Download As A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Compendium of the Findings of the OPCAST Pandemic Subgroup 12
1 A Compendium of the Findings of the Obama PCAST Ad Hoc Subgroup on Pandemic Preparedness and Response December 23, 2020 Introduction A subset of the former members of President Obama’s Council of Advisors on Science and Technology (here OPCAST)—ten individuals who played particularly important roles in producing the six OPCAST reports between 2009 and 2016 that dealt with issues related to pandemic preparedness and response1—came together starting in March of this year to consider how insights from those studies might be combined with more recent research and current observations to develop suggestions about how the U.S. response to the COVID-19 pandemic could be improved. The Subgroup has produced six reports, addressing • the national strategic pandemic-response stockpile (May 20) • the role of contact tracing (June 18) • the role of public health data in controlling the spread of COVID-19 (July 28) • testing for the pathogen (August 18) • recommendations for the coming COVID-19 commission (September 21) • needs for improved epidemiological modeling (September 28) Each report was distributed, upon completion, to selected members of the Trump COVID-19 team and the Biden campaign staff, selected governors and members of Congress, selected public health experts outside government, and the media. The reports have also been posted on the OPCAST team’s website, http://opcast.org, together with a few opinion pieces based on them. In the current volume, we have assembled all six reports in full, preceded by a set of brief summaries. Four of the reports are followed by short updates taking account of developments since the reports first came out. -

INSIDE THIS ISSUE EXCLUSIVE Anthony Adams Kizzmekia Corbett
Feb/Mar, 2021 SMART PAGES SINCE 2006 DBUSINESSETR - POLITICS OI- COMMUNITYT “Building Business to Business and Business to Community Relationships” INSIDE THIS ISSUE EXCLUSIVE Anthony Adams Why I want to be Everyone’s Mayor in Detroit pg. 11 Kizzmekia Corbett Lead Scientific Researcher, Coronavirus Vaccine pg. 4 www.detroitsmartpages.com | [email protected] Commonly asked questions about COVID-19 VACCINES 1. What are the differences and second time, it really develops that (LNP) carrier, essential for efficient vaccine at an alternate site. similarities between the Moderna full, long term memory. delivery of the mRNA, were FDA If you have ever had a severe and Pfizer vaccines? 4. What are the common side approved only a couple years ago. reaction to the Pfizer or Moderna • Both vaccines are about 95% ef- effects of the vaccine? Additional vaccines for rabies, Zika COVID-19 vaccines, or any of their fective. Pfizer and Moderna had a The most common side effects and influenza remain under devel- components, you cannot receive fair and comparable spread of races that have been reported with the opment and it is likely we will see the vaccine. and ethnicities included in the clin- COVID-19 vaccine include: other mRNA vaccines approved in • If you have had an anaphylactic ical trials. There does not appear • Injection site pain the near future. reaction to any vaccine or in- to be any significant differences in • Tiredness 8. Will this be a once a year vaccine jectable, you cannot receive the vaccine effectiveness between the • Headache or once you have both doses will it COVID-19 vaccine at Beaumont at two brands. -

January 11, 2021 Anthony Shadid Award for Journalism Ethics, Center
January 11, 2021 Anthony Shadid Award for Journalism Ethics, Center for Journalism Ethics at the University of Wisconsin-Madison, School of Journalism and Mass Communication 5115 Vilas Hall, 821 University Avenue Madison, WI 53706 Dear Shadid Award judges: Alaska has the highest rate of sexual assault and child sex abuse in the U.S. Yet for generations it has been an unspoken epidemic. Predators assume, often correctly, that victims will keep their secrets. The “Unheard” project shattered that silence with a new kind of collaborative journalism rooted in trust and respect for 29 Alaskans who have stepped forward to share their stories. The series is a centerpiece of the ongoing investigation into sexual violence Alaska by ProPublica and the Anchorage Daily News. Please find the online version of Unheard here: https://features.propublica.org/alaska-sexual-assault/unheard-survivor-stories/ And two front covers of the print edition, which bookended the stories published throughout June 2020, here: https://www.dropbox.com/s/mlhiwdtq5xld82x/ADN_PP_Unheard_FrontPages.pdf?dl=0 In 2018, after a string of particularly gut-wrenching sexual assault and murder cases, the Anchorage Daily News asked readers if they would be willing to share their stories of sexual violence to help us determine why the problem appeared to be getting worse and where the failure points exist within the criminal justice system. More than 200 people responded, most saying they would be willing to speak on the record to a reporter. Often, they told of being sexually abused as children and again and again throughout adulthood. When they reported the crimes, police sometimes failed to investigate or prosecutors declined to file charges. -

J. Michael Mcginnis, Md, Ma, Mpp
J. MICHAEL MCGINNIS, MD, MA, MPP National Academy of Medicine, the National Academies, 500 Fifth Street NW, Washington DC 20001, (202) 334-3963, [email protected] Highlights: Michael McGinnis is a physician and epidemiologist who lives and works in Washington DC. Through his writing, government service, and work in philanthropy, he has been a long-time contributor to national and international field leadership in health, health care, and health policy. He currently serves at the National Academy of Medicine (NAM), where he is the Leonard D. Schaeffer Executive Officer, Senior Scholar, and Executive Director of the NAM’s Leadership Consortium for public and private collaboration on behalf of a continuously learning health system. Previously, he served as founding Director, respectively, of the Robert Wood Johnson Foundation’s (RWJF) Health Group, the World Health Organization’s Office for Health Reconstruction in Bosnia, the federal Office of Research Integrity (interim), and the federal Office of Disease Prevention and Health Promotion. In a tenure unusual for political and policy posts, he held continuous appointment through the Carter, Reagan, Bush and Clinton Administrations at the Department of Health and Human Services, with policy responsibilities for disease prevention and health promotion (1977-1995). Programs and policies conceived and launched at his initiative include the Healthy People process establishing national health goals and objectives (1979-present), the U.S. Preventive Services Task Force (1984-present), the Dietary Guidelines for Americans (with USDA, 1980- present), the multi-level Public Health Functions Steering Group and the Ten Essential Services of Public Health (1994-present), the RWJF Active Living family of programs (2000-present), the RWJF Young Epidemiology Scholars Program (2001-2012), the RWJF Health and Society Scholars Program (2002-2017), and the current Learning Health System initiative of the NAM. -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 Background/Overview .........................................................................................1 -

Minority Percentages at Participating Newspapers
Minority Percentages at Participating Newspapers Asian Native Asian Native Am. Black Hisp Am. Total Am. Black Hisp Am. Total ALABAMA The Anniston Star........................................................3.0 3.0 0.0 0.0 6.1 Free Lance, Hollister ...................................................0.0 0.0 12.5 0.0 12.5 The News-Courier, Athens...........................................0.0 0.0 0.0 0.0 0.0 Lake County Record-Bee, Lakeport...............................0.0 0.0 0.0 0.0 0.0 The Birmingham News................................................0.7 16.7 0.7 0.0 18.1 The Lompoc Record..................................................20.0 0.0 0.0 0.0 20.0 The Decatur Daily........................................................0.0 8.6 0.0 0.0 8.6 Press-Telegram, Long Beach .......................................7.0 4.2 16.9 0.0 28.2 Dothan Eagle..............................................................0.0 4.3 0.0 0.0 4.3 Los Angeles Times......................................................8.5 3.4 6.4 0.2 18.6 Enterprise Ledger........................................................0.0 20.0 0.0 0.0 20.0 Madera Tribune...........................................................0.0 0.0 37.5 0.0 37.5 TimesDaily, Florence...................................................0.0 3.4 0.0 0.0 3.4 Appeal-Democrat, Marysville.......................................4.2 0.0 8.3 0.0 12.5 The Gadsden Times.....................................................0.0 0.0 0.0 0.0 0.0 Merced Sun-Star.........................................................5.0 -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Carolina Digital Repository THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 -

Renewing the News
Renewing the News alter Cronkite tion of everyday behavior, stepped to the podium and the vexing cultural and before a respectful audi- political challenges it has ence at Harvard one No- spawned in its unbound- Wvember evening in 1990. ed flood of information. An avuncular legend of broad- Though Cronkite spoke cast journalism, celebrated that evening from the apex as “the most trusted man in of American journalism, he America,” he was an obvious had begun his career at its choice to initiate an annual base: with a local report- lecture series at the Kennedy ing job at The Houston Post. School’s Shorenstein Center In 1990, that base appeared on Media, Politics and Policy. secure. Even in the age of Cronkite shared insider tales television, American news- from the 1950s and ’60s as he papers employed by far described the unfortunate ef- the most journalists and fects of television on Ameri- produced by far the most can politics: shallow debates, journalism, especially at shrinking soundbites, image the local level. The indus- over substance. try’s most profitable year The ninth of 11 questions he would not come until 2000. fielded pointed him toward the And then it collapsed. future. “There is the imminent Long supported by adver- emergence of a digital, global tisers drawn to the audi- information environment with Supporting journalism— ence they commanded, the instantaneous transmis- newspaper publishers sion of information…in many and democracy—after found themselves stunned forms almost anywhere,” his and stumbling across an questioner said. Combined the Internet eviscerated unfamiliar and treacher- with the proliferation of cable ous landscape. -

Genealogy Resources in the Alaska Collection at the Z. J. Loussac Public Library
Genealogy Resources in the Alaska Collection at the Z. J. Loussac Public Library In the Z.J. Loussac Public Library Alaska Collection, one copy of each book stays in the library for reference and research. The call number is preceded by AK-R. If there is a second copy, that book will have an ‘N’ call number and blue dot ● on the spine indicating it may be checked out. Books with AK-RARE preceding the call number are kept in a locked cabinet. Please ask the Alaska Reference Librarian for assistance. Standard Reference Source Alaska Sources: a Guide to Historical Records and Information AK-R 979.8 BRADBUR Resources. Biographical Information Alaska: Who’s Here, What’s Doing, Who’s Doing It. Contains N 920.0798 JEFFERY biographical paragraphs on 500 people living in Alaska in 1955 . Biographies of Alaska-Yukon Pioneers, 1850-1950. A 5-volume AK-R 929.39798 FERRELL work of biographical material from the period of early development of Alaska and the Yukon. The information was gleaned from newspaper obituaries, magazine articles and books; and the articles include the source of the information. Legends & Legacies, Anchorage 1910-1935 . Written by John P. N 979.83504 BAGOY Bagoy about early Anchorage families. Nome and Seward Peninsula: History, Description, Biographies AK-RARE 917.98 HARRISO and Stories by E. S. Harrison (1905). Tewkesbury’s Who’s Who in Alaska and Alaska Business Index. N 920.0798 TEWKESB (1947) “Persons selected for listing are those who maintained a home in the territory and who are notable for worthy achievement.” Who’s Who in Alaskan Politics, a Biographical Dictionary of N 920 ATWOOD Alaskan Political Personalities, 1884-1974. -

Villages Daily Sun Inks Press, Postpress Deals for New Production
www.newsandtech.com www.newsandtech.com September/October 2019 The premier resource for insight, analysis and technology integration in newspaper and hybrid operations and production. Villages Daily Sun inks press, postpress deals for new production facility u BY TARA MCMEEKIN CONTRIBUTING WRITER The Villages (Florida) Daily Sun is on the list of publishers which is nearer to Orlando. But with development trending as winning the good fight when it comes to community news- it is, Sprung said The Daily Sun will soon be at the center of the papering. The paper’s circulation is just over 60,000, and KBA Photo: expanded community. — thanks to rapid growth in the community — that number is steadily climbing. Some 120,000 people already call The Partnerships key Villages home, and approximately 300 new houses are being Choosing vendors to supply various parts of the workflow at built there every month. the new facility has been about forming partnerships, accord- To keep pace with the growth, The Daily Sun purchased a Pictured following the contract ing to Sprung. Cost is obviously a consideration, but success brand-new 100,000-square-foot production facility and new signing for a new KBA press in ultimately depends on relationships, he said — both with the Florida: Jim Sprung, associate printing equipment. The publisher is confident the investment publisher for The Villages Media community The Daily Sun serves and the technology providers will help further entrench The Daily Sun as the definitive news- Group; Winfried Schenker, senior who help to produce the printed product. paper publisher and printer in the region. -

Distribution Agreement in Presenting This Thesis Or Dissertation As A
Distribution Agreement In presenting this thesis or dissertation as a partial fulfillment of the requirements for an advanced degree from Emory University, I hereby grant to Emory University and its agents the non-exclusive license to archive, make accessible, and display my thesis or dissertation in whole or in part in all forms of media, now or hereafter known, including display on the world wide web. I understand that I may select some access restrictions as part of the online submission of this thesis or dissertation. I retain all ownership rights to the copyright of the thesis or dissertation. I also retain the right to use in future works (such as articles or books) all or part of this thesis or dissertation. Signature: _____________________________ ______________ Anita L. Renahan-White Date Faith and the Public's Health By Anita L. Renahan-White Master of Divinity Candler School of Theology ___________________________________________ [Thesis Advisor's signature] Dr. John Blevins Committee Chair ___________________________________________ [Member's signature] Dr. Steven J. Kraftchick Director of General and Advanced Studies ___________________________________________ [Member's signature] Dr. Emmanuel Lartey Committee Member Faith and the Public's Health By Anita L. Renahan-White MPH Emory University 1993 Thesis Committee Chair: John Blevins, ThD An abstract of A thesis submitted to the Faculty of the Candler School of Theology in partial fulfillment of the requirements for the degree of Master of Divinity 2012 Abstract Faith and the Public's Health By Anita L. Renahan-White In the following thesis "Faith and the Public's Health," I detail findings from research and interviews I conducted from March 2011 through February 2012. -
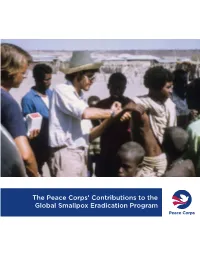
The Peace Corps' Contributions to the Global Smallpox Eradication Program
The Peace Corps’ Contributions to the Global Smallpox Eradication Program About the Office of Strategic Information, Research, and Planning (OSIRP) It is the mission of OSIRP to advance evidence-based management at the Peace Corps by guiding agency strategic planning; monitoring and evaluating agency-level performance and programs; conducting research to generate new insights in the fields of international development, cultural exchange, and Volunteer service; enhancing the stewardship and governance of agency data; and helping to shape agency engagement on high-level, governmentwide initiatives. Front Cover: Peace Corps Volunteers Robert Steinglass and Doug Arbuckle administering the smallpox vaccine in Mille, Ethiopia, in 1974. Photo: Steinglass, personal collection. ii Dedication This report is dedicated to the memory of Dr. Donald Ainslie “D. A.” Henderson (September 7, 1928—August 19, 2016), a seminal figure in the field of smallpox eradication. The Peace Corps is deeply appreciative of having had the opportunity to correspond with Dr. Henderson about the contributions of Peace Corps Volunteers and returned Volunteers within the context of the global eradication program. His charismatic leadership, tireless energy, and unflagging devotion to this program inspired countless public health workers around the world, including many of the returned Peace Corps Volunteers interviewed for this report. iii Acknowledgments In 1806, approximately 10 years after Dr. Edward Jenner conducted the first documented experiment with smallpox vaccination, laying the foundations of modern medicine, President Thomas Jefferson wrote to the English physician and scientist. Jefferson acknowledged the importance of this discovery, extending “a portion of the tribute of gratitude due to you from the whole human family.