PDF-Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Development and Maintenance of Epidermal Stem Cells in Skin Adnexa
International Journal of Molecular Sciences Review Development and Maintenance of Epidermal Stem Cells in Skin Adnexa Jaroslav Mokry * and Rishikaysh Pisal Medical Faculty, Charles University, 500 03 Hradec Kralove, Czech Republic; [email protected] * Correspondence: [email protected] Received: 30 October 2020; Accepted: 18 December 2020; Published: 20 December 2020 Abstract: The skin surface is modified by numerous appendages. These structures arise from epithelial stem cells (SCs) through the induction of epidermal placodes as a result of local signalling interplay with mesenchymal cells based on the Wnt–(Dkk4)–Eda–Shh cascade. Slight modifications of the cascade, with the participation of antagonistic signalling, decide whether multipotent epidermal SCs develop in interfollicular epidermis, scales, hair/feather follicles, nails or skin glands. This review describes the roles of epidermal SCs in the development of skin adnexa and interfollicular epidermis, as well as their maintenance. Each skin structure arises from distinct pools of epidermal SCs that are harboured in specific but different niches that control SC behaviour. Such relationships explain differences in marker and gene expression patterns between particular SC subsets. The activity of well-compartmentalized epidermal SCs is orchestrated with that of other skin cells not only along the hair cycle but also in the course of skin regeneration following injury. This review highlights several membrane markers, cytoplasmic proteins and transcription factors associated with epidermal SCs. Keywords: stem cell; epidermal placode; skin adnexa; signalling; hair pigmentation; markers; keratins 1. Epidermal Stem Cells as Units of Development 1.1. Development of the Epidermis and Placode Formation The embryonic skin at very early stages of development is covered by a surface ectoderm that is a precursor to the epidermis and its multiple derivatives. -
Comparative Gene Expression Profiling of Stromal Cell Matrices
ell Res C ea m rc te h S & f o T h l Journal of Tiwari et al., J Stem Cell Res Ther 2013, 3:4 e a r n a r p u DOI: 10.4172/2157-7633.1000152 y o J ISSN: 2157-7633 Stem Cell Research & Therapy Research Article Open Access Comparative Gene Expression Profiling of Stromal Cell Matrices that Support Expansion of Hematopoietic Stem/Progenitor Cells Abhilasha Tiwari1,2, Christophe Lefevre2, Mark A Kirkland2*, Kevin Nicholas2 and Gopal Pande1* 1CSIR-Centre for Cellular and Molecular Biology (CCMB), Hyderabad, India 2Deakin University, Waurn Ponds, Geelong, VIC, Australia Abstract The bone marrow microenvironment maintains a stable balance between self-renewal and differentiation of hematopoietic stem/progenitor cells (HSPCs). This microenvironment, also termed the “hematopoietic niche”, is primarily composed of stromal cells and their extracellular matrices (ECM) that jointly regulate HSPC functions. Previously, we have demonstrated that umbilical cord blood derived HSPCs can be maintained and expanded on stromal cell derived acellular matrices that mimic the complexity of the hematopoietic niche. The results indicated that matrices prepared at 20% O2 with osteogenic medium (OGM) were best suited for expanding committed HSPCs, whereas, matrices prepared at 5% O2 without OGM were better for primitive progenitors. Based upon these results we proposed that individual constituents of these matrices could be responsible for regulation of specific HSPC functions. To explore this hypothesis, we have performed comparative transcriptome profiling of these matrix producing cells, which identified differential expression of both known niche regulators, such as Wnt4, Angpt2, Vcam and Cxcl12, as well as genes not previously associated with HSPC regulation, such as Depp. -

Implications for Diabetic Nephropathy
ORIGINAL ARTICLE Hyperglycemia Causes Renal Cell Damage via CCN2-Induced Activation of the Tropomyosin Receptor Kinase A, TrkA Implications for Diabetic Nephropathy Maria Fragiadaki,1 Nicola Hill,1 Reiko Hewitt,1 George Bou-Gharios,1,2 Terence Cook,1,3 Frederick W. Tam,1 Jan Domin,1,4 and Roger M. Mason1 CCN2, a secreted profibrotic protein, is highly expressed in di- biopsy specimens from patients with different stages of DN abetic nephropathy (DN) and implicated in its pathogenesis; (6). CCN2 is also induced by TGF-b, hypoxia (low oxygen), however, the actions of CCN2 in DN remain elusive. We previously and advanced glycation-end products, all of which are demonstrated that CCN2 triggers signaling via tropomyosin re- stimulants that result in kidney damage (6–9). Moreover, ceptor kinase A (TrkA). Trace expression of TrkA is found in CCN2 overexpression in transgenic mice with streptozotocin- normal kidneys, but its expression is elevated in several nephrop- induced DN led to worsening of the disease, thus indicating athies; yet its role in DN is unexplored. In this study we show de the latter may play a profibrotic role after primary injury in novo expression of TrkA in human and murine DN. We go on to the context of diabetes (10). study the molecular mechanisms leading to TrkA activation and show – More evidence that CCN2 is a profibrotic protein comes that it involves hypoxia, as demonstrated by ischemia reperfusion fi injury and in vitro experiments mimicking hypoxia, implicating from studies of genetically modi ed animals. Sonnylal et al. hypoxia as a common pathway leading to disease. -

Versican V2 Assembles the Extracellular Matrix Surrounding the Nodes of Ranvier in the CNS
The Journal of Neuroscience, June 17, 2009 • 29(24):7731–7742 • 7731 Cellular/Molecular Versican V2 Assembles the Extracellular Matrix Surrounding the Nodes of Ranvier in the CNS María T. Dours-Zimmermann,1 Konrad Maurer,2 Uwe Rauch,3 Wilhelm Stoffel,4 Reinhard Fa¨ssler,5 and Dieter R. Zimmermann1 Institutes of 1Surgical Pathology and 2Anesthesiology, University Hospital Zurich, CH-8091 Zurich, Switzerland, 3Vascular Wall Biology, Department of Experimental Medical Science, University of Lund, S-221 00 Lund, Sweden, 4Center for Biochemistry, Medical Faculty, University of Cologne, D-50931 Cologne, Germany, and 5Department of Molecular Medicine, Max Planck Institute of Biochemistry, D-82152 Martinsried, Germany The CNS-restricted versican splice-variant V2 is a large chondroitin sulfate proteoglycan incorporated in the extracellular matrix sur- rounding myelinated fibers and particularly accumulating at nodes of Ranvier. In vitro, it is a potent inhibitor of axonal growth and therefore considered to participate in the reduction of structural plasticity connected to myelination. To study the role of versican V2 during postnatal development, we designed a novel isoform-specific gene inactivation approach circumventing early embryonic lethality of the complete knock-out and preventing compensation by the remaining versican splice variants. These mice are viable and fertile; however, they display major molecular alterations at the nodes of Ranvier. While the clustering of nodal sodium channels and paranodal structures appear in versican V2-deficient mice unaffected, the formation of the extracellular matrix surrounding the nodes is largely impaired. The conjoint loss of tenascin-R and phosphacan from the perinodal matrix provide strong evidence that versican V2, possibly controlled by a nodal receptor, organizes the extracellular matrix assembly in vivo. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Early Acute Microvascular Kidney Transplant Rejection in The
CLINICAL RESEARCH www.jasn.org Early Acute Microvascular Kidney Transplant Rejection in the Absence of Anti-HLA Antibodies Is Associated with Preformed IgG Antibodies against Diverse Glomerular Endothelial Cell Antigens Marianne Delville,1,2,3 Baptiste Lamarthée,4 Sylvain Pagie,5,6 Sarah B. See ,7 Marion Rabant,3,8 Carole Burger,3 Philippe Gatault ,9,10 Magali Giral,11 Olivier Thaunat,12,13,14 Nadia Arzouk,15 Alexandre Hertig,16,17 Marc Hazzan,18,19,20 Marie Matignon,21,22,23 Christophe Mariat,24,25 Sophie Caillard,26,27 Nassim Kamar,28,29 Johnny Sayegh,30,31 Pierre-François Westeel,32 Cyril Garrouste,33 Marc Ladrière,34 Vincent Vuiblet,35 Joseph Rivalan,36 Pierre Merville,37,38,39 Dominique Bertrand,40 Alain Le Moine,41,42 Jean Paul Duong Van Huyen,3,8 Anne Cesbron,43 Nicolas Cagnard,3,44 Olivier Alibeu,3,45 Simon C. Satchell,46 Christophe Legendre,3,4,47 Emmanuel Zorn,7 Jean-Luc Taupin,48,49,50 Béatrice Charreau,5,6 and Dany Anglicheau 3,4,47 Due to the number of contributing authors, the affiliations are listed at the end of this article. ABSTRACT Background Although anti-HLA antibodies (Abs) cause most antibody-mediated rejections of renal allo- grafts, non-anti–HLA Abs have also been postulated to contribute. A better understanding of such Abs in rejection is needed. Methods We conducted a nationwide study to identify kidney transplant recipients without anti-HLA donor-specific Abs who experienced acute graft dysfunction within 3 months after transplantation and showed evidence of microvascular injury, called acute microvascular rejection (AMVR). -

And MMP-Mediated Cell–Matrix Interactions in the Tumor Microenvironment
International Journal of Molecular Sciences Review Hold on or Cut? Integrin- and MMP-Mediated Cell–Matrix Interactions in the Tumor Microenvironment Stephan Niland and Johannes A. Eble * Institute of Physiological Chemistry and Pathobiochemistry, University of Münster, 48149 Münster, Germany; [email protected] * Correspondence: [email protected] Abstract: The tumor microenvironment (TME) has become the focus of interest in cancer research and treatment. It includes the extracellular matrix (ECM) and ECM-modifying enzymes that are secreted by cancer and neighboring cells. The ECM serves both to anchor the tumor cells embedded in it and as a means of communication between the various cellular and non-cellular components of the TME. The cells of the TME modify their surrounding cancer-characteristic ECM. This in turn provides feedback to them via cellular receptors, thereby regulating, together with cytokines and exosomes, differentiation processes as well as tumor progression and spread. Matrix remodeling is accomplished by altering the repertoire of ECM components and by biophysical changes in stiffness and tension caused by ECM-crosslinking and ECM-degrading enzymes, in particular matrix metalloproteinases (MMPs). These can degrade ECM barriers or, by partial proteolysis, release soluble ECM fragments called matrikines, which influence cells inside and outside the TME. This review examines the changes in the ECM of the TME and the interaction between cells and the ECM, with a particular focus on MMPs. Keywords: tumor microenvironment; extracellular matrix; integrins; matrix metalloproteinases; matrikines Citation: Niland, S.; Eble, J.A. Hold on or Cut? Integrin- and MMP-Mediated Cell–Matrix 1. Introduction Interactions in the Tumor Microenvironment. -

Dickkopf-1 Promotes Hematopoietic Regeneration Via Direct and Niche-Mediated Mechanisms
ARTICLES Dickkopf-1 promotes hematopoietic regeneration via direct and niche-mediated mechanisms Heather A Himburg1,7, Phuong L Doan2,7, Mamle Quarmyne1,3, Xiao Yan1,3, Joshua Sasine1, Liman Zhao1, Grace V Hancock4, Jenny Kan1, Katherine A Pohl1, Evelyn Tran1, Nelson J Chao2, Jeffrey R Harris2 & John P Chute1,5,6 The role of osteolineage cells in regulating hematopoietic stem cell (HSC) regeneration following myelosuppression is not well understood. Here we show that deletion of the pro-apoptotic genes Bak and Bax in osterix (Osx, also known as Sp7 transcription factor 7)-expressing cells in mice promotes HSC regeneration and hematopoietic radioprotection following total body irradiation. These mice showed increased bone marrow (BM) levels of the protein dickkopf-1 (Dkk1), which was produced in Osx-expressing BM cells. Treatment of irradiated HSCs with Dkk1 in vitro increased the recovery of both long-term repopulating HSCs and progenitor cells, and systemic administration of Dkk1 to irradiated mice increased hematopoietic recovery and improved survival. Conversely, inducible deletion of one allele of Dkk1 in Osx-expressing cells in adult mice inhibited the recovery of BM stem and progenitor cells and of complete blood counts following irradiation. Dkk1 promoted hematopoietic regeneration via both direct effects on HSCs, in which treatment with Dkk1 decreased the levels of mitochondrial reactive oxygen species and suppressed senescence, and indirect effects on BM endothelial cells, in which treatment with Dkk1 induced epidermal growth factor (EGF) secretion. Accordingly, blockade of the EGF receptor partially abrogated Dkk1-mediated hematopoietic recovery. These data identify Dkk1 as a regulator of hematopoietic regeneration and demonstrate paracrine cross-talk between BM osteolineage cells and endothelial cells in regulating hematopoietic reconstitution following injury. -

2335 Roles of Molecules Involved in Epithelial/Mesenchymal Transition
[Frontiers in Bioscience 13, 2335-2355, January 1, 2008] Roles of molecules involved in epithelial/mesenchymal transition during angiogenesis Giulio Ghersi Dipartimento di Biologia Cellulare e dello Sviluppo, Universita di Palermo, Italy TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Extracellular matrix 3.1. ECM and integrins 3.2. Basal lamina components 4. Cadherins. 4.1. Cadherins in angiogenesis 5. Integrins. 5.1. Integrins in angiogenesis 6. Focal adhesion molecules 7. Proteolytic enzymes 7.1. Proteolytic enzymes inhibitors 7.2. Proteolytic enzymes in angiogenesis 8. Perspective 9. Acknowledgements 10. References 1.ABSTRACT 2. INTRODUCTION Formation of vessels requires “epithelial- Growth of new blood vessels (angiogenesis) mesenchymal” transition of endothelial cells, with several plays a key role in several physiological processes, such modifications at the level of endothelial cell plasma as vascular remodeling during embryogenesis and membranes. These processes are associated with wound healing tissue repair in the adult; as well as redistribution of cell-cell and cell-substrate adhesion pathological processes, including rheumatoid arthritis, molecules, cross talk between external ECM and internal diabetic retinopathy, psoriasis, hemangiomas, and cytoskeleton through focal adhesion molecules and the cancer (1). Vessel formation entails the “epithelial- expression of several proteolytic enzymes, including matrix mesenchymal” transition of endothelial cells (ECs) “in metalloproteases and serine proteases. These enzymes with vivo”; a similar phenotypic exchange can be induced “in their degradative action on ECM components, generate vitro” by growing ECs to low cell density, or in “wound molecules acting as activators and/or inhibitors of healing” experiments or perturbing cell adhesion and angiogenesis. The purpose of this review is to provide an associated molecule functions. -

Anti-MMP26 (GW21139)
3050 Spruce Street, Saint Louis, MO 63103 USA Tel: (800) 521-8956 (314) 771-5765 Fax: (800) 325-5052 (314) 771-5757 email: [email protected] Product Information Anti-MMP26 antibody produced in chicken, affinity isolated antibody Catalog Number GW21139 Formerly listed as GenWay Catalog Number 15-288-21139, Matrix metalloproteinase-26 Antibody. – Storage Temperature Store at 20 °C The product is a clear, colorless solution in phosphate buffered saline, pH 7.2, containing 0.02% sodium azide. Synonyms: Matrix metalloproteinase 26 preproprotein, EC 3.4.24.-; MMP-26; Matrilysin-2; Endometase Species Reactivity: Human Product Description Tested Applications: WB May hydrolyze collagen type IV. fibronectin. fibrinogen. Recommended Dilutions: Recommended starting dilution beta-casein. type I gelatin and alpha-1 proteinase inhibitor. for Western blot analysis is 1:500, for tissue or cell staining Is also able to activates progelatinase B. Proteins of the 1:200. matrix metalloproteinase (MMP) family are involved in the breakdown of extracellular matrix in normal physiological Note: Optimal concentrations and conditions for each processes. such as embryonic development. reproduction. application should be determined by the user. and tissue remodeling. as well as in disease processes. such Precautions and Disclaimer as arthritis and metastasis. Most MMP's are secreted as This product is for R&D use only, not for drug, household, or inactive proproteins which are activated when cleaved by other uses. Due to the sodium azide content a material extracellular proteinases. The enzyme encoded by this gene safety data sheet (MSDS) for this product has been sent to degrades type IV collagen, fibronectin, fibrinogen, and the attention of the safety officer of your institution. -
Supplement 1 Microarray Studies
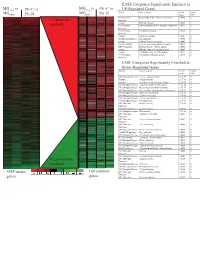
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Perlecan Antagonizes Collagen IV and ADAMTS9/GON-1 in Restricting the Growth of Presynaptic Boutons
The Journal of Neuroscience, July 30, 2014 • 34(31):10311–10324 • 10311 Development/Plasticity/Repair Perlecan Antagonizes Collagen IV and ADAMTS9/GON-1 in Restricting the Growth of Presynaptic Boutons Jianzhen Qin,1,2 Jingjing Liang,1 and X Mei Ding1 1State Key Laboratory of Molecular Developmental Biology, Institute of Genetics and Developmental Biology, Chinese Academy of Sciences, Beijing 100101, China, and 2University of Chinese Academy of Sciences, Beijing 100049, China In the mature nervous system, a significant fraction of synapses are structurally stable over a long time scale. However, the mechanisms that restrict synaptic growth within a confined region are poorly understood. Here, we identified that in the C. elegans neuromuscular junction, collagens Type IV and XVIII, and the secreted metalloprotease ADAMTS/GON-1 are critical for growth restriction of presyn- apticboutons.Withoutthesecomponents,ectopicboutonsprogressivelyinvadeintothenonsynapticregion.Perlecan/UNC-52promotes the growth of ectopic boutons and functions antagonistically to collagen Type IV and GON-1 but not to collagen XVIII. The growth constraint of presynaptic boutons correlates with the integrity of the extracellular matrix basal lamina or basement membrane (BM), which surrounds chemical synapses. Fragmented BM appears in the region where ectopic boutons emerge. Further removal of UNC-52 improves the BM integrity and the tight association between BM and presynaptic boutons. Together, our results unravel the complex role of the BM in restricting the growth of presynaptic boutons and reveal the antagonistic function of perlecan on Type IV collagen and ADAMTS protein. Key words: ADAMTS9/GON-1; basement membrane; perlecan/UNC-52; presynaptic boutons; Type IV collagen/EMB-9; Type XVIII collagen/CLE-1 Introduction wider and present in the form of a basal lamina or basement Synapses are specialized intercellular junctions between neu- membrane (BM) (Palay and Chan-Palay, 1976; Burns and Au- rons or between neurons and other excitable cells.