Development of a Single Use Device Intended to Wash Blood Clot Debris from a Stent Retriever in the Operating Room
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Work Catalog
Your Partner In Safety -Since 1979- • Illness Prevention Signage BACK TO WORK • Disposable Clothing • Respiratory CATALOG Protection What you need to get back to work safely • Eye Protection • Disinfectants Back To Work Novel Coronavirus (nCoV) Infection Overview The Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) are closely monitoring an outbreak caused by a novel (new) coronavirus first identified in Wuhan, Hubei Province, China. Chinese authorities iden- tified the new coronavirus, which has resulted in hundreds of confirmed cases in China, including cases outside Wuhan, with additional cases being identified in a growing number of countries internationally. These numbers will likely grow given the high amount of travel associated with the Lunar New Year holiday. It has been confirmed that the virus can spread from human to human although specific routes of transmission (i.e. airborne, direct contact, ingestion, etc.) have yet to be definitively determined. Common symptoms include runny nose, headache, cough, sore throat, fever, and a general feeling of being unwell. The CDC is providing the following precautions for health care providers: “Healthcare providers should obtain a detailed travel history for patients with fever and respiratory symptoms. For pa- tients who traveled to Wuhan on or after December 1, 2019 and had onset of illness within 2 weeks of leaving, consider the novel coronavirus outbreak in China when evaluating a patient with these symptoms and notify infection control per- sonnel and your local health department immediately. Although routes of transmission have yet to be definitively determined, CDC recommends a cautious approach to inter- acting with patients under investigation. -

(12) United States Patent (10) Patent No.: US 6,702,110 B1
USOO670211 OB1 (12) UnitedO States Patent (10) Patent No.: US 6,702,110 B1 Flores, Jr. et al. (45) Date of Patent: Mar. 9, 2004 (54) DISC STORAGE CONTAINER 5,573,120 A 11/1996 Kaufman et al. ........... 206/755 5,574,716 A 11/1996 Uchida ....................... 369/291 w 5,584,391 A 12/1996 Weisburn (75) Inventors: Victor' E. SER 5,590,768 A 1/1997 Hilton et al. ............ 206/308.1 erdes, CA (US); Victorio M. Flores, 5,597,068 A 1/1997 Weisburn et al. ........ 206/308.1 III, San Pedro, CA (US); Ernst C. 5,615,779 A 4/1997 Marsilio et al. .............. 211/40 Benjamins, Covina, CA (US) 5,682,991. A 11/1997 Lammerant et al. ..... 206/308.1 5,690,218 A 11/1997 McCamy et al. ........... 206/303 (73) ASSignee: Ace Packaging, Inc., Lake Forest, CA D387,217 S 12/1997 Lakoski et al. .............. D6/407 (US) 5,713,463 A 2/1998 Lakoski et al. .......... 206/308.1 5,762,187 A 6/1998 Belden, Jr. et al. ...... 206/3O8.2 - - - - 5,779,038 A 7/1998 Herr et al. ............... 206/3O8.2 (*) Notice: Subject to any disclaimer, the term of this 5,782,350 A 7/1998 Weisburn et al. ........ 206/3O8.2 patent is extended or adjusted under 35 5,788,068 A 8/1998 Fraser et al. ................ 206/310 U.S.C. 154(b) by 0 days. 5,794,796 A 8/1998 Weisburn ..................... 211/40 5,816,394 A 10/1998 O’Brien et al. .......... 206/308.1 5,829,582 A 11/1998 Ippolito et al. -

Brands Talk Sustainability: Exclusive M&S and Coca-Cola Interviews
VOLUME 13.1 – 2018 BRANDS TALK SUSTAINABILITY: EXCLUSIVE M&S AND COCA-COLA INTERVIEWS WHAT ARE THE DEFINING TRENDS OF 2018? SERIALISATION PERSPECTIVES MINIMALIST DESIGN: THE POWER OF SILENCE INTRODUCING THE DIGITAL NOMAD Cover image © Mehmet Gözetlik Head of Content Senior Account VOLUME 13.1 – 2018 Tim Sykes Managers Kevin Gambrill Editors Jesse Roberts Elisabeth Skoda Libby White Account Manager Dominic Kurkowski Head of Studio Gareth Harrey Executive Assistant Amber Dawson Art Editor Paul Holden-Abbott IT Support Syed Hassan Advertising Coordinator Kayleigh Harvey Data Manager 3 Editorial Tim Sykes Andrew Wood 5 M&S Interview Are we looking at a one-polymer future? 7 2018 Predictions This year’s defining trends in CPG and retail packaging 14 Smart Manufacturing Automation perspectives 17 Innovation Spotlight Pont brings twist to cap design Packaging Europe Ltd 18 Coca-Cola Interview Inside the new sustainability plan Part of the Rapid News Communications Group 20 Pharmapack The future is now Alkmaar House, Alkmaar Way, Norwich, Norfolk, NR6 6BF, UK 23 Bostik What if hotmelt adhesives could bring comfort and safety in your plant? Registered Office: Carlton House, Sandpiper Way, 25 Smurfit Kappa On-shelf differentiation in advance Chester Business Park, Chester, CH4 9QE. 28 Bioplastics EUBP Conference review Company No: 10531302. 31 ADF/PCD Paris Counting down to the next edition Registered in England. VAT Registration No. GB 265 4148 96 33 Prosweets Sweet solution 35 Ipack-Ima Ipack-Ima returns with new vision Telephone: +44 (0)1603 -

Food Packaging Technology
FOOD PACKAGING TECHNOLOGY Edited by RICHARD COLES Consultant in Food Packaging, London DEREK MCDOWELL Head of Supply and Packaging Division Loughry College, Northern Ireland and MARK J. KIRWAN Consultant in Packaging Technology London Blackwell Publishing © 2003 by Blackwell Publishing Ltd Trademark Notice: Product or corporate names may be trademarks or registered Editorial Offices: trademarks, and are used only for identification 9600 Garsington Road, Oxford OX4 2DQ and explanation, without intent to infringe. Tel: +44 (0) 1865 776868 108 Cowley Road, Oxford OX4 1JF, UK First published 2003 Tel: +44 (0) 1865 791100 Blackwell Munksgaard, 1 Rosenørns Allè, Library of Congress Cataloging in P.O. Box 227, DK-1502 Copenhagen V, Publication Data Denmark A catalog record for this title is available Tel: +45 77 33 33 33 from the Library of Congress Blackwell Publishing Asia Pty Ltd, 550 Swanston Street, Carlton South, British Library Cataloguing in Victoria 3053, Australia Publication Data Tel: +61 (0)3 9347 0300 A catalogue record for this title is available Blackwell Publishing, 10 rue Casimir from the British Library Delavigne, 75006 Paris, France ISBN 1–84127–221–3 Tel: +33 1 53 10 33 10 Originated as Sheffield Academic Press Published in the USA and Canada (only) by Set in 10.5/12pt Times CRC Press LLC by Integra Software Services Pvt Ltd, 2000 Corporate Blvd., N.W. Pondicherry, India Boca Raton, FL 33431, USA Printed and bound in Great Britain, Orders from the USA and Canada (only) to using acid-free paper by CRC Press LLC MPG Books Ltd, Bodmin, Cornwall USA and Canada only: For further information on ISBN 0–8493–9788–X Blackwell Publishing, visit our website: The right of the Author to be identified as the www.blackwellpublishing.com Author of this Work has been asserted in accordance with the Copyright, Designs and Patents Act 1988. -
The Dynisco Extrusion Processors Handbook 2Nd Edition
The Dynisco Extrusion Processors Handbook 2nd edition Written by: John Goff and Tony Whelan Edited by: Don DeLaney Acknowledgements We would like to thank the following people for their contributions to this latest edition of the DYNISCO Extrusion Processors Handbook. First of all, we would like to thank John Goff and Tony Whelan who have contributed new material that has been included in this new addition of their original book. In addition, we would like to thank John Herrmann, Jim Reilly, and Joan DeCoste of the DYNISCO Companies and Christine Ronaghan and Gabor Nagy of Davis-Standard for their assistance in editing and publication. For the fig- ures included in this edition, we would like to acknowledge the contributions of Davis- Standard, Inc., Krupp Werner and Pfleiderer, Inc., The DYNISCO Companies, Dr. Harold Giles and Eileen Reilly. CONTENTS SECTION 1: INTRODUCTION TO EXTRUSION Single-Screw Extrusion . .1 Twin-Screw Extrusion . .3 Extrusion Processes . .6 Safety . .11 SECTION 2: MATERIALS AND THEIR FLOW PROPERTIES Polymers and Plastics . .15 Thermoplastic Materials . .19 Viscosity and Viscosity Terms . .25 Flow Properties Measurement . .28 Elastic Effects in Polymer Melts . .30 Die Swell . .30 Melt Fracture . .32 Sharkskin . .34 Frozen-In Orientation . .35 Draw Down . .36 SECTION 3: TESTING Testing and Standards . .37 Material Inspection . .40 Density and Dimensions . .42 Tensile Strength . .44 Flexural Properties . .46 Impact Strength . .47 Hardness and Softness . .48 Thermal Properties . .49 Flammability Testing . .57 Melt Flow Rate . .59 Melt Viscosity . .62 Measurement of Elastic Effects . .64 Chemical Resistance . .66 Electrical Properties . .66 Optical Properties . .68 Material Identification . .70 SECTION 4: THE SCREW AND BARREL SYSTEM Materials Handling . -
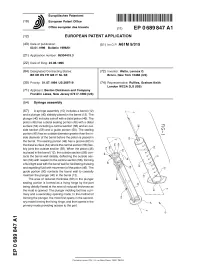
Syringe Assembly
^ ^ ^ ^ I ^ ^ ^ ^ ^ ^ II ^ II ^ ^ ^ ^ ^ ^ ^ ^ ^ ^ ^ ^ ^ I ^ European Patent Office Office europeen des brevets EP 0 689 847 A1 EUROPEAN PATENT APPLICATION (43) Date of publication: (51 ) |nt CIA A61 M 5/31 5 03.01.1996 Bulletin 1996/01 (21) Application number: 95304415.3 (22) Date of filing: 23.06.1995 (84) Designated Contracting States: (72) Inventor: Watts, Lennox O. BE DE ES FR GB IT NL SE Bronx, New York 10466 (US) (30) Priority: 01.07.1994 US 269719 (74) Representative: Ruffles, Graham Keith London WC2A 3LS (GB) (71) Applicant: Becton Dickinson and Company Franklin Lakes, New Jersey 07417-1880 (US) (54) Syringe assembly (57) A syringe assembly (10) includes a barrel (12) and a plunger (40) slidably placed in the barrel (12). The plunger (40) includes a shaft with a distal piston (46). The piston (46) has a distal sealing portion (48) with a distal surface (54) including a central section (56) and an out- side section (58) and a guide portion (50). The sealing portion (48) has an outside diameter greater than the in- side diameter of the barrel before the piston is placed in the barrel. The sealing portion (48) has a groove (62) in the distal surface (54) where the central section (56) flex- ibly joins the outside section (58). When the piston (46) is placed in the barrel (1 2), the outside section ((58) con- tacts the barrel wall distally, deflecting the outside sec- tion (58) with respect to the central sectionpart.� (56), forming a fluid tight seal with the barrel wall for facilitating drawing and expelling fluid with movement of the piston (46). -

DESIGN ESSENTIALS for 3D Printing Design Essentials for 3D Printing
DESIGN ESSENTIALS for 3D Printing Design Essentials for 3D Printing Industrial 3D printing opens up many new design possibilities, but it’s important to keep a few Contents fundamental principles in mind when designing for additive manufacturing processes. Most of these are 03 Rapid Prototyping with Stereolithography fairly obvious like feature resolution, surface finish, and material selection, but there’s more to 3D printing 06 Prototyping with PolyJet 3D Printing success than selecting the right material and process. If you will eventually need increased part quantities 08 3D Printing Fully Functional Parts with through more traditional processes like injection molding, Selective Laser Sintering you should considering the part’s moldability even 11 How to Use Multi Jet Fusion for Functional when designing early prototypes. Understanding the 3D-Printed Parts fundamental principles for 3D printing will help you get the most out the versatile technology—whether you're 14 The Basics of Metal 3D Printing Part Design iterating part design through rapid prototyping or creating end-use production parts. Got a 3D CAD model ready to be quoted? Upload it today for an instant quote. GET INSTANT QUOTE © Proto Labs, Inc. 1999–2018 Protolabs HQ, 5540 Pioneer Creek Dr., Maple Plain, MN 55359 USA | 877-479-3680 2 Design Essentials for 3D Printing Rapid Prototyping with Stereolithography 3 1 Stereolithography, or SLA, emerged in the 2 mid-1980s and established itself as a staple of additive manufacturing (now known as 3D printing) over the next decade. Since that 10 time, SL’s ability to quickly and accurately create 6 complex prototypes has helped transform the design world like never before. -

Investigation of Traditional and Alternate Living Hinge Designs for Fused Deposition Modeling Additive Manufacturing Process
Dissertations and Theses 8-2014 Investigation of Traditional and Alternate Living Hinge Designs for Fused Deposition Modeling Additive Manufacturing Process Cassandra Sue Gribbins Follow this and additional works at: https://commons.erau.edu/edt Part of the Mechanical Engineering Commons Scholarly Commons Citation Gribbins, Cassandra Sue, "Investigation of Traditional and Alternate Living Hinge Designs for Fused Deposition Modeling Additive Manufacturing Process" (2014). Dissertations and Theses. 213. https://commons.erau.edu/edt/213 This Thesis - Open Access is brought to you for free and open access by Scholarly Commons. It has been accepted for inclusion in Dissertations and Theses by an authorized administrator of Scholarly Commons. For more information, please contact [email protected]. INVESTIGATION OF TRADITIONAL AND ALTERNATE LIVING HINGE DESIGNS FOR FUSED DEPOSITION MODELING ADDITIVE MANUFACTURING PROCESS by Cassandra Sue Gribbins A Thesis Submitted to the College of Engineering Department of Mechanical Engineering in Partial Fulfillment of the Requirements for the Degree of Master of Science in Mechanical Engineering Embry-Riddle Aeronautical University Daytona Beach, Florida August 2014 i Acknowledgements My sincere gratitude goes to Dr. Heidi M. Steinhauer and Mr. Raul Rumbaut for the support and guidance as well as keeping me focused with the much needed reminder to just “Finish it!” I would not be where I am at today without your mentorship and care. I am also very grateful for all of the help and direction from Dr. Sypeck and Mr. Potash with the material testing. Thank you as well to Dr. Rollin and Dr. Dhainaut for the feedback and guidance. I would also like to thank my “pamily” for providing laughter and pep talks throughout the process. -

WO 2013/116763 Al 8 August 2013 (08.08.2013) P O P CT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/116763 Al 8 August 2013 (08.08.2013) P O P CT (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every B32B 27/20 (2006.01) C08L 67/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 13/024487 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 1 February 2013 (01 .02.2013) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, (26) Publication Language: English RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (30) Priority Data: ZM, ZW. 61/594,638 3 February 2012 (03.02.2012) US (84) Designated States (unless otherwise indicated, for every (71) Applicant (for all designated States except US): ECO- kind of regional protection available): ARIPO (BW, GH, SPAN USA [US/US]; 300 Drakes Landing, Suite 200, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, Greenbrae, California 94904 (US). -
PP/TPO Processing Guidelines and Troubleshooting Guide
PP/TPO Processing Guidelines and Troubleshooting Guide This guideline provides valuable information to help with some of the many problems that may arise when working with polypropylene. The suggestions and material supplied should be considered as general guidelines. Each part has to be designed with its end use requirements in mind. If additional information is needed, please contact a process engineer. 6/1/2007 ACP (2007) All Rights Reserved Advanced Composites TS Group Table of Contents PP/TPO Characteristics High Temperature Resistance Low Density UV Resistance Chemical Resistance Other Part Design Wall Thickness Ribs Radii Undercuts Holes Draft Living Hinge Mold Design Manifold Type Gate Geometry Gate Location Venting Mold Cooling Requirements Cores (Holes) Part Ejection Requirements Molding Parts with PP/TPO Machine Specifications Start up molding conditions Optimizing the process Mold Cooling Material Mixing Gating Troubleshooting common molding problems Short Shots Sinks Splay Color streaks Tiger striping Flash Bubbles Voids Poor weld line strength Brittleness Gate Blush Gloss differences ACP (2007) All Rights Reserved Advanced Composites TS Group Introduction: Advanced Composites (ACP) is a world class PP/TPO compound supplier to the Automotive Industry. These materials meet the ever-demanding needs of the automotive interior and exterior communities. This guideline will give you an understanding of the possibilities and requirements of ACP materials. Baseline processing parameters and design guidelines will also be provided. Please utilize our Technical Service Department for more detailed information. PP/TPO Characteristics High Temperature Resistance Polypropylenes relatively high melting point of 335°F allows continued use at temperatures up to 220°F with the material softening at 235°F. -

Pandemic Preparedness
Your Partner In Safety -Since 1979- • Disposable Clothing • Respiratory PANDEMIC Protection • Eye Protection PREPAREDNESS • Disinfectants • OTC Medications Pandemic Preparedness Novel Coronavirus (nCoV) Infection Overview The Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) are closely monitoring an outbreak caused by a novel (new) coronavirus first identified in Wuhan, Hubei Province, China. Chinese authorities iden- tified the new coronavirus, which has resulted in hundreds of confirmed cases in China, including cases outside Wuhan, with additional cases being identified in a growing number of countries internationally. These numbers will likely grow given the high amount of travel associated with the Lunar New Year holiday. It has been confirmed that the virus can spread from human to human although specific routes of transmission (i.e. airborne, direct contact, ingestion, etc.) have yet to be definitively determined. Common symptoms include runny nose, headache, cough, sore throat, fever, and a general feeling of being unwell. The CDC is providing the following precautions for health care providers: “Healthcare providers should obtain a detailed travel history for patients with fever and respiratory symptoms. For pa- tients who traveled to Wuhan on or after December 1, 2019 and had onset of illness within 2 weeks of leaving, consider the novel coronavirus outbreak in China when evaluating a patient with these symptoms and notify infection control per- sonnel and your local health department immediately. Although routes of transmission have yet to be definitively determined, CDC recommends a cautious approach to inter- acting with patients under investigation. As of March 2020 ask such patients to use respiratory protection (i.e., a respira- tor) that is at least as protective as a fit-tested NIOSH-certified disposable N95 filtering facepiece respirator before entry into the patient room or care area as soon as they are identified. -

CORTINA-CATALOG.Pdf
CONTENTS A-FRAME BARRIER SYSTEMS . .. 12-13 COMPLETE WORK-ZONE SOLUTIONS BANNERS . 49 BARGARD COVERS . .. 53 What’s your WORK-ZONE? BARRICADE SYSTEMS . 19 Whether the WORK-ZONE is along a stretch of highway, BARRICADE LIGHTS . 20-21 providing roadside assistance, running a Distribution CHANNELIZER CONES . 26 complex, managing parking facilities, protecting CHANNELIZER DRUM . 27 pedestrians or working on a construction site, no other CONES SIGNS . 35-36 manufacturer is as vertically integrated or has the product range that we offer. At Cortina we have assembled the DELINEATOR POSTS . 22-24 industry’s most complete line of products from Warning FENCING . 47 Triangles to Rebar Caps. FLEET SAFETY KITS . 3-4 FUSEE KITS AND HOLDERS . 5 Manufacturing is at the CORE of our WORK-ZONE. GRIP N GO TRAILBLAZER . 25 As a U.S. based manufacturer, serving the NAFTA market I-BEAMS AND T-BOARDS . 14-15 our WORK-ZONE starts with a vertically integrated US based manufacturing and distribution HUB located at LAMBA CONES & FLOOR stanDS . 28-29 our Headquarters in Franklin Park, Illinois and supported M-CADES . 8-9 around the world, with complete manufacturing N-CADE SYSTEMS . 16 capabilities including; Plastic Processing, Laminating, paCK N POP CONES . 30 Screen Printing, as well as fabrication. parkinG BLOCKS . 50 Since 1969 Cortina has been committed to exceeding PENNANTS . 48 customer expectations, today our manufacturing PLASTX BARRICADES . 6-7 facilities and Distribution Centers are positioned to meet QUICK DEPLOY batONS . 46 your needs from basic product to customized solutions, REFLECTIVE PRODUCTS . 49 we are your ONE STOP safety products provider for all ROLL UP SIGNS .