Spatial UBE2N Protein Expression Indicates Genomic Instability In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Data
Supplemental Figure 1: In vitro viability data A C HDQ-P1 basal-like cells HDQ-P1 untreated HDQ-P1 40 0.04 uM MEKi 35 30 25 MCF7 20 15 CAL85-1 %BrdU 10 Incorporation 5 MDA-MB-231 0 MDA-MB-468 0 6E-05 3E-04 0.002 0.008 0.04 0.2 1 5 25 MEKi (ȝM) T47D luminal cells 50 T-47D untreated T-47D 40 0.2uM MEKi 30 20 PD0325901 (ȝM) %BrdU 10 Incorporation 0 0 6E-05 3E-04 0.002 0.008 0.04 0.2 1 5 25 MEKi (ȝM) B D HDQ-P1 Vehicle Treated 1PM MEKi 100 G1: 45.2% 1500 G1: 62.5% MCF7 1000 S: 4.2% S: 3.4% 75 BT474 800 G2/M: 34.9% 1000 G2/M: 27.4% MDA-MB-231 34.9 27.4 50 600 HDQ-P1 # Cells 4.17 #Cells 3.36 Cell viability (%) 400 CAL85-1 45.2 500 62.5 25 0.001 0.01 0.1 1 10 200 MEK inhibitor 2 (PM) 0 0 0 200 400 600 800 1000 0 200 400 600 800 1000 Propidium Iodide Propidium Iodide EGFR B A WEGFR Levels 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 --- MDA-MB-134VI Basal-like HDQ-P1 BT549 Basal-like Her2 DU4475 CAL51 + HCC1806 Supplemental Figure2:PTENandEGFRinBreastLines - MDA-MB-435s CAL85-1 + HCC70 CAL120 -- MX1 CAL148 CAL-120 + CAL85-1 HCC70 -- SW527 HCC1143 CAL-51 HCC1395 + MDA-MB-231 HCC1937 + HCC1143 + BT20 MDA-MB-231 + Hs578T MDA-MB-436 + MDA-MB-468 MDA-MB-468 - HCC1395 MFM223 + BT-549 - CAL-148 AU565 + HCC1937 BT474 + HCC38 EFM192A + MDA-MB-436 + HCC1954 HCC1419 + AU565 ------ HCC1569 BT474 Her2 orLuminal EFM-192A HCC1954 HCC1419 HCC2218 HCC1569 HCC202 MDA-MB-361 HCC2218 MDA-MB-453 + JIM-T --- SKBR3 KPL4 MDA-MB-361 UACC812 MDA-MB-453 UACC893 + SKBR3 ZR75-30 ---------- UACC-812 -

Defining Functional Interactions During Biogenesis of Epithelial Junctions
ARTICLE Received 11 Dec 2015 | Accepted 13 Oct 2016 | Published 6 Dec 2016 | Updated 5 Jan 2017 DOI: 10.1038/ncomms13542 OPEN Defining functional interactions during biogenesis of epithelial junctions J.C. Erasmus1,*, S. Bruche1,*,w, L. Pizarro1,2,*, N. Maimari1,3,*, T. Poggioli1,w, C. Tomlinson4,J.Lees5, I. Zalivina1,w, A. Wheeler1,w, A. Alberts6, A. Russo2 & V.M.M. Braga1 In spite of extensive recent progress, a comprehensive understanding of how actin cytoskeleton remodelling supports stable junctions remains to be established. Here we design a platform that integrates actin functions with optimized phenotypic clustering and identify new cytoskeletal proteins, their functional hierarchy and pathways that modulate E-cadherin adhesion. Depletion of EEF1A, an actin bundling protein, increases E-cadherin levels at junctions without a corresponding reinforcement of cell–cell contacts. This unexpected result reflects a more dynamic and mobile junctional actin in EEF1A-depleted cells. A partner for EEF1A in cadherin contact maintenance is the formin DIAPH2, which interacts with EEF1A. In contrast, depletion of either the endocytic regulator TRIP10 or the Rho GTPase activator VAV2 reduces E-cadherin levels at junctions. TRIP10 binds to and requires VAV2 function for its junctional localization. Overall, we present new conceptual insights on junction stabilization, which integrate known and novel pathways with impact for epithelial morphogenesis, homeostasis and diseases. 1 National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. 2 Computing Department, Imperial College London, London SW7 2AZ, UK. 3 Bioengineering Department, Faculty of Engineering, Imperial College London, London SW7 2AZ, UK. 4 Department of Surgery & Cancer, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Spectrin Binding Motifs Control Scribble Cortical Dynamics And
1 2 3 Spectrin binding motifs control Scribble cortical 4 dynamics and polarity function 5 6 Batiste Boëda and Sandrine Etienne Manneville 7 8 Institut Pasteur (CNRS URA 3691-INSERM), France 9 Correspondance to Sandrine Etienne-Manneville. Cell Polarity, Migration and Cancer Unit, 10 Institut Pasteur, 25 rue du Dr Roux, 75724 Paris cedex 15, France; Phone: +33 1 4438 9591; 11 FAX: +33 1 4568 8548. 12 e-mail: [email protected] 13 14 Competing interests statement: 15 The authors declare that no competing interests exist. 16 17 1 18 Abstract 19 The tumor suppressor protein Scribble (SCRIB) plays an evolutionary conserved role in 20 cell polarity. Despite being central for its function, the molecular basis of SCRIB 21 recruitment and stabilization at the cell cortex is poorly understood. Here we show that 22 SCRIB binds directly to the CH1 domain of spectrins, a molecular scaffold that 23 contributes to the cortical actin cytoskeleton and connects it to the plasma membrane. 24 We have identified a short evolutionary conserved peptide motif named SADH motif 25 (SCRIB ABLIMs DMTN Homology) which is necessary and sufficient to mediate protein 26 interaction with spectrins. The SADH domains contribute to SCRIB dynamics at the 27 cell cortex and SCRIB polarity function. Furthermore, mutations in SCRIB SADH 28 domains associated with spina bifida and cancer impact the stability of SCRIB at the 29 plasma membrane, suggesting that SADH domain alterations may participate in human 30 pathology. 31 32 33 34 35 36 37 2 38 Introduction 39 The protein SCRIB has been implicated in a staggering array of cellular processes 40 including polarity, migration, proliferation, differentiation, apoptosis, stemcell 41 maintenance, and vesicle trafficking [1]. -
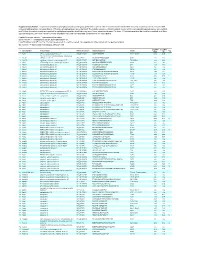
Supplementary Table 1
Supplementary Table 1. Large-scale quantitative phosphoproteomic profiling was performed on paired vehicle- and hormone-treated mTAL-enriched suspensions (n=3). A total of 654 unique phosphopeptides corresponding to 374 unique phosphoproteins were identified. The peptide sequence, phosphorylation site(s), and the corresponding protein name, gene symbol, and RefSeq Accession number are reported for each phosphopeptide identified in any one of three experimental pairs. For those 414 phosphopeptides that could be quantified in all three experimental pairs, the mean Hormone:Vehicle abundance ratio and corresponding standard error are also reported. Peptide Sequence column: * = phosphorylated residue Site(s) column: ^ = ambiguously assigned phosphorylation site Log2(H/V) Mean and SE columns: H = hormone-treated, V = vehicle-treated, n/a = peptide not observable in all 3 experimental pairs Sig. column: * = significantly changed Log 2(H/V), p<0.05 Log (H/V) Log (H/V) # Gene Symbol Protein Name Refseq Accession Peptide Sequence Site(s) 2 2 Sig. Mean SE 1 Aak1 AP2-associated protein kinase 1 NP_001166921 VGSLT*PPSS*PK T622^, S626^ 0.24 0.95 PREDICTED: ATP-binding cassette, sub-family A 2 Abca12 (ABC1), member 12 XP_237242 GLVQVLS*FFSQVQQQR S251^ 1.24 2.13 3 Abcc10 multidrug resistance-associated protein 7 NP_001101671 LMT*ELLS*GIRVLK T464, S468 -2.68 2.48 4 Abcf1 ATP-binding cassette sub-family F member 1 NP_001103353 QLSVPAS*DEEDEVPVPVPR S109 n/a n/a 5 Ablim1 actin-binding LIM protein 1 NP_001037859 PGSSIPGS*PGHTIYAK S51 -3.55 1.81 6 Ablim1 actin-binding -

Biological Models of Colorectal Cancer Metastasis and Tumor Suppression
BIOLOGICAL MODELS OF COLORECTAL CANCER METASTASIS AND TUMOR SUPPRESSION PROVIDE MECHANISTIC INSIGHTS TO GUIDE PERSONALIZED CARE OF THE COLORECTAL CANCER PATIENT By Jesse Joshua Smith Dissertation Submitted to the Faculty of the Graduate School of Vanderbilt University In partial fulfillment of the requirements For the degree of DOCTOR OF PHILOSOPHY In Cell and Developmental Biology May, 2010 Nashville, Tennessee Approved: Professor R. Daniel Beauchamp Professor Robert J. Coffey Professor Mark deCaestecker Professor Ethan Lee Professor Steven K. Hanks Copyright 2010 by Jesse Joshua Smith All Rights Reserved To my grandparents, Gladys and A.L. Lyth and Juanda Ruth and J.E. Smith, fully supportive and never in doubt. To my amazing and enduring parents, Rebecca Lyth and Jesse E. Smith, Jr., always there for me. .my sure foundation. To Jeannine, Bill and Reagan for encouragement, patience, love, trust and a solid backing. To Granny George and Shawn for loving support and care. And To my beautiful wife, Kelly, My heart, soul and great love, Infinitely supportive, patient and graceful. ii ACKNOWLEDGEMENTS This work would not have been possible without the financial support of the Vanderbilt Medical Scientist Training Program through the Clinical and Translational Science Award (Clinical Investigator Track), the Society of University Surgeons-Ethicon Scholarship Fund and the Surgical Oncology T32 grant and the Vanderbilt Medical Center Section of Surgical Sciences and the Department of Surgical Oncology. I am especially indebted to Drs. R. Daniel Beauchamp, Chairman of the Section of Surgical Sciences, Dr. James R. Goldenring, Vice Chairman of Research of the Department of Surgery, Dr. Naji N. -
Identification of the Fatty Acid Synthase Interaction Network Via Itraq-Based Proteomics Indicates the Potential Molecular Mecha
Huang et al. Cancer Cell Int (2020) 20:332 https://doi.org/10.1186/s12935-020-01409-2 Cancer Cell International PRIMARY RESEARCH Open Access Identifcation of the fatty acid synthase interaction network via iTRAQ-based proteomics indicates the potential molecular mechanisms of liver cancer metastasis Juan Huang1, Yao Tang1, Xiaoqin Zou1, Yi Lu1, Sha She1, Wenyue Zhang1, Hong Ren1, Yixuan Yang1,2* and Huaidong Hu1,2* Abstract Background: Fatty acid synthase (FASN) is highly expressed in various types of cancer and has an important role in carcinogenesis and metastasis. To clarify the mechanisms of FASN in liver cancer invasion and metastasis, the FASN protein interaction network in liver cancer was identifed by targeted proteomic analysis. Methods: Wound healing and Transwell assays was performed to observe the efect of FASN during migration and invasion in liver cancer. Isobaric tags for relative and absolute quantitation (iTRAQ)-based mass spectrometry were used to identify proteins interacting with FASN in HepG2 cells. Diferential expressed proteins were validated by co-immunoprecipitation, western blot analyses and confocal microscopy. Western blot and reverse transcription- quantitative polymerase chain reaction (RT-qPCR) were performed to demonstrate the mechanism of FASN regulating metastasis. Results: FASN knockdown inhibited migration and invasion of HepG2 and SMMC7721 cells. A total of, 79 proteins interacting with FASN were identifed. Additionally, gene ontology term enrichment analysis indicated that the majority of biological regulation and cellular processes that the FASN-interacting proteins were associated with. Co- precipitation and co-localization of FASN with fascin actin-bundling protein 1 (FSCN1), signal-induced proliferation- associated 1 (SIPA1), spectrin β, non-erythrocytic 1 (SPTBN1) and CD59 were evaluated. -

Common Genetic Aberrations Associated with Metabolic Interferences in Human Type-2 Diabetes and Acute Myeloid Leukemia: a Bioinformatics Approach
International Journal of Molecular Sciences Article Common Genetic Aberrations Associated with Metabolic Interferences in Human Type-2 Diabetes and Acute Myeloid Leukemia: A Bioinformatics Approach Theodora-Christina Kyriakou 1, Panagiotis Papageorgis 1,2 and Maria-Ioanna Christodoulou 3,* 1 Tumor Microenvironment, Metastasis and Experimental Therapeutics Laboratory, Basic and Translational Cancer Research Center, Department of Life Sciences, European University Cyprus, Nicosia 2404, Cyprus; [email protected] (T.-C.K.); [email protected] (P.P.) 2 European University Cyprus Research Center, Nicosia 2404, Cyprus 3 Tumor Immunology and Biomarkers Laboratory, Basic and Translational Cancer Research Center, Department of Life Sciences, European University Cyprus, Nicosia 2404, Cyprus * Correspondence: [email protected] Abstract: Type-2 diabetes mellitus (T2D) is a chronic metabolic disorder, associated with an increased risk of developing solid tumors and hematological malignancies, including acute myeloid leukemia (AML). However, the genetic background underlying this predisposition remains elusive. We herein aimed at the exploration of the genetic variants, related transcriptomic changes and disturbances in metabolic pathways shared by T2D and AML, utilizing bioinformatics tools and repositories, as well as publicly available clinical datasets. Our approach revealed that rs11709077 and rs1801282, on PPARG, rs11108094 on USP44, rs6685701 on RPS6KA1 and rs7929543 on AC118942.1 comprise Citation: Kyriakou, T.-C.; common SNPs susceptible to the two diseases and, together with 64 other co-inherited proxy SNPs, Papageorgis, P.; Christodoulou, M.-I. may affect the expression patterns of metabolic genes, such as USP44, METAP2, PPARG, TIMP4 and Common Genetic Aberrations RPS6KA1, in adipose tissue, skeletal muscle, liver, pancreas and whole blood. -

MALDI MS Imaging of FFPE Tissues REVIEW Gorzolka and Walch Histology and Histopathology Final
Title: MALDI mass spectrometry imaging of formalin-fixed paraffin-embedded tissues in clinical research Karin Gorzolka1, Axel Walch1 1Institute of Pathology, Research Unit Analytical Pathology Helmholtz Zentrum Muenchen National Research Centre for Environment and Health, Ingolstädter Landstraße 1 85764 Neuherberg, Germany Corresponding author: Axel Walch, MD. eMail: [email protected]; phone: +49 89 3187-2739 HISTOPAHTOLOGY manuscript) AND (non-edited HISTOLOGY 1 Abstract The molecular investigation of archived formalin-fixed, paraffin-embedded (FFPE) tissue samples provides the chance to obtain molecular patterns as indicatives for treatment and clinical end points. MALDI mass spectrometry imaging is capable of localizing molecules like proteins and peptides in tissue sections and became a favorite platform for the targeted and non-targeted approaches, especially in clinical investigations for biomarker research. In FFPE tissues the recovery of proteomic information is constrained by fixation-induced cross-links of proteins. The promising new insights obtained from FFPE in combination with the comprehensive patients’ data caused much progress in the optimization of MS imaging protocols to investigate FFPE samples. This review presents the past and current research in MALDI MS imaging of FFPE tissues, demonstrating the improvement of analyses, their actual limitations, but also the promising future perspectives for histopathological and tissue-based research. Key words FFPE (formalin-fixed, paraffin-embedded), mass spectrometry imaging, MALDI, proteins, peptides Introduction HISTOPAHTOLOGY Formalin fixation became a routine measure for the longmanuscript)-term storage of tissues in clinical settings after its first report in 1893 (Blum, 1893). It sustains the tissue integrity for years (Casadonte & Caprioli, 2011) and biomolecules like proteins, DNA, and RNA can be extracted (Ralton & Murray, 2011; Frankel,AND 2012). -

The K-Cl Co-Transporter 2 Is a Point of Convergence for Multiple Autism Spectrum Disorder and Epilepsy Risk Gene Products
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.02.973859; this version posted March 2, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. KCC2 and autism/epilepsy risk gene products The K-Cl co-transporter 2 is a point of convergence for multiple autism spectrum disorder and epilepsy risk gene products. Joshua L. Smalley1, Georgina Kontou1, Catherine Choi1, Qiu Ren1, David Albrecht1, Krithika Abiraman1, Miguel A. Rodriguez Santos1, Christopher E. Bope1, Tarek Z. Deeb1, Paul A. Davies1, Nicholas J. Brandon2,3 and Stephen J. Moss*1,4 1Department of Neuroscience, Tufts University School of Medicine, 136 Harrison Ave, Boston 02111. 2Sage Therapeutics, 215 First Street, Cambridge, MA 02142. 3Department of Neuroscience, Physiology, and Pharmacology, University College, London, WC1E, 6BT, UK. Running Title: KCC2 and autism/epilepsy risk gene products To whom correspondence should be addressed: Professor. S. J. Moss, Department of Neuroscience, Tufts University School of Medicine, Boston MA 02111, Telephone: (617) 636-3976; FAX: (617) 636-2413; Email: [email protected] Key words; KCC2, epilepsy, proteome, FMRP, autism, phosphorylation. ABSTRACT KCC2 plays a critical role in determining the efficacy of synaptic inhibition The K+/Cl– co-transporter KCC2 (encoded by the and deficits in its activity lead to epilepsy and gene SLC12A5) is the principal Cl--extrusion mechanism employed by mature neurons in the neurodevelopmental delay. Here we use unbiased CNS (1). Its activity is a pre-requisite for the proteomic analyses to demonstrate that KCC2 efficacy of fast synaptic inhibition mediated by forms stable protein complexes in the neuronal Glycine (GLYR) and type A γ-aminobutyric acid plasma membrane with 96 autism and/or epilepsy receptors (GABAAR), which are Cl– permeable risk gene (ASD/Epi) products including ANKB, ligand-gated ion channels. -

Αii-Spectrin and Βii-Spectrin Do Not Affect Tgfβ1-Induced Myofibroblast Differentiation
Cell and Tissue Research https://doi.org/10.1007/s00441-018-2842-x REGULAR ARTICLE αII-spectrin and βII-spectrin do not affect TGFβ1-induced myofibroblast differentiation Bram Piersma1 & Olaf Y. Wouters1 & Ruud A. Bank1 Received: 16 May 2017 /Accepted: 10 April 2018 # The Author(s) 2018 Abstract Mechanosensing of fibroblasts plays a key role in the development of fibrosis. So far, no effective treatments are available to treat this devastating disorder. Spectrins regulate cell morphology and are potential mechanosensors in a variety of non-erythroid cells, but little is known about the role of spectrins in fibroblasts. We investigate whether αII- and βII-spectrin are required for the phenotypic properties of adult human dermal (myo)fibroblasts. Knockdown of αII- or βII-spectrin in fibroblasts did not affect cell adhesion, cell size and YAP nuclear/cytosolic localization. We further investigated whether αII- and βII-spectrin play a role in the phenotypical switch from fibroblasts to myofibroblasts under the influence of the pro-fibrotic cytokine TGFβ1. Knockdown of spectrins did not affect myofibroblast formation, nor did we observe changes in the organization of αSMA stress fibers. Focal adhesion assembly was unaffected by spectrin deficiency, as was collagen type I mRNA expression and protein deposition. Wound closure was unaffected as well, showing that important functional properties of myofibroblasts are unchanged without αII- or βII-spectrin. In fact, fibroblasts stimulated with TGFβ1 demonstrated significantly lower endogenous mRNA levels of αII- and βII-spectrin. Taken together, despite the diverse roles of spectrins in a variety of other cells, αII- and βII-spectrin do not regulate cell adhesion, cell size and YAP localization in human dermal fibroblasts and are not required for the dermal myofibroblast phenotypical switch. -

Breast Pathology
28A ANNUAL MEETING ABSTRACTS Breast Pathology Clincopathologic parameters n=68(%) Predominant MC 101 Overexpression of FoxO3a Is Associated with Lymph Node Squamous 31(45.5) Metastasis and Poor Disease-Free Survival in Triple-Negative Breast Spindle 15(22) Cancers Chondroid 9(13) Rehman Abdul, Yumin Chung, Hyein Ahn, Jongmin Sim, Min Sung Chung, Kiseok Jang. Osseous 4(6) Hanyang University College of Medicine, Seoul, Republic of Korea. Background: Triple negative breast cancer (TNBC) is the most aggressive type of breast Pseudoangiomatous 6(9) cancer, whichis a heterogeneous group and has no proven molecular target. FoxO3a, Mixed 2(3) a transcription factor, is involved in wide spectrum of biological processes, including HG sarcomatoid 1(1.5) cell cycle progression, proliferation, DNA damage repair, and apoptosis.Recently, DCIS with metaplastic features 14(52) accumulating evidences suggests that FoxO3a act as a tumor suppressorin variety Squamous 11(78.5) of human cancers. However,the previous studies usingTNBC cell lines have shown controversial results. The aim of this study was to investigate the clinicopathological Chondroid 2(14) significance and role of FoxO3a in the progression of TNBC. Rhabdoid 1(7.5) Design: Tissue microarrays consisting of 124 cases of TNBC were studied for FoxO3a None 13(48) expression by immunohistochemistry and interpreted by semi-quantitative scoring Grade system. The FoxO3a expression correlated with various clinicopathological parameters, 1 1(1.5) including patient’s survival. Furthermore, cultured TNBC cell lines (MDA-MB-231, MDA-MB-468, BT20) were assessed for FoxO3a expression by western blot. MDA- 2 3(4.5) MB-468 breast cancer cell line was transiently transfected with exogenous siRNA, 3 64(94) which wasspecific for FoxO3a.