CURRICULUM VITAE Hendrik Peter Nicolas Scholl
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
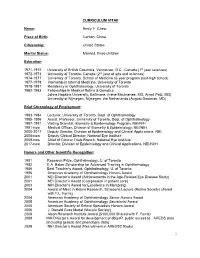
Emily Y. Chew, M.D
CURRICULUM VITAE Name: Emily Y. Chew Place of Birth: Canton, China Citizenship: United States Marital Status: Married, three children Education 1971-1972 University of British Columbia, Vancouver, B.C., Canada (1st year sciences) 1972-1973 University of Toronto, Canada (2nd year of arts and sciences) 1974-1977 University of Toronto, School of Medicine (6-year program post-high school) 1977-1978 Internship in Internal Medicine, University of Toronto 1978-1981 Residency in Ophthalmology, University of Toronto 1982-1983 Fellowships in Medical Retina & Genetics Johns Hopkins University, Baltimore, (Irene Maumenee, MD, Arnall Patz, MD) University of Nijmegen, Nijmegen, the Netherlands (August Deutman, MD) Brief Chronology of Employment: 1983-1984 Lecturer, University of Toronto, Dept. of Ophthalmology 1985-1986 Assist. Professor, University of Toronto, Dept. of Ophthalmology 1987-1991 Visiting Scientist, Biometry & Epidemiology Program, NEI/NIH 1991-now Medical Officer, Division of Biometry & Epidemiology, NEI/NIH 2000-2017 Deputy Director, Division of Epidemiology and Clinical Applications, NEI. 2008-now Deputy Clinical Director, National Eye Institute 2009-now Chief of Clinical Trials Branch, National Eye Institute 2017-now Director, Division of Epidemiology and Clinical Applications, NEI/NIIH Honors and Other Scientific Recognition: 1981 Research Prize, Ophthalmology, U. of Toronto 1982 E.A. Baker Scholarship for Advanced Training in Ophthalmology 1986 Best Teacher’s Award, Ophthalmology, U. of Toronto 1996 American Academy of Ophthalmology Honors Award 2001 NEI Director’s Award (Achievements in the Age-Related Eye Disease Study) 2001 NEI Director’s Award (Compassion in patient care) 2003 NIH Director’s Award for Excellence in Mentoring 2004 Award of Merit in Retina Research, Schepens Lecture (Retina Society) shared with F.L. -
Copyright and Use of This Thesis This Thesis Must Be Used in Accordance with the Provisions of the Copyright Act 1968
COPYRIGHT AND USE OF THIS THESIS This thesis must be used in accordance with the provisions of the Copyright Act 1968. Reproduction of material protected by copyright may be an infringement of copyright and copyright owners may be entitled to take legal action against persons who infringe their copyright. Section 51 (2) of the Copyright Act permits an authorized officer of a university library or archives to provide a copy (by communication or otherwise) of an unpublished thesis kept in the library or archives, to a person who satisfies the authorized officer that he or she requires the reproduction for the purposes of research or study. The Copyright Act grants the creator of a work a number of moral rights, specifically the right of attribution, the right against false attribution and the right of integrity. You may infringe the author’s moral rights if you: - fail to acknowledge the author of this thesis if you quote sections from the work - attribute this thesis to another author - subject this thesis to derogatory treatment which may prejudice the author’s reputation For further information contact the University’s Copyright Service. sydney.edu.au/copyright Clinical Studies into the Causes of Idiopathic Macular Telangiectasia Type 2: Sleep Apnoea and Macular Telangiectasia: The SAMTel Project Martin Lee Submitted to the Faculty of Medicine in fulfillment of the requirements of the degree Masters of Philosophy (Medicine) Department of Clinical Ophthalmology & Eye Health University of Sydney January 2015 Acknowledgements: To my family, especially parents, Anne and Russell, and siblings Alison and Frances, thank you for your unbridled support and endless encouragement to enable me to continue to pursue my educational interests. -

Macular Telangiectasia Type 2: Quantitative Analysis of a Novel
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UCL Discovery Macular telangiectasia type 2: quantitative analysis of a novel phenotype and implications for the pathobiology of the disease Mali Okada, MBBS, MMed*; Catherine A Egan, FRANZCO*†; Tjebo FC Heeren, MD*‡; Adnan Tufail, MD, FRCOphth*; Marcus Fruttiger, PhD‡; Peter M Maloca, MD*§ * Moorfields Eye Hospital NHS Foundation Trust, London, UK † Department of Ophthalmology, University of Bonn, Bonn, Germany ‡ UCL Institute of Ophthalmology, London, United Kingdom § Department of Ophthalmology, University of Basel, Basel, Switzerland Short Title: Retinal microcystoid spaces in MacTel 2 Funding: Supported by the Lowy Medical Research Institute, Sydney, Australia as part of The Macular Telangiectasia Project (MO, CE). AT receives a proportion of funding from the National Institute for Health Research (NIHR) and Biomedical Research Centre at Moorfields Eye Hospital and the University College London Institute of Ophthalmology. The views expressed in the publication are those of the authors and not necessarily those of the Department of Health. Financial Disclosures: AT is on the advisory board for Heidelberg engineering (Heidelberg, Germany) and Optovue (Optovue Inc, USA). PM receives fees for lectures from Heidelberg engineering (Heidelberg, Germany) 1 Address for correspondence: Peter M Maloca, MD Moorfields Eye Hospital 162 City Road, London EC1V 2PD London, United Kingdom Tel: +44 20 72533411 Fax: +44 20 72534696 [email protected] Key words Macular telangiectasia type 2; spectral domain optical coherence tomography; volume rendering; microcystoid spaces; cystoid macular oedema; microcystic macular oedema; inner nuclear layer cysts; microcysts; microcavitations Summary Statement Retinal microcystoid spaces are a novel phenotype of Macular Telangiectasia (MacTel) type 2 on optical coherence tomography. -

Genetic Disruption of Serine Biosynthesis Is a Key Driver Of
bioRxiv preprint doi: https://doi.org/10.1101/2020.02.04.934356; this version posted February 5, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Genetic Disruption of Serine Biosynthesis is a Key 2 Driver of Macular Telangiectasia Type 2 Etiology and 3 Progression 4 5 RoBerto Bonelli,1,2 Brendan R E Ansell,1,2 Luca Lotta,3 Thomas Scerri,1,2 Traci E Clemons,4 Irene Leung,5 The 6 MacTel Consortium,6 Tunde Peto,7 Alan C Bird,8 Ferenc Sallo,9 Claudia LangenBerg,3 and Melanie Bahlo*1,2. 7 8 9 1 Department of Medical Biology, The University of Melbourne, 3052, Parkville, Victoria, Australia. 10 2 Population Health and Immunity Division, Walter and Eliza Hall Institute of Medical Research, 3052, Parkville, Victoria, 11 Australia. 12 3 MRC Epidemiology Unit, University of Cambridge, CB2 0SL, Cambridge, UK. 13 4 The EMMES Corporation, Rockville, 20850, Maryland, United States. 14 5 Department of Research and Development, Moorfields Eye Hospital NHS Foundation Trust, EC1V 2PD, London, United 15 Kingdom. 16 6 A list of members and affiliations is provided in Table S8. 17 7 Department of Ophthalmology, Queen’s University, Belfast, BT7 1NN, United Kingdom. 18 8 Inherited Eye Disease, Moorfields Eye Hospital NHS Foundation Trust, EC1V 2PD, London, United Kingdom. 19 9 Department of Ophthalmology, University of Lausanne, Hôpital Ophtalmique Jules-Gonin, Fondation Asile des aveugles, 20 Switzerland. -

Rotational Three-Dimensional OCTA
www.nature.com/scientificreports OPEN Rotational Three-dimensional OCTA: a Notable New Imaging Tool to Characterize Type 3 Macular Neovascularization Enrico Borrelli 1, Riccardo Sacconi 1, Gerd Klose2, Luis de Sisternes3, Francesco Bandello1 & Giuseppe Querques 1* This study explored whether rotational three-dimensional (3D) visualization of optical coherence tomography angiography (OCTA) volume data may yield valuable information regarding type 3 macular neovascularization (MNV). In this retrospective, cross-sectional study, we collected data from 15 eyes (13 patients) with treatment-naïve type 3 MNV in their post-nascent stage and age-related macular degeneration (AMD). Subjects were imaged with the SS-OCT system (PLEX Elite 9000, Carl Zeiss Meditec Inc., Dublin, CA, USA). The OCTA volume data were processed with a prototype volume projection removal algorithm and then analyzed using volumetric visualization techniques in order to obtain a 3D visualization of the region occupied by type 3 MNV. The two-dimensional and three-dimensional OCTA images were investigated. Mean ± SD age was 75.1 ± 7.4 years. BCVA was 0.42 ± 0.21 LogMAR in the study eyes. Considering the cohort of analyzed eyes, on rotational 3D OCTA images, a total of 35 neovascular lesions (vs 22 lesions detected on 2D OCTA images) rising from the deep vascular complex and variably spanning the outer retinal layers and eventually reaching the RPE/sub-RPE space were detected. Nine of 35 lesions had a saccular shape, while the remaining cases had a fliform shape. On rotational 3D OCTA images, these lesions were inclined on the three planes, instead of perpendicular to the RPE/Bruch’s membrane. -

Prevalence and Quantification of Geographic Atrophy Associated With
Downloaded from http://bjo.bmj.com/ on August 18, 2017 - Published by group.bmj.com Clinical science Prevalence and quantification of geographic atrophy associated with newly diagnosed and treatment- naïve exudative age-related macular degeneration Anne Sikorav,1 Oudy Semoun,1 Sandrine Zweifel,2 Camille Jung,3 Mayer Srour,1 Giuseppe Querques,1,4 Eric H Souied1 10–14 ► Additional material is ABSTRACT develop, causing further vision loss. Most published online only. To view Objective To identify and quantify geographic atrophy studies focus on either wet or dry form separately please visit the journal online (GA) associated with neovascular age-related macular and there is a paucity of reports on both forms of (http:// dx. doi. org/ 10. 1136/ bjophthalmol- 2015- 308065). degeneration (AMD) at initial presentation using a AMD concomitantly in the same eye. There are fundus autofluorescence (FAF) semi-automated software recent published data regarding the prevalence of – 1Department of Ophthalmology, and to correlate the results with demographic and GA complicating exudative AMD at diagnosis,14 16 University Paris Est, Centre clinical data. with diverse results. Hospitalier Intercommunal de Creteil, Creteil, France Design Retrospective, observational study. In both atrophic and exudative AMDs, RPE 2Department of Ophthalmology, Methods The study population consisted of treatment- damage may be an important factor for visual loss. University Hospital Zurich, naïve patients with newly diagnosed neovascular AMD. The status of RPE can be studied by blue light Zurich, Switzerland Best-corrected visual acuity, fundus photographs, infrared fundus autofluorescence (FAF) imaging, which is a 3 Clinical Research Center, reflectance, FAF and spectral-domain optical coherence non-invasive imaging method that allows for topo- University Paris Est fl Creteil, Centre Hospitalier tomography were performed, associated with uorescein graphic mapping of lipofuscin distribution in the 17 18 intercommunal de Creteil, and indocyanine green angiographies. -

The Progression of Geographic Atrophy Secondary to Age-Related Macular Degeneration
The Progression of Geographic Atrophy Secondary to Age-Related Macular Degeneration Monika Fleckenstein, MD,1 Paul Mitchell, MD, PhD,2 K. Bailey Freund, MD,3,4 SriniVas Sadda, MD,5,6 Frank G. Holz, MD,1 Christopher Brittain, MBBS,7 Erin C. Henry, PhD,8 Daniela Ferrara, MD, PhD8 Geographic atrophy (GA) is an advanced form of age-related macular degeneration (AMD) that leads to pro- gressive and irreversible loss of visual function. Geographic atrophy is defined by the presence of sharply demarcated atrophic lesions of the outer retina, resulting from loss of photoreceptors, retinal pigment epithelium (RPE), and underlying choriocapillaris. These lesions typically appear first in the perifoveal macula, initially sparing the foveal center, and over time often expand and coalesce to include the fovea. Although the kinetics of GA progression are highly variable among individual patients, a growing body of evidence suggests that specific characteristics may be important in predicting disease progression and outcomes. This review synthesizes current understanding of GA progression in AMD and the factors known or postulated to be relevant to GA lesion enlargement, including both affected and fellow eye characteristics. In addition, the roles of genetic, environ- mental, and demographic factors in GA lesion enlargement are discussed. Overall, GA progression rates reported in the literature for total study populations range from 0.53 to 2.6 mm2/year (median, w1.78 mm2/year), assessed primarily by color fundus photography or fundus autofluorescence (FAF) imaging. Several factors that could inform an individual’s disease prognosis have been replicated in multiple cohorts: baseline lesion size, lesion location, multifocality, FAF patterns, and fellow eye status. -

Improving Anti-VEGF Drugs in the Vitreous by Eda Isil Altiok A
Improving Anti-VEGF Drugs in the Vitreous By Eda Isil Altiok A dissertation submitted in partial satisfaction of the Requirement for the degree of Joint Doctor of Philosophy with UC San Francisco In Bioengineering In the graduate division Of the University of California, Berkeley Committee in charge: Professor Kevin E. Healy, Chair Professor David Schaffer Professor Tejal Desai Professor Anthony Adams Fall 2015 Improving Anti-VEGF Drugs in the Vitreous © 2015 by Eda Isil Altiok University of California, Berkeley Abstract Improving Anti-VEGF Drugs in the Vitreous By Eda Isil Altiok Doctor of Philosophy in Bioengineering University of California, Berkeley Professor Kevin Healy, Chair The work described in this dissertation present a novel technique utilizing multivalent hyaluronic acid bioconjugates with an anti-VEGF protein for improving the action of drugs in the vitreous. This technology, which has shown efficacy both in vitro and in vivo has the potential to enhance the bioactivity of drugs used for treating patients with diseases including diabetic retinopathy, wet AMD and other neovascular diseases of the retina. Chapter 2 described our initial efforts in creating multivalent conjugates of the anti-VEGF protein, sFlt. Before beginning in vivo studies, we wanted to determine what parameters would maximize the bioactivity of mvsFlt. We investigated the use of several HyA molecular weights and valencies of sFlt molecules to HyA chains. The characterization and in vitro experiments were carried out with 6 mvsFlt conjugates of 300 kDa, 650 kDa and 1 MDa molecular weights with feed ratios of 10 sFlt per 1 HyA chain (termed low conjugation ratio (LCR)) and 30 sFlt per 1 HyA chain (termed high conjugation ratio (HCR)). -

Specialist Clinic Referral Guidelines OPHTHALMOLOGY
Specialist Clinic Referral Guidelines OPHTHALMOLOGY COVID-19 Impact — Specialist Clinics As part of Alfred Health’s COVID-19 response plan, from October significant changes have been made to Specialist Clinic (Outpatient) services. All referrals received will be triaged; however, if your patient’s care is assessed as not requiring an appointment within the next three months, the referral may be declined. Where possible, care will be delivered via telehealth (phone or video consultation). Please fax your referral to The Alfred Specialist Clinics on 9076 6938. The Alfred Outpatient Referral Form is available to print and fax. Where appropriate and available, the referral may be directed to an alternative specialist clinic or service. You will be notified when your referral is received. Your referral may be declined if it does not contain essential information required for triage, or if the condition is not appropriate for referral to a public hospital, or is a condition not routinely seen at Alfred Health. The clinical information provided in your referral will determine the triage category. The triage category will affect the timeframe in which the patient is offered an appointment. Referral to Victorian public hospitals is not appropriate for: Review or treatment of neovascular (wet) age-related macular degeneration (AMD) where the patient has already commenced treatment at another facility Early intermediate or geographic atrophy (dry) age-related macular degeneration. If the patient is not willing to have surgical treatment Cataract that does not have a significant impact on the person’s activities of daily living Prior to the person’s vision being corrected with spectacles, contact lenses, or the use of visual aids. -

INHERITED RETINAL DISEASE ¨ Hundreds of Causative Mutations Now Identified ¤ Most Affecting Photoreceptors Or RPE
9/4/18 Hereditary Retinal Diseases Epidemiology ¨ HRDs affect about 1/2000 people worldwide INHERITED RETINAL DISEASE ¨ Hundreds of causative mutations now identified ¤ Most affecting photoreceptors or RPE ¨ Many associated with systemic syndromes Blair Lonsberry, MS, OD, MEd., FAAO ¨ Most cause significant visual disability Professor of Optometry Pacific University College of Optometry [email protected] ! Hereditary Retinal Disease! The Rod/Cone Dichotomy ! Signs and Symptoms Based on Photoreceptors Peripheral (Rod) Diseases Central (Cone) Diseases ! Involved: ¨ Retinitis Pigmentosa family ¨ Achromatopsia ! ¤ Leber’s Congenital Amaurosis ¨ Cone Dystrophy RODS CONES ¨ CSNB • Loss of Night Vision • Decreased Acuity ¨ Oguchi’s ¨ Stargardt’s juvenile • Peripheral Field Loss • Central scotoma macular ¨ Best’s dystrophies • ERG: Scotopic loss • ERG: Photopic loss • VA and color vision affected late • Color Vision Affected •Photosensitivity • Photosensitivity Case History/Entrance Skills Health Assessment 5 6 ¨ 31 YR HM ¨ SLE: ¨ CC: referred from PCP for a possible uveitis ¤ 1+ conjunctival injection in the right eye ¨ LEE: 3 years ago ¤ Anterior chamber: deep and quiet (no cells or flare ¨ PMHx: unremarkable noted in either eye) ¨ Meds: Omega-3 supplements ¨ Entrance VA: 20/30+ OD, OS ¨ IOP: 12 and 11 OD, OS ¨ Refraction: ¨ DFE: see photos ¤ +0.75 -2.50 x 003 6/7.5+ (20/25+) ¤ +0.25 -2.75 x 004 6/7.5+ (20/25+) ¨ All other entrance skills unremarkable except for difficulty doing confrontation visual fields 1 9/4/18 OS 7 OS OD 8 OD Retinitis -

Visual Impairment Age-Related Macular
VISUAL IMPAIRMENT AGE-RELATED MACULAR DEGENERATION Macular degeneration is a medical condition predominantly found in young children in which the center of the inner lining of the eye, known as the macula area of the retina, suffers thickening, atrophy, and in some cases, watering. This can result in loss of side vision, which entails inability to see coarse details, to read, or to recognize faces. According to the American Academy of Ophthalmology, it is the leading cause of central vision loss (blindness) in the United States today for those under the age of twenty years. Although some macular dystrophies that affect younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD). Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called fovea) called drusen between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents or the Rheo Procedure. Advanced AMD, which is responsible for profound vision loss, has two forms: dry and wet. Central geographic atrophy, the dry form of advanced AMD, results from atrophy to the retinal pigment epithelial layer below the retina, which causes vision loss through loss of photoreceptors (rods and cones) in the central part of the eye. -

Polypoidal Choroidal Vasculopathy-Associated Vitreous Haemorrhage Presenting As Hyphema Srikanta Kumar Padhy, Atul Kumar, Rebika Dhiman, Karen Sharma
Images in… BMJ Case Rep: first published as 10.1136/bcr-2018-227547 on 13 December 2018. Downloaded from Polypoidal choroidal vasculopathy-associated vitreous haemorrhage presenting as hyphema Srikanta Kumar Padhy, Atul Kumar, Rebika Dhiman, Karen Sharma Dr Rajendra Prasad Centre for DESCRIPTION Ophthalmic Sciences, All India A 59-year-old Indian male patient presented to our Institute of Medical Sciences, clinic with sudden-onset, painless diminution of New Delhi, Delhi, India vision in the right eye for the last 1 week. Records from previous follow-up (2 months back) showed Correspondence to Dr Srikanta Kumar Padhy, that his vision was 20/200 right eye (OD) and 20/80 srikantkumar. padhy19@ gmail. left eye (OS). He had no known systemic medical com conditions. He was diagnosed as a case of right eye pseudophakia with polypoidal choroidal vascu- Accepted 13 November 2018 lopathy (figure 1A), as evidenced by his previous fundus fluorescein angiography (FFA) (figure 1B), indocyanine green angiography (ICGA) (figure 1C) and swept source optical coherence tomography (SSOCT) (figure 2A,C). He has been on regular follow-up for the same condition for the past 4 years. During the course, he had received four intravitreal antivascular endothelial growth factor (anti-VEGF, aflibercept 2 mg in 0.05 mL) injections, with the last injection being administered 4 months back. On ocular examination, his best-corrected visual acuity was hand movement close to face OD and 20/80 OS. Intraocular pressure was 16 mm Hg OD Figure 2 (A,C) Swept source optical coherence and 14 mm Hg OS. On slit lamp examination, pres- tomography (SSOCT) imaging of the right eye showing ence of hyphema (figure 3A) was noted in the right thumb-shaped pigment epithelial detachment (long eye obscuring the details of the rest of the ante- arrow) with double-layer sign (short arrow).