Practice Profiles Plus Transforming Cancer Services Team for London Selection Select Area: NHS Enfield CCG Select Year: 2015-16
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neighbourhoods in England Rated E for Green Space, Friends of The
Neighbourhoods in England rated E for Green Space, Friends of the Earth, September 2020 Neighbourhood_Name Local_authority Marsh Barn & Widewater Adur Wick & Toddington Arun Littlehampton West and River Arun Bognor Regis Central Arun Kirkby Central Ashfield Washford & Stanhope Ashford Becontree Heath Barking and Dagenham Becontree West Barking and Dagenham Barking Central Barking and Dagenham Goresbrook & Scrattons Farm Barking and Dagenham Creekmouth & Barking Riverside Barking and Dagenham Gascoigne Estate & Roding Riverside Barking and Dagenham Becontree North Barking and Dagenham New Barnet West Barnet Woodside Park Barnet Edgware Central Barnet North Finchley Barnet Colney Hatch Barnet Grahame Park Barnet East Finchley Barnet Colindale Barnet Hendon Central Barnet Golders Green North Barnet Brent Cross & Staples Corner Barnet Cudworth Village Barnsley Abbotsmead & Salthouse Barrow-in-Furness Barrow Central Barrow-in-Furness Basildon Central & Pipps Hill Basildon Laindon Central Basildon Eversley Basildon Barstable Basildon Popley Basingstoke and Deane Winklebury & Rooksdown Basingstoke and Deane Oldfield Park West Bath and North East Somerset Odd Down Bath and North East Somerset Harpur Bedford Castle & Kingsway Bedford Queens Park Bedford Kempston West & South Bedford South Thamesmead Bexley Belvedere & Lessness Heath Bexley Erith East Bexley Lesnes Abbey Bexley Slade Green & Crayford Marshes Bexley Lesney Farm & Colyers East Bexley Old Oscott Birmingham Perry Beeches East Birmingham Castle Vale Birmingham Birchfield East Birmingham -

BUILDING FOUR North London Business Park
BUILDING4 FOUR AT NORTH LONDON BUSINESS PARK NEW SOUTHGATE • LONDON • N11 1NP 10,000 - 125,000 Sq FT OF mODERN OFFIcE spacE AvAILABLE to LET BUILDING FOUR North LONDON Business PARK modern offices in a 40 acre parkland setting with ornamental lake, extensive car parking and full on-site building management and security. / Finished to Grade A standard / Large single floors of approximately 62,500 sq ft (NIA) / Suites from 5,000 sq ft upwards to 125,000 sq ft / Air conditioned / Full access raised flooring / On-site management and 24 hour security / Extensive car parking / On-site facilities include café, gym and crèche / c lose to Arnos Grove tube station and New Southgate overground station SERvIcED OFFIcES > FROm 250 Sq FT to 5,000 Sq FT A fully serviced office facility is also provided at North London Business Park. The comer Innovation centre offers managed, fully furnished office space on a highly flexible monthly arrangement. The centre offers a highly valuable facility for larger occupiers on the park, either as overflow space or a near-site base for North LONDON Business PARK IS companies with associated services. located IN THE heart OF North LONDON AND SET WITHIN 40 AcRES OF beautifully landscAPED grounds NORTH LONDON BUSINESS PARK FLOOR PLAN - FIRST & SEcOND FLOOR BUILDING4 FOUR void S N FLOOR AREA NIA 1st Floor 63,677 sq ft 5,916 sq m These particulars are believed to be correct but their accuracy is in no way guaranteed nor do 2nd Floor 63,677 sq ft 5,916 sq m they form part of any contract. -

Situation of Polling Stations for the Election of the London Mayor and Assembly Members in the Enfield and Haringey Constituency on Thursday 5 May 2016
Situation of Polling Stations for the election of the London Mayor and Assembly Members in the Enfield and Haringey Constituency on Thursday 5 May 2016 Notice is hereby given that the situation of polling stations at the above election and the descriptions of the persons entitled to vote thereat are as follows: In the area of the London Borough of Enfield Polling Description of Polling Description of Station Situation of polling station persons entitled Station Situation of polling station persons entitled Number to vote Number to vote XA1S Botany Bay Cricket Club, East Lodge Lane, Enfield XAA-1 to XAA-118 XG30S Ellenborough Table Tennis Club, Craddock Road, Enfield XGC-1 to XGC- 1293 XA2A Brigadier Free Church, 36 Brigadier Hill, Enfield XAB-1 to XAB- XG31S Fellowship Hut (Bush Hill Park Recreation Ground), Cecil Avenue, XGD-1 to XGD- 1405 Bush Hill Park 1627 XA2B Brigadier Free Church, 36 Brigadier Hill, Enfield XAB-1406 to XAB- XG32A John Jackson Library, Agricola Place, Bush Hill Park XGE-1 to XGE- 2789 1353 XA3S St. John`s Church Hall, Strayfield Road, Clay Hill XAC-1 to XAC-568 XG32B John Jackson Library, Agricola Place, Bush Hill Park XGE-1354 to XGE- 2584 XA4A St. Lukes Youth Centre, Morley Hill, Enfield XAD-1 to XAD- XG33S St. Marks Hall, Millais Road, (Junction with Main Avenue) XGF-1 to XGF- 1306 1131 XA4B St. Lukes Youth Centre, Morley Hill, Enfield XAD-1307 to XAD- XH34S St. Helier Hall, 12 Eastfield Road, Enfield XHA-1 to XHA- 2531 1925 XA5S Old Ignatian Hall, The Loyola Ground, 147 Turkey Street XAE-1 to XAE-593 XH35A St. -

Foodbank in Demand As Pandemic Continues
ENFIELD DISPATCH No. 27 THE BOROUGH’S FREE COMMUNITY NEWSPAPER DEC 2020 FEATURES A homelessness charity is seeking both volunteers and donations P . 5 NEWS Two new schools and hundreds of homes get go-ahead for hospital site P . 6 ARTS & CULTURE Enfield secondary school teacher turns filmmaker to highlight knife crime P . 12 SPORT How Enfield Town FC are managing through lockdown P . 15 ENFIELD CHASE Restoration Project was officially launched last month with the first of many volunteering days being held near Botany Bay. The project, a partnership between environmental charity Thames 21 and Enfield Council, aims to plant 100,000 trees on green belt land in the borough over the next two years – the largest single tree-planting project in London. A M E E Become a Mmember of Enfield M Dispatch and get O the paper delivered to B your door each month E Foodbank in demand C – find out more R E on Page 16 as pandemic continues B The Dispatch is free but, as a Enfield North Foodbank prepares for Christmas surge not-for-profit, we need your support to stay that way. To BY JAMES CRACKNELL we have seen people come together tial peak in spring demand was Citizens Advice, a local GP or make a one-off donation to as a community,” said Kerry. “It is three times higher. social worker. Of those people our publisher Social Spider CIC, scan this QR code with your he manager of the bor- wonderful to see people stepping “I think we are likely to see referred to North Enfield Food- PayPal app: ough’s biggest foodbank in to volunteer – we have had hun- another big increase [in demand] bank this year, most have been has thanked residents dreds of people helping us. -

BHE City's Cash and Sundry Trusts FINANCIAL
ANNEX 1 Bridge House Estates The Trustee’s Annual Report and Financial Statements for the year ended 31 March 2014 Charity number 1035628 BRIDGE HOUSE ESTATES TRUSTEE’S ANNUAL REPORT AND FINANCIAL STATEMENTS Contents Trustee’s Annual Report Reference and Administrative Details 2 Structure, Governance and Management 3 Objectives and Activities 6 Aims, Achievements, Performance and Future Plans 10 Financial Review 25 Explanation of the Financial Statements 29 Responsibilities of the Trustee 29 Adoption of the Annual Report and Financial Statements 30 Independent Auditor’s Report 31 Report of the Audit Review Panel 33 Statement of Financial Activities 34 Balance Sheet 35 Cash Flow Statement 36 Notes to the Financial Statements 37 List of Grants approved 66 Membership of Committees 86 1 BRIDGE HOUSE ESTATES TRUSTEE’S ANNUAL REPORT AND FINANCIAL STATEMENTS 1. Reference and Administrative Details Bridge House Estates is a Trust governed by various instruments which are mentioned below. In April 1994 it was registered with the Charity Commission. Charity Name Bridge House Estates Other Working Names Bridge House Estates Trust Fund Bridge House Trust Bridge House Grants The City Bridge Trust Charity Number 1035628 Registered Address Guildhall, London, EC2P 2EJ Trustee The Mayor and Commonalty & Citizens of the City of London Chief Executive John Barradell OBE - The Town Clerk of the City of London Corporation Treasurer Chris Bilsland – The Chamberlain of London (February 2007 - May 2014) Dr Peter Kane - The Chamberlain of London (April 2014 – present) Solicitor Michael Cogher - The Comptroller and City Solicitor Bank Lloyds TSB Bank plc Discretionary Fund Managers Artemis Investment Management LLP, Wellington Management Co LLP, Veritas Asset Management LLP, Carnegie Asset Management, Ruffer LLP, Southeastern Asset Management Inc., GMO (U.K.) Ltd, Pryford International Plc, Standard Life Investments Ltd and M&G Investment Management Ltd. -

Question 2 SECRETARY GENERAL
Question 2 SECRETARY GENERAL Churches that reported child (aged under 16) attendance of 101 or over in all three of the years 2015 to 2017 Abingdon: Christ Church Harrogate: St Mark Oxford: St Andrew Ashtead: St George's Christian Centre Holy Trinity Brompton Oxford: St Ebbe Bishopsgate: St Helen Howell Hill: St Paul Reigate: St Mary Magdalene Jesmond: Clayton Memorial Brighton: St Peter Church Rusholme: Holy Trinity Cambridge: St Andrew the Great Lancaster: St Thomas Sevenoaks: St Nicholas Stratford: St John the Cheltenham: Holy Trinity Langham Place: All Souls Evangelist Tonge-cum-Alkrington: St Crookes: St Thomas Leamington Priors: St Paul Michael Wandsworth: St Michael & Fulwood: Christ Church Longfleet: St Mary All Angels, Southfields Maidenhead: St Andrew & Warfield: St Michael the Halliwell: St Peter St Mary Magdalene Archangel Harborne: St John the Baptist Muswell Hill: St James West Ealing: St Paul Woodside Park: St Harpenden: St Nicholas Oxford: St Aldate Barnabas 1 Question 2 SECRETARY GENERAL Churches that reported child (aged under 16) attendance of 51-100 in all three of the years 2015 to 2017 Aldridge: St Mary the Virgin Harold Wood: St Peter Solihull: St Alphege Ashton-upon-Mersey: St Mary Magdalene Harwood: Christ's Church South Croydon: Emmanuel Blackheath: St John the South Wimbledon: Holy Evangelist Hazlemere: Holy Trinity Trinity & St Peter Southampton (Highfield) Bournemouth: St Swithun High Crompton: St Mary Portswood: Christ Church High Harrogate: Christ Broxbourne: St Augustine Church Southwark Cathedral Brussels -

Download Alternative Route
ALTERNATIVE ROUTES DURING DISRUPTION KING’S LYNN Suggested alternative 37* Watlington Downham Market routes during times of Littleport ELY disruption XL* Waterbeach 9*,12* Cambridge North PETERBOROUGH CAMBRIDGE Journeys via alternative routes may take longer than B* Huntingdon your normal journey or operate only at certain times. Foxton St Neots Shepreth Meldreth Sandy On some alternative routes, you may need to purchase BEDFORD X5* Royston Biggleswade Ashwell & a ticket and apply for a refund*. Full details of where Flitwick Morden Arlesey Baldock your ticket will be accepted will be available on our Audley End websites during times of disruption. Harlington Letchworth Garden City HITCHIN 97, 98 Leagrave Stansted 55 Airport GreatNorthernRail.com STEVENAGE LUTON 101 Watton-at-Stone Bishops Stortford ThameslinkRailway.com LUTON AIRPORT 100 Knebworth Hertford PARKWAY 301 HERTFORD NORTH East Welwyn North 724 Harlow Town Hertford Further information will be available from the sources Harpenden 366, WELWYN GARDEN CITY 301 Bayford Bus Stn 610 724 Cuffley below: 242 Broxbourne ST ALBANS CITY 301, 302, 601 Hatfield 602, 653, 724 242 Crews Hill Cheshunt Welham Green National Rail Enquiries 610 601 Brookmans Park Gordon Hill Enfield Enfield nationalrail.co.uk Radlett Potters Bar Town 84 Chase 03457 48 49 50 313 High Hadley Wood Grange Park Elstree & Borehamwood Barnet New Barnet 107 Cockfosters Winchmore Hill Transport for London Oakleigh Park Tottenham (Tube & bus services within London travel zones) Mill Hill Broadway Palmers Green Hale New Southgate -

Enfield Tackling Gangs and Serious Youth Violence Strategy
Enfield Tackling Gangs and Serious Youth Violence Strategy 2015-2017 1 Executive Summary This document sets out what Enfield partners working collaboratively, are seeking to achieve by 2017, to combat gang violence and reduce the harm caused by gangs to individuals and communities in Enfield. The timescale of the strategy to 2017, with a planned annual review, reflects the need to ensure that we match the rapidly changing profile of London Gangs within the context of other regional or national policy changes. 1.1 We know that typically our gang members are getting younger, they are often poor, and their families face challenges that would test the best of us. Our aim is support parents who want to see their children achieve success and not break the law. The picture in Enfield is further complicated by the effect of cheaper housing costs that make Enfield an attractive borough to place gang members from other boroughs. 1.1.1 The approach focuses on 4 key elements: Identification: The prevention, intervention, and enforcement work will be underpinned by a firm commitment to improve how partners share information and resources and the development of an even better understanding of the gang crime picture, and what works to reduce the harm caused by gangs. Prevention: Ensuring that children and young people avoid gang involvement by providing prevention programmes accessible through schools and other agencies. Intervention: A consistent approach to commissioning and delivering sustainable services in the community to reduce serious youth violence and the harm caused by gangs. Enforcement: A targeted criminal justice system approach which delivers swift appropriate justice to deter and put a stop to the criminal behaviour of the most harmful gang members. -
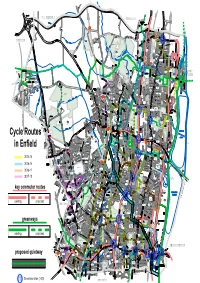
Cycle Routes in Enfield
9'.9;0*#6(+'.& $41:$1740' CREWS HILL Holmesdale Tunnel Open Space Crews Hill Whitewebbs Museum Golf Course of Transport Capel Manor Institute of Lea Valley Lea Valley Horticulture and Field Studies *'465/'4' Sports Centre High School 20 FREEZYWATER Painters Lane Whitewebbs Park Open Space Aylands Capel Manor Primary School Open Space Honilands Primary School Bulls Cross Field Whitewebbs Park Golf Course Keys Meadow School Warwick Fields Open Space Myddelton House and Gardens Elsinge St John's Jubilee C of E Primary School Freezywaters St Georges Park Aylands C of E Primary School TURKEY School ENFIELD STREET LOCK St Ignatius College RC School Forty Hall The Dell Epping Forest 0%4 ENFIELD LOCK Hadley Wood Chesterfield Soham Road Forty Hill Primary School Recreation Ground '22+0) Open Space C of E Primary School 1 Forty Hall Museum (14'56 Prince of Wales Primary School HADLEY Hadley Wood Hilly Fields Gough Park WOOD Primary School Park Hoe Lane Albany Leisure Centre Wocesters Open Space Albany Park Primary School Prince of Oasis Academy North Enfield Hadley Wales Field Recreation Ground Ansells Eastfields Lavender Green Primary School St Michaels Primary School C of E Hadley Wood Primary School Durants Golf Course School Enfield County Lower School Trent Park Country Park GORDON HILL HADLEY WOOD Russet House School St George's Platts Road Field Open Space Chase Community School St Michaels Carterhatch Green Infant and Junior School Trent Park Covert Way Mansion Queen Elizabeth David Lloyd Stadium Centre ENFIELD Field St George's C of E Primary School St James HIGHWAY St Andrew's C of E Primary School L.B. -

Buses from Cockfosters
Buses from Cockfosters 298 Route 298 terminates at Potters Bar Station Key Potters Bar Mutton Lane Potters Bar on Monday to Friday evenings and at weekends Cranborne Road 298 Day buses in black Industrial Estate N91 Night buses in blue Potters Bar POTTERS BAR Lion —O Connections with London Underground o Connections with London Overground R Connections with National Rail Southgate Road M Mondays to Fridays daytime only Stagg Hill Slopers Pond Farm Red discs show the bus stop you need for your chosen bus Cockfosters Road service. The disc appears on the top of the bus stop in the Beech Hill street (see map of town centre in centre of diagram). Cockfosters Road Green Oak Place Cockfosters Road The yellow tinted area includes every Route finder Coombehurst Close bus stop up to about one-and-a-half miles from Cockfosters. Main stops Day buses Cockfosters Road are shown in the white area outside. Bus route Towards Bus stops Trent Country Park 307 Brimsdown 298 Arnos Grove +BDJ Castlewood Road Potters Bar +ACK B Cockfosters NT Green Street Grove Road ELMO A 299 Muswell Hill Broadway +BDE B C L Northfield Road O S Barnet Hospital +HL Westbrook Crescent E 307 Westbrook Square Hail & Ride Mount Pleasant ANT Hertford Road Brimsdown PLEAS W +EN section UNT ESTP MO OLE AV Barnet B ENU 384 Lawton Road C E Ponders End O G Westbrook Crescent C L K O Night buses FO U C K Stapylton Road S E T S E Southbury Road Baring Road E T N Bus route Towards Bus stops R E T Fordham Road S R Hail & Ride D UE C R G R ENFIELD N91 Trafalgar Square +BDE section EN O A -
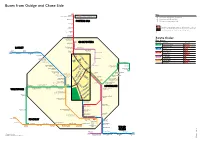
Buses from Osidge and Chase Side
POTTERS BAR COCKFOSTERS BARNET SOUTHGATE WHETSTONE FINCHLEY WOOD GREEN Buses from Osidge and Chase Side 298 Potters Bar Key Cranborne Road Industrial Estate Route 298 terminates at Potters Bar Station on Monday to Friday evenings and at weekends —O Connections with London Underground Potters Bar R Connections with National Rail POTTERS BAR M Mondays to Fridays daytime only Potters Bar Lion Potters Bar Red discs show the bus stop you need for your chosen bus Southgate Road service. The disc appears on the top of the bus stop in the street (see map of town centre in centre of diagram). Stagg Hill SloperÕs Pond Farm Hadley Wood Cockfosters Road Cockfosters Road Route finder Trent Country Park Day buses 299 COCKFOSTERS Cockfosters Bus route Towards Bus stops 125 Finchley Central EFS Winchmore Hill + Cockfosters Road Bramley Road +GHR BARNET Freston Gardens Cockfosters Road 184 Barnet WX Bramley Road Barnet Barnet Chase Side Peace Close Turnpike Lane GY Chesterfield Road Church Meadway Bramley Road Reservoir Road Arnos Grove PQR 184 Mays Lane High Barnet 298 Potters Bar STU New Barnet U P 299 Cockfosters S T R E The Fairway East Barnet Road N Muswell Hill R NK T Victoria Road O . M M E R AV G 382 Mill Hill East EFS FA E A Hail & Ride section East Barnet Road AN C R L H Q D Green Dragon Lane A E Southgate HR Crescent Road S N E S East Barnet Road Avenue Road East Barnet Village AY Eversley Park Road Green Lanes W T S Eversley Mount I E H D U T E EN Church Hill Road I V AD Winchmore Hill FR A O Littlegrove K R N R Station Road MO 125 K Church Hill Road L A Winchmore Hill Road D Southgate Cedar Avenue W E Parkside A S Church Hill O ASDA S R Gardens R Church Hill Road A I R M Winchmore Hill Road St. -

Send a Letter to Seema
forum FocusJune / July 2019 E n f i E l d Borough o v E r 5 0 s f o r u m n E w s l E t t E r Send a letter to Seema You may well be asking “Who is this Seema?” Well, Seema Kennedy MP is the Minister in the Department of Health and Social Care responsible for Public Health and Primary Care. the forum is appealing to all its members, supporters and getting £69 – almost 50% more than our £47 – when these newsletter readers to write a short, simple single-page letter three boroughs are linked with Enfield in a north Central to seema Kennedy asking: london nhs consortium pledged to “why has the assessment of public health reduce health inequalities for their 1.5 funding for Enfield (the borough with the million citizens? fastest growing population in london) not the forum has received a letter from the been updated since 2015, despite us having policy manager, public health systems and some of the most deprived and poverty- strategy, at the department of health & stricken wards in the country? social Care, telling us that although they “why is Enfield’s public health grant of are giving Kensington and Chelsea residents £47 per head of our growing population £130 per head to spend on public health so much lower than the average £73 for all “we do not consider a per capita basis to be london’s boroughs? the best way of determining allocations”. “without waiting for the next spending so if that is the case, why do the whitehall review in 2020, will you now ensure that policymakers take the lazy route of just Enfield gets a fair deal for funding its looking at what we had last year and then vital public health services – funding the cut it.