Heart Wall Structure 660 22.2b External Heart Anatomy 660 Heart 22.2c Internal Heart Anatomy: Chambers and Valves 660 22.3 Coronary Circulation 666 22.4 How the Heart Beats: Electrical Properties of Cardiac Tissue 668 22.4a Characteristics of Cardiac Muscle Tissue 668 22.4b Contraction of Heart Muscle 669 22.4c The Heart’s Conducting System 670 22.5 Innervation of the Heart 672 22.6 Tying It All Together: The Cardiac Cycle 673 22.6a Steps in the Cardiac Cycle 673 22.6b Summary of Blood Flow During the Cardiac Cycle 673 22.7 Aging and the Heart 677 22.8 Development of the Heart 677 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch22_656-682.indd 656 2/14/11 4:29 PM Chapter Twenty-Two Heart 657 n chapter 21, we discovered the importance of blood and the which carry blood back to the heart. The differences between I myriad of substances it carries. To maintain homeostasis, blood these types of vessels are discussed in chapter 23. Most arteries must circulate continuously throughout the body. The continual carry blood high in oxygen (except for the pulmonary arteries, pumping action of the heart is essential for maintaining blood as explained later), while most veins carry blood low in oxygen circulation. If the heart fails to pump adequate volumes of blood, (except for the pulmonary veins). -
Structure Coronary Circulation
B C M Y X CMY B5 C5 M5 Y5 X5 B C M Y X 40% 80% B C M Y X B C M Y X 40% 80% B C M Y Prinect/FOGRA 5 Dipco 2.1 Format 105 © 2004 FOGRA/Heidelberger Druckmaschinen AG B C M Y X 40% 80% B C M Y X B C M Y X 40% 80% B C M Y X B C M Y X B C M Y X B5 C5 M5 Y5 X5 CMY B C M Y X B C M Y X CMY B5 C5 M5 Y5 X5 B C M Y X 40% 80% B C M Y X B C M Y X 40% 80% B C M Y Prinect/FOGRA 5 Dipco 2.1 Format 105 © 2004 FOGRA/Heidelberger Druckmaschinen AG B C M Y X 40% 80% B C M Y X B C M Y X 40% 80% B C M Y X B C M Y X B C M Y X B5 C5 M5 Y5 X5 CMY B C M Y X 5 5 5 5 5 5 5 5 5 5 4 4 4 4 4 4 4 4 4 4 3 3 3 3 3 3 3 3 3 3 2 2 2 2 2 2 2 2 2 2 1 1 1 1 1 1 1 1 1 1 1234567891011121314151617181920212223242526272829303132 coronary circulation The heart is a continuous pump which distributes blood to every part of the body. Blood carries essential oxygen to the tissues and carries away unwanted carbon dioxide and other waste products. -

Evaluation of Anatomy, Variation and Anomalies of the Coronary Arteries with Coronary Computed Tomography Angiography
154 Review Derleme Evaluation of anatomy, variation and anomalies of the coronary arteries with coronary computed tomography angiography Koroner arterlerin anatomi, varyasyon ve anomalilerinin koroner bilgisayarlı tomografi anjiyografi ile değerlendirilmesi Cengiz Erol, Mustafa Koplay, Yahya Paksoy Department of Radiology, Selçuklu Faculty of Medicine, Selçuk University, Konya-Turkey ABSTRACT Recent technical advances in computed tomography (CT) have improved image quality, diagnostic performance and accuracy of coronary CT angiography (CCTA). Latest dose-reduction strategies reduce radiation dose to an acceptable level even lower than that from conventional coronary angiography. CCTA is a noninvasive imaging modality which can effectively show complex coronary artery anatomy, variations and congenital anomalies of the coronary arteries. Congenital coronary artery anomalies are rare entities, but sometimes have a potential of producing fatal consequences. CCTA is now the primary imaging modality for the evaluation and diagnosis of coronary artery anomalies. Reporters should, there- fore, have knowledge of the normal coronary artery anatomy and variations, and understand the different types of coronary artery anomalies and their respective prognostic implications in order to provide correct diagnosis and to prevent undesirable mistakes during interventional and surgi- cal procedures. (Anadolu Kardiyol Derg 2013; 13: 154-64) Key words: Coronary artery anatomy, variation, anomalies, coronary computed tomography angiography ÖZET Bilgisayarlı -

1. Right Coronary 2. Left Anterior Descending 3. Left
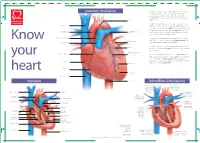
1. RIGHT CORONARY 2. LEFT ANTERIOR DESCENDING 3. LEFT CIRCUMFLEX 4. SUPERIOR VENA CAVA 5. INFERIOR VENA CAVA 6. AORTA 7. PULMONARY ARTERY 8. PULMONARY VEIN 9. RIGHT ATRIUM 10. RIGHT VENTRICLE 11. LEFT ATRIUM 12. LEFT VENTRICLE 13. PAPILLARY MUSCLES 14. CHORDAE TENDINEAE 15. TRICUSPID VALVE 16. MITRAL VALVE 17. PULMONARY VALVE Coronary Arteries Because the heart is composed primarily of cardiac muscle tissue that continuously contracts and relaxes, it must have a constant supply of oxygen and nutrients. The coronary arteries are the network of blood vessels that carry oxygen- and nutrient-rich blood to the cardiac muscle tissue. The blood leaving the left ventricle exits through the aorta, the body’s main artery. Two coronary arteries, referred to as the "left" and "right" coronary arteries, emerge from the beginning of the aorta, near the top of the heart. The initial segment of the left coronary artery is called the left main coronary. This blood vessel is approximately the width of a soda straw and is less than an inch long. It branches into two slightly smaller arteries: the left anterior descending coronary artery and the left circumflex coronary artery. The left anterior descending coronary artery is embedded in the surface of the front side of the heart. The left circumflex coronary artery circles around the left side of the heart and is embedded in the surface of the back of the heart. Just like branches on a tree, the coronary arteries branch into progressively smaller vessels. The larger vessels travel along the surface of the heart; however, the smaller branches penetrate the heart muscle.