Bladder Management Options Following Spinal Cord Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Suplento1 Volumen 71 En
S1 Volumen 71 Mayo 2015 Revista Española de Vol. 71 Supl. 1 • Mayo 2015 Vol. Clínica e Investigación Órgano de expresión de la Sociedad Española de SEINAP Investigación en Nutrición y Alimentación en Pediatría Sumario XXX CONGRESO DE LA SOCIEDAD espaÑOLA DE CUIDADOS INTENSIVOS PEDIÁTRICOS Toledo, 7-9 de mayo de 2015 MESA REDONDA: ¿HACIA DÓNDE VAMOS EN LA MESA REDONDA: EL PACIENTE AGUDO MONITORIZACIÓN? CRONIFICADO EN UCIP 1 Monitorización mediante pulsioximetría: ¿sólo saturación 47 Nutrición en el paciente crítico de larga estancia en UCIP. de oxígeno? P. García Soler Z. Martínez de Compañón Martínez de Marigorta 3 Avances en la monitorización de la sedoanalgesia. S. Mencía 53 Traqueostomía, ¿cuándo realizarla? M.A. García Teresa Bartolomé y Grupo de Sedoanalgesia de la SECIP 60 Los cuidados de enfermería, ¿un reto? J.M. García Piñero 8 Avances en neuromonitorización. B. Cabeza Martín CHARLA-COLOQUIO SESIÓN DE PUESTA AL DÍA: ¿ES BENEFICIOSA LA 64 La formación en la preparación de las UCIPs FLUIDOTERAPIA PARA MI PACIENTE? españolas frente al riesgo de epidemias infecciosas. 13 Sobrecarga de líquidos y morbimortalidad asociada. J.C. de Carlos Vicente M.T. Alonso 68 Lecciones aprendidas durante la crisis del Ébola: 20 Estrategias de fluidoterapia racional en Cuidados experiencia del intensivista de adultos. J.C. Figueira Intensivos Pediátricos. P. de la Oliva Senovilla Iglesias 72 El niño con enfermedad por virus Ébola: un nuevo reto MESA REDONDA: INDICADORES DE CALIDAD para el intensivista pediátrico. E. Álvarez Rojas DE LA SECIP 23 Evolución de la cultura de seguridad en UCIP. MESA REDONDA: UCIP ABIERTAS 24 HORAS, La comunicación efectiva. -

Distance Learning Program Anatomy of the Human Brain/Sheep Brain Dissection
Distance Learning Program Anatomy of the Human Brain/Sheep Brain Dissection This guide is for middle and high school students participating in AIMS Anatomy of the Human Brain and Sheep Brain Dissections. Programs will be presented by an AIMS Anatomy Specialist. In this activity students will become more familiar with the anatomical structures of the human brain by observing, studying, and examining human specimens. The primary focus is on the anatomy, function, and pathology. Those students participating in Sheep Brain Dissections will have the opportunity to dissect and compare anatomical structures. At the end of this document, you will find anatomical diagrams, vocabulary review, and pre/post tests for your students. The following topics will be covered: 1. The neurons and supporting cells of the nervous system 2. Organization of the nervous system (the central and peripheral nervous systems) 4. Protective coverings of the brain 5. Brain Anatomy, including cerebral hemispheres, cerebellum and brain stem 6. Spinal Cord Anatomy 7. Cranial and spinal nerves Objectives: The student will be able to: 1. Define the selected terms associated with the human brain and spinal cord; 2. Identify the protective structures of the brain; 3. Identify the four lobes of the brain; 4. Explain the correlation between brain surface area, structure and brain function. 5. Discuss common neurological disorders and treatments. 6. Describe the effects of drug and alcohol on the brain. 7. Correctly label a diagram of the human brain National Science Education -

Power Wheelchair Alternative Drive Controls in Spinal Cord Injury
Power Wheelchair Alternative Drive Controls in Spinal Cord Injury Kristen Cezat, PT, DPT, NCS, ATP/SMS When a person with a spinal cord injury is unable to use a standard joystick on a Fact Sheet power wheelchair, an alternative drive control and location is required. Depending on the person’s level of injury and musculature that remains innervated, the more common locations of alternative drive control input devices include the head, neck, face, eyes, and tongue. A proportional drive control allows the wheelchair’s speed/direction to mirror the force/direction applied to the input device by the user, most often through a joystick. Proportional drive control options include1: • Standard Joystick: able to move in any direction at any speed. It is often the most intuitive device for adults with injuries at C5 and below. Joysticks are commonly located on either left or right arm rest but can be altered for Produced by location in midline if spasticity or contracture limits neutral shoulder/elbow alignment. • Alternative Joystick (often set at the user’s chin): joysticks vary in size and require less force and deflection to activate the joystick.1 air Drive ControlA non -Optionsproportional drive for control Clients uses commands with to turn on/offSpinal various functionsCord such as direction (forward, back, left, or right) of the wheelchair. Speed is predetermined and not variable to the strength of the command provided. Non- Injury proportional drive controls include1,2: a Special Interest • Sip-and-Puff Group of • Head Array • Head Array/Sip-and-Puff Combo Non-proportional drive controls can be either momentary or latched. -

Basic Brain Anatomy
Chapter 2 Basic Brain Anatomy Where this icon appears, visit The Brain http://go.jblearning.com/ManascoCWS to view the corresponding video. The average weight of an adult human brain is about 3 pounds. That is about the weight of a single small To understand how a part of the brain is disordered by cantaloupe or six grapefruits. If a human brain was damage or disease, speech-language pathologists must placed on a tray, it would look like a pretty unim- first know a few facts about the anatomy of the brain pressive mass of gray lumpy tissue (Luria, 1973). In in general and how a normal and healthy brain func- fact, for most of history the brain was thought to be tions. Readers can use the anatomy presented here as an utterly useless piece of flesh housed in the skull. a reference, review, and jumping off point to under- The Egyptians believed that the heart was the seat standing the consequences of damage to the structures of human intelligence, and as such, the brain was discussed. This chapter begins with the big picture promptly removed during mummification. In his and works down into the specifics of brain anatomy. essay On Sleep and Sleeplessness, Aristotle argued that the brain is a complex cooling mechanism for our bodies that works primarily to help cool and The Central Nervous condense water vapors rising in our bodies (Aristo- tle, republished 2011). He also established a strong System argument in this same essay for why infants should not drink wine. The basis for this argument was that The nervous system is divided into two major sec- infants already have Central nervous tions: the central nervous system and the peripheral too much moisture system The brain and nervous system. -

Minnesotan Invented Life-Saving Catheter « Access Press
Access Press - Minnesota's Disability Community Newspaper Minnesotan invented life-saving catheter by Jane McClure // June 10th, 2011 A medical device which has made life easier for countless people with disabilities and illness has ties to Minnesota. The Foley catheter was invented by St. Cloud native Frederic Foley. A Foley catheter is a flexible tube that is passed through the urethra and into the bladder. The tube has two separated lumens. One lumen is open at both ends, and allows urine to drain out into a collection bag. The other lumen has a valve on the outside end and connects to a balloon at the tip. The balloon is inflated with sterile saline when it lies inside the bladder, in order to stop it from slipping out. Born in St. Cloud in 1891, Foley earned his bachelor’s degree at Yale University, and then attended Johns Hopkins School of Medicine. After graduating from medical school in 1918, Foley worked on the East Coast. He was on the junior surgical staff at Boston’s Peter Brigham Hospital. He was certified by the American Board of Urology in 1937, although several histories note that there are no records of Foley having formal training in urology. He worked as an urologist in Boston until becoming chief of urology at Ancker Hospital in St. Paul. Ancker later became St. Paul-Ramsey Medical Center and is now Regions Hospital. Ancker Hospital was located on the Mississippi River bluff in St. Paul’s West End neighborhood. The site is now occupied by St. Paul Public Schools administration. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

HSOA Archives of Urology a Pilot Study of Foley Catheter Balloon Volumes and Pullout Forces in Females Cadavers
Greenberg JA and Ito TE, Arch Urol 2018 1: 002 HSOA Archives of Urology Pilot Study A Pilot Study of Foley Catheter Introduction Indwelling Foley catheters are used around the world in every Balloon Volumes and Pullout healthcare setting as a means for draining the bladder. Simplified, the Foley catheter is a flexible, hollow tube with an inflatable balloon on Forces in Females Cadavers the indwelling end that functions to keep the catheter from falling James A Greenberg1* and Traci E Ito2 out after it has been placed into the bladder. Despite the ubiquity of this device, the scientifically derived data regarding its use is limited. 1Harvard Medical School, Brigham & Women’s Hospital, Boston, USA As one example, manufacturer guidelines for use of a 16 Fr Foley 2Department of Minimally Invasive Gynecology Surgery, University of catheter with a 5 mL balloon recommends filling the balloon with Louisville Hospital, Louisville, USA 10 mL of sterile water [1]. The 10 mL inflation volume has become an almost universal standard though it is unclear on how this recom- mendation was derived. A search of the literature revealed only one study investigating balloon fill volumes and pull out forces [2]. This study was performed with three male cadavers. While these data may seem trivial, unnecessarily high catheter balloon volumes may influ- ence catheter-associated patient discomfort, leakage around catheter, catheters related trauma to bladder mucosa or urethra, and possibly Catheter-Associated Urinary Tract Infections (CAUTI’s). While the most effective method of reducing Foley catheter relat- Abstract ed complications is by avoiding unnecessary placement, this cannot always be prevented. -

Catheter Associated Urinary Tract Infection (CAUTI) Prevention
Catheter Associated Urinary Tract Infection (CAUTI) Prevention System CAUTI Prevention Team 1 Objectives At the end of this module, the participant will be able to: Identify risk factors for CAUTI Explain the relationship between catheter duration and CAUTI risk List the appropriate indications for urinary catheter insertion and continued use Implement evidence-based nursing practice to decrease the risk and incidence of CAUTI 2 The Problem All patients with an indwelling urinary catheter are at risk for developing a CAUTI. CAUTI increases pain and suffering, morbidity & mortality, length of stay, and healthcare costs. Appropriate indwelling catheter use can prevent about 400,000 infections and 9,000 deaths every year! (APIC, 2008; Gould et al, 2009) 3 2012 National Patient Safety Goal Implement evidence-based practices to prevent indwelling catheter associated urinary tract infections (CAUTI) Insert indwelling urinary catheters according to evidence-based guidelines Limit catheter use and duration Use aseptic technique for site preparation, equipment, and supplies (The Joint Commission (TJC), 2011) 4 2012 National Patient Safety Goal Manage indwelling urinary catheters according to evidence-based guidelines Secure catheters for unobstructed urine flow and drainage Maintain the sterility of the urine collection system Replace the urine collection system when required Collect urine samples using aseptic technique (TJC, 2011) 5 Sources of CAUTI Microorganisms Endogenous Meatal, rectal, or vaginal colonization Exogenous -

Pediatric Shock
REVIEW Pediatric shock Usha Sethuraman† & Pediatric shock accounts for significant mortality and morbidity worldwide, but remains Nirmala Bhaya incompletely understood in many ways, even today. Despite varied etiologies, the end result †Author for correspondence of pediatric shock is a state of energy failure and inadequate supply to meet the metabolic Children’s Hospital of Michigan, Division of demands of the body. Although the mortality rate of septic shock is decreasing, the severity Emergency Medicine, is on the rise. Changing epidemiology due to effective eradication programs has brought in Carman and Ann Adams new microorganisms. In the past, adult criteria had been used for the diagnosis and Department of Pediatrics, 3901 Beaubien Boulevard, management of septic shock in pediatrics. These have been modified in recent times to suit Detroit, MI 48201, USA the pediatric and neonatal population. In this article we review the pathophysiology, Tel.: +1 313 745 5260 epidemiology and recent guidelines in the management of pediatric shock. Fax: +1 313 993 7166 [email protected] Shock is an acute syndrome in which the circu- to generate ATP. It is postulated that in the face of latory system is unable to provide adequate oxy- prolonged systemic inflammatory insult, overpro- gen and nutrients to meet the metabolic duction of cytokines, nitric oxide and other medi- demands of vital organs [1]. Due to the inade- ators, and in the face of hypoxia and tissue quate ATP production to support function, the hypoperfusion, the body responds by turning off cell reverts to anaerobic metabolism, causing the most energy-consuming biophysiological acute energy failure [2]. -

Neurogenic Erectile Dysfunction. Where Do We Stand?
medicines Review Neurogenic Erectile Dysfunction. Where Do We Stand? Charalampos Thomas 1,* and Charalampos Konstantinidis 2 1 Urology Department, General Hospital of Corinth, 20131 Corinth, Greece 2 Urology & Neurourology Unit, National Rehabilitation Center, Ilion, 13122 Athens, Greece; [email protected] * Correspondence: [email protected] Abstract: Erectile Dysfunction (ED) is the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance, causing tremendous effects on both patients and their partners. The pathophysiology of ED remains a labyrinth. The underlying mechanisms of ED may be vasculogenic, neurogenic, anatomical, hormonal, drug-induced and/or psychogenic. Neurogenic ED consists of a large cohort of ED, accounting for about 10% to 19% of all cases. Its diversity does not allow an in-depth clarification of all the underlying mechanisms nor a “one size fits all” therapeutical approach. In this review, we focus on neurogenic causes of ED, trying to elucidate the mechanisms that lie beneath it and how we manage these patients. Keywords: erectile dysfunction (ED); neurogenic; sexual dysfunction (SD); phosphodiesterase type-5 inhibitors (PDE5I); spinal cord injury (SCI); multiple sclerosis (MS) 1. Introduction Erectile dysfunction (ED) is defined as the persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance [1]. Besides the obvious, it has tremendous effects on the patient’s psychosocial health, and it affects not only their quality of life but the lives of their partners [2]. Citation: Thomas, C.; Konstantinidis, The pathophysiology of ED remains a labyrinth since many pathways can co-exist, C. Neurogenic Erectile Dysfunction. thus contributing negatively. Where Do We Stand? Medicines 2021, Traditionally ED was divided into three large cohorts, organic, psychogenic and of 8, 3. -
Mechanical Ventilation Guide
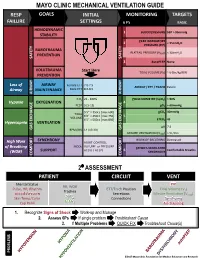
MAYO CLINIC MECHANICAL VENTILATION GUIDE RESP GOALS INITIAL MONITORING TARGETS FAILURE SETTINGS 6 P’s BASIC HEMODYNAMIC 1 BLOOD PRESSURE SBP > 90mmHg STABILITY PEAK INSPIRATORY 2 < 35cmH O PRESSURE (PIP) 2 BAROTRAUMA PLATEAU PRESSURE (P ) < 30cmH O PREVENTION PLAT 2 SAFETY SAFETY 3 AutoPEEP None VOLUTRAUMA Start Here TIDAL VOLUME (V ) ~ 6-8cc/kg IBW PREVENTION T Loss of AIRWAY Female ETT 7.0-7.5 AIRWAY / ETT / TRACH Patent Airway MAINTENANCE Male ETT 8.0-8.5 AIRWAY AIRWAY FiO2 21 - 100% PULSE OXIMETRY (SpO2) > 90% Hypoxia OXYGENATION 4 PEEP 5 [5-15] pO2 > 60mmHg 5’5” = 350cc [max 600] pCO2 40mmHg TIDAL 6’0” = 450cc [max 750] 5 VOLUME 6’5” = 500cc [max 850] ETCO2 45 Hypercapnia VENTILATION pH 7.4 GAS GAS EXCHANGE BPM (RR) 14 [10-30] GAS EXCHANGE MINUTE VENTILATION (VMIN) > 5L/min SYNCHRONY WORK OF BREATHING Decreased High Work ASSIST CONTROL MODE VOLUME or PRESSURE of Breathing PATIENT-VENTILATOR AC (V) / AC (P) 6 Comfortable Breaths (WOB) SUPPORT SYNCHRONY COMFORT COMFORT 2⁰ ASSESSMENT PATIENT CIRCUIT VENT Mental Status PIP RR, WOB Pulse, HR, Rhythm ETT/Trach Position Tidal Volume (V ) Trachea T Blood Pressure Secretions Minute Ventilation (V ) SpO MIN Skin Temp/Color 2 Connections Synchrony ETCO Cap Refill 2 Air-Trapping 1. Recognize Signs of Shock Work-up and Manage 2. Assess 6Ps If single problem Troubleshoot Cause 3. If Multiple Problems QUICK FIX Troubleshoot Cause(s) PROBLEMS ©2017 Mayo Clinic Foundation for Medical Education and Research CAUSES QUICK FIX MANAGEMENT Bleeding Hemostasis, Transfuse, Treat cause, Temperature control HYPOVOLEMIA Dehydration Fluid Resuscitation (End points = hypoxia, ↑StO2, ↓PVI) 3rd Spacing Treat cause, Beware of hypoxia (3rd spacing in lungs) Pneumothorax Needle D, Chest tube Abdominal Compartment Syndrome FLUID Treat Cause, Paralyze, Surgery (Open Abdomen) OBSTRUCTED BLOOD RETURN Air-Trapping (AutoPEEP) (if not hypoxic) Pop off vent & SEE SEPARATE CHART PEEP Reduce PEEP Cardiac Tamponade Pericardiocentesis, Drain. -

Urological Supplies Requirements
Pharmacy & Medical Supplies Urological Supplies DOCUMENTATION IN MEDICAL RECORDS REQUIRED BY CMS Documentation Requirements Key Items to Address Duration of patient’s condition Why does the patient require the item? Clinical course Do the physical examination findings support the need for the item? Prognosis Signs and symptoms that indicate the need for the item Nature and extent of functional limitations Diagnoses that are responsible for these signs and symptoms Other therapeutic interventions and results Other diagnoses that may relate to the need for the item Medical records should contain: Urinary catheters and external urinary collection devices Medical records support the beneficiary has permanent urinary incontinence or permanent urinary retention that is not expected to be medically or surgically corrected within 3 months Indwelling catheters (A4311 – A4316, A4338 – A4346) No more than one catheter per month for routine catheter maintenance Non-routine indwelling catheter changes are covered for the following indications: • Catheter is accidentally removed (e.g., pulled out by beneficiary) • Malfunction of catheter (e.g., balloon does not stay inflated, hole in catheter) • Catheter is obstructed by encrustation, mucous plug, or blood clot • History of recurrent obstruction or urinary tract infection for which it has been established that an acuteevent is s prevented by a scheduled change frequency of more than once per month Specialty indwelling catheter (A4340) or all silicone catheter (A4344, A4312, or A4315) Criteria for an