Traumatic Brain Injury in Boxing and Mixed Martial Arts Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of the Head Injury Patient
Management of the Head Injury Patient William Schecter, MD Epidemilogy • 1.6 million head injury patients in the U.S. annually • 250,000 head injury hospital admissions annually • 60,000 deaths • 70-90,000 permanent disability • Estimated cost: $100 billion per year Causes of Brain Injury • Motor Vehicle Accidents • Falls • Anoxic Encephalopathy • Penetrating Trauma • Air Embolus after blast injury • Ischemia • Intracerebral hemorrhage from Htn/aneurysm • Infection • tumor Brain Injury • Primary Brain Injury • Secondary Brain Injury Primary Brain Injury • Focal Brain Injury – Skull Fracture – Epidural Hematoma – Subdural Hematoma – Subarachnoid Hemorrhage – Intracerebral Hematorma – Cerebral Contusion • Diffuse Axonal Injury Fracture at the Base of the Skull Battle’s Sign • Periorbital Hematoma • Battle’s Sign • CSF Rhinorhea • CSF Otorrhea • Hemotympanum • Possible cranial nerve palsy http://health.allrefer.com/pictures-images/ Fracture of maxillary sinus causing CSF Rhinorrhea battles-sign-behind-the-ear.html Skull Fractures Non-depressed vs Depressed Open vs Closed Linear vs Egg Shell Linear and Depressed Normal Depressed http://www.emedicine.com/med/topic2894.htm Temporal Bone Fracture http://www.vh.org/adult/provider/anatomy/ http://www.bartleby.com/107/illus510.html AnatomicVariants/Cardiovascular/Images0300/0386.html Epidural Hematoma http://www.chestjournal.org/cgi/content/full/122/2/699 http://www.bartleby.com/107/illus769.html Epidural Hematoma • Uncommon (<1% of all head injuries, 10% of post traumatic coma patients) • Located -

The Effectiveness of Kickboxing Techniques and Its Relation to Fights Won by Knockout
ORIGINAL ARTICLE The effectiveness of kickboxing techniques and its relation to fights won by knockout Authors’ Contribution: Tadeusz Ambroży1ABCD, Łukasz Rydzik1ABCD, Andrzej Kędra1BCD, A Study Design 1BD 2DE 2DE 2BCD B Data Collection Dorota Ambroży , Marta Niewczas , Ewa Sobiło , Wojciech Czarny C Statistical Analysis D Manuscript Preparation 1 Faculty of Physical Education and Sport, Institute of Sport, University of Physical Education in Krakow, Krakow, Poland E Funds Collection 2 College of Medical Sciences, Institute of Physical Culture Studies, University of Rzeszow, Rzeszow, Poland Received: 29 December 2019; Accepted: 21 January 2020; Published online: 17 February 2020 AoBID: 13154 Abstract Background and Study Aim: Ratio of fights won is important to kickboxers on professional and amateur levels. Knockout is the most eco- nomical way of winning the fight. The objective of the paper is the effectiveness of kickboxing techniques and their impact on winning the fight by knockout. Material and Methods: There were 156 participants in the study (61 amateurs and 95 professionals). Their total number of fights won by knockout was 188 and the amateur competitions they participated in complied with the K-1 ruleset. Fighters were 19 to 32 years old and their training experience was on the average 7.36 yrs. ±3.24 yrs. The shortest training lasted 3 yrs. and the longest one 18 yrs. The study was conducted using the analysis of vid- eos of professional fights as well as diagnostic survey conducted in a group of amateur fighters. The survey in- cluded questions about training experience and techniques used in a fight won by knockout. -

CHAPTER 165-X-8 Professional Bare
165-X-8-.01. Definitions., AL ADC 165-X-8-.01 Alabama Administrative Code Alabama Athletic Commission Chapter 165-X-8. Professional Bare-Knuckle Boxing Ala. Admin. Code r. 165-X-8-.01 165-X-8-.01. Definitions. Currentness (1) “Applicant” means any persons, corporations, organizations or associations required to be licensed before promoting, holding, organizing, participating in, or competing in a professional boxing match, contest, or exhibition. (2) “Body jewelry” means any tangible object affixed to, through, or around any portion of the contestant's body. (3) “Official” unless otherwise indicated is an exclusive term collectively meaning “judge,” “referee,” “timekeeper,” and “inspectors” (4) “Sanctioning Organization” means a national or international organization generally recognized in the bare-knuckle boxing community and which: ranks bare-knuckle boxers within each weight class; sanctions and approves championship matches in those weight classes; and awards championship status and championship prizes (belts, rings, plaques, etc.) to the winner of those matches. (5) “Special Event” means a bare-knuckle boxing card or bare-knuckle boxing show, which has among its contests a championship match, a pay-per-view or subscription television match, a national televised match, or any other match of significance to boxing in this state as designated by the commission. (6) “The Commission” is reference for the Alabama Athletic Commission. Authors: Dr. John Marshall, Joel R. Blankenship, Larry Bright, Stan Frierson, Shane Sears Credits Statutory Authority: Code of Ala. 1975, § 41-9-1024. History: New Rule: Filed July 16, 2010; effective August 20, 2010. Repealed: Filed December 27, 2013; effective January 31, 2014. New Rule: Published February 28, 2020; effective April 13, 2020. -

Download Power Training: for Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Po
Download: Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power PDF Free [036.Book] Download Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power PDF By J. Barnes Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power you can download free book and read Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power for free here. Do you want to search free download Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power or free read online? If yes you visit a website that really true. If you want to download this ebook, i provide downloads as a pdf, kindle, word, txt, ppt, rar and zip. Download pdf #Power Training: For Combat, MMA, Boxing, Wrestling, Martial Arts, and Self-Defense: How to Develop Knockout Punching Power, Kicking Power, Grappling Power, and Ground Fighting Power | #295499 in eBooks | 2014-07-31 | 2014-07-31 | File type: PDF | |8 of 8 people found the following review helpful.| Excellent Resource | By Let's Read Charles |I would first say that Power Training for Combat is an excellent resource for both beginners and more advanced fighters. -

Mixed Martial Arts Rules for Amateur Competition Table of Contents 1
MIXED MARTIAL ARTS RULES FOR AMATEUR COMPETITION TABLE OF CONTENTS 1. SCOPE Page 2 2. VISION Page 2 3. WHAT IS THE IMMAF Page 2 4. What is the UMMAF Page 3 5. AUTHORITY Page 3 6. DEFINITIONS Page 3 7. AMATEUR STATUS Page 5 8. PROMOTERS & REQUIREMENTS Page 5 9. PROMOTERS INSURANCE Page 7 10. PHYSICIANS AND EMT’S Page 7 11. WEIGN-INS & WEIGHT DIVISIONS Page 8 12. COMPETITORS APPEARANCE& REQUIREMENTS Page 9 13. COMPETITOR’s MEDICAL TESTING Page 10 14. MATCHMAKING APPROVAL Page 11 15. BOUTS, CONTESTS & ROUNDS Page 11 16. SUSPENSIONS AND REST PERIODS Page 12 17. ADMINISTRATION & USE OF DRUGS Page 13 18. JURISDICTION,ROUNDS, STOPPING THE CONTEST Page 13 19. COMPETITOR’s REGISTRATION & EQUIPMENT Page 14 20. COMPETITON AREA Page 16 21. FOULS Page 17 22. FORBIDDEN TECHNIQUES Page 18 23. OFFICIALS Page 18 24. REFEREES Page 19 25. FOUL PROCEDURES Page 21 26. WARNINGS Page 21 27. STOPPING THE CONTEST Page 22 28. JUDGING TYPES OF CONTEST RESULTS Page 22 29. SCORING TECHNIQUES Page 23 30. CHANGE OF DECISION Page 24 31. ANNOUNCING THE RESULTS Page 24 32. PROTESTS Page 25 33. ADDENDUMS Page 26 PROTOCOL FOR COMPETITOR CORNERS ROLE OF THE INSPECTORS MEDICAL HISTORY ANNUAL PHYSICAL OPTHTHALMOLOGIC EXAM PROTOCOL FOR RINGSIDE EMERGENCY PERSONNEL PRE & POST –BOUT MEDICAL EXAM 1 SCOPE: Amateur Mixed Martial Arts [MMA] competition shall provide participants new to the sport of MMA the needed experience required in order to progress through to a possible career within the sport. The sole purpose of Amateur MMA is to provide the safest possible environment for amateur competitors to train and gain the required experience and knowledge under directed pathways allowing them to compete under the confines of the rules set out within this document. -

Endovascular Management of Acute Epidural Hematomas: Clinical Experience with 80 Cases
CLINICAL ARTICLE J Neurosurg 128:1044–1050, 2018 Endovascular management of acute epidural hematomas: clinical experience with 80 cases Carlos Michel A. Peres, MD,1 Jose Guilherme M. P. Caldas, MD, PhD,2 Paulo Puglia Jr., MD,2 Almir F. de Andrade, MD, PhD,3 Igor A. F. da Silva, MD,3 Manoel J. Teixeira, MD, PhD,3 and Eberval G. Figueiredo, MD, PhD3 1Hospital Universitário Francisca Mendes, Manaus; and Divisions of 2Neuroradiology and 3Neurosurgery, University of São Paulo School of Medicine, São Paulo, Brazil OBJECTIVE Small acute epidural hematomas (EDHs) treated conservatively carry a nonmeasurable risk of late en- largement due to middle meningeal artery (MMA) lesions. Patients with EDHs need to stay hospitalized for several days, with neurological supervision and repeated CT scans. In this study, the authors analyzed the safety and efficacy of the embolization of the involved MMA and associated lesions. METHODS The study group consisted of 80 consecutive patients harboring small- to medium-sized EDHs treated by MMA embolization between January 2010 and December 2014. A literature review cohort was used as a control group. RESULTS The causes of head injury were falls, traffic-related accidents (including car, motorcycle, and pedestrian vs vehicle accidents), and assaults. The EDH topography was mainly temporal (lateral or pole). Active contrast leaking from the MMA was seen in 57.5%; arteriovenous fistulas between the MMA and diploic veins were seen in 10%; and MMA pseudoaneurysms were found in 13.6% of the cases. Embolizations were performed under local anesthesia in 80% of the cases, with N-butyl-2-cyanoacrylate, polyvinyl alcohol particles, or gelatin sponge (or a combination of these), obtaining MMA occlusion and complete resolution of the vascular lesions. -

Spontaneous Cervical Spinal Epidural Hematoma
CASE REPORT Spontaneous Cervical Spinal Epidural Hematoma Katie Rinne, MBBS; Sunil Gopisetty, MRCEM A 68-year-old woman presented with sudden-onset right arm and leg weakness, as well as right-sided neck pain. nilateral weakness is a common ED and was a nonsmoker with a normal body presentation with a diverse etiology, mass index. Her family history was signifi- including stroke.1,2 Studies have re- cant for cerebral vascular accidents. U ported a misdiagnosis rate of stroke On arrival at the ED, the patient had a and transient ischemic attack of approxi- blood pressure of 179/95 mm Hg; her other mately 10%.3 This case presents an un- vital signs were normal. On examination, usual stroke mimic where treatment with she had a right-sided hemiplegia, with a 0/5 an anticoagulant could have led to adverse power grading observed for motor strength outcomes. It also highlights the importance for both her right arm and leg. She reported of considering a spontaneous cervical spi- paresthesia in dermatomes C4 to C5 and L3 to nal epidural hematoma (SCSEH) as a stroke L5. There was extreme tenderness when her mimic. This is especially pertinent when a right trapezius and upper paraspinal muscles patient’s symptoms are not fully consistent were palpated, but she had no midline cer- with an acute stroke, in order to avoid po- vical spine tenderness and had full, though tentially dangerous anticoagulation and al- painful, range of movement of her neck. Her low for prompt treatment of the hematoma. left side was unaffected. She had normal cra- nial nerves, no higher cortical dysfunction, a Case Glasgow Coma Scale (GCS) score of 15, and A 68-year-old woman presented to the ED via complete control of her bladder and bowel. -

Intracranial Hemorrhage
Intracranial Hemorrhage MARK MOSS, M.D. INTERVENTIONAL NEURORADIOLOGY WASHINGTON REGIONAL MEDICAL CENTER Definitions Stroke Clinical syndrome of rapid onset deficits of brain function lasting more than 24 hours or leading to death Transient Ischemic attack (TIA) Clinical syndrome of rapid onset deficits of brain function which resolves within 24 hours Epidemiology Stroke is the leading cause of adult disabilities 2nd leading cause of death worldwide 3rd leading cause of death in the U.S. 800,000 strokes per year resulting in 150,000 deaths Deaths are projected to increase exponentially in the next 30 years owing to the aging population The annual cost of stroke in the U.S. is estimated at $69 billion Stroke can be divided into hemorrhagic and ischemic origins 13% hemorrhagic 87% ischemic Intracranial Hemorrhage Collective term encompassing many different conditions characterized by the extravascular accumulation of blood within different intracranial spaces. OBJECTIVES: Define types of ICH Discuss best imaging modalities Subarachnoid hemorrhage / Aneurysms Roles of endovascular surgery Intracranial hemorrhage Outside the brain (Extra-axial) hemorrhage Subdural hematoma (SDH) Epidural hematoma (EDH) Subarachnoid hematoma (SAH) Intraventricular (IVH) Inside the brain (Intra-axial) hemorrhage Intraparenchymal hematoma (basal ganglia, lobar, pontine etc.) Your heads compartments Scalp Subgaleal Space Bone (calvarium) Dura Mater thick tough membrane Arachnoid flimsy transparent membrane Pia Mater tightly hugs the -
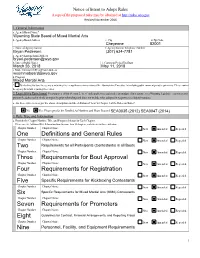
One Definitions and General Rules Two Three Requirements for Bout Approval Four Requirements for Registration Five Six Seven
Notice of Intent to Adopt Rules A copy of the proposed rules may be obtained at http://rules.wyo.gov Revised November 2016 1. General Information a. Agency/Board Name* b. Agency/Board Address c. City d. Zip Code e. Name of Agency Liaison f. Agency Liaison Telephone Number g. Agency Liaison Email Address h. Date of Public Notice i. Comment Period End Date j. Public Comment URL or Email Address: k. Program * By checking this box, the agency is indicating it is exempt from certain sections of the Administrative Procedure Act including public comment period requirements. Please contact the agency for details regarding these rules. 2. Legislative Enactment For purposes of this Section 2, “new” only applies to regular rules promulgated in response to a Wyoming legislative enactment not previously addressed in whole or in part by prior rulemaking and does not include rules adopted in response to a federal mandate. a. Are these rules new as per the above description and the definition of “new” in Chapter 1 of the Rules on Rules? No. Yes. Please provide the Enrolled Act Numbers and Years Enacted: 3. Rule Type and Information a. Provide the Chapter Number, Title, and Proposed Action for Each Chapter. Please use the Additional Rule Information form for more than 10 chapters, and attach it to this certification. Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed Chapter Number: Chapter Name: New Amended Repealed 1 4. -

Spontaneous Cervical Epidural Hematoma Mimicking Acute Ischemic Stroke
Published Ahead of Print on August 4, 2020 as 10.1212/WNL.0000000000010511 Rahangdale 1 Neurology Publish Ahead of Print DOI: 10.1212/WNL.0000000000010511 Spontaneous cervical epidural hematoma mimicking acute ischemic stroke Rahul Rahangdale, MD1, John Coburn, MD2, Christopher Streib, MD1 1 Department of Neurology, University of Minnesota, Minneapolis MN 2 Division of Neuroradiology, Midwest Radiology PA, St. Paul, MN Corresponding author: Rahul Rahangdale, Email: [email protected] Title character count: 70 Abstract word count: 0 Manuscript word count: 100 Legends word count: 50 References: 2 Figures: 2 Neurology® PublishedACCEPTED Ahead of Print articles have been peer reviewed and accepted for publication. This manuscript will be published in its final form after copyediting, page composition, and review of proofs. Errors that could affect the content may be corrected during these processes. Copyright © 2020 American Academy of Neurology. Unauthorized reproduction of this article is prohibited Rahangdale 2 Keywords: Spontaneous cervical spinal epidural hematoma, Stroke mimics, IV tPA Disclosure: R.Rahangdale. reports no disclosures relevant to the manuscript; J.Coburn. reports no disclosures relevant to the manuscript; C.Streib. reports no disclosures relevant to the manuscript. Study funding: No targeted funding reported. Manuscript: A 67-year-old male presented with acute right hemiparesis and hemianesthesia (NIHSS 5). Hyperacute neuroimaging was interpreted as normal. Following IV tPA, his symptoms worsened with concern for cervical radiculopathy. Upon reviewing the CT angiogram (CTA), a possible spinal epidural hematoma (EDH) was noted and subsequently confirmed with MRI (figure 1). Cryoprecipitate was administered. His symptoms gradually improved with conservative management. Spontaneous spinal EDH is rare (incidence: 0.1/100,000 per year).1 Risk factors include hypertension and 1 ACCEPTED2 coagulopathy. -

Spontaneous Cervical Epidural Hematoma: Case Report
Spinal Cord (1998) 36, 71 ± 72 1998 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/98 $12.00 Spontaneous cervical epidural hematoma: case report Adnan Awada1, Neville Russell2, Naif Al Fayez2, Richard Naufal3 and Hussein Al Kohlani2 Sections of 1Neurology and 2Neurosurgery and 3Department of Medical Imaging, King Fahd National Guard Hospital, POB 22490, Riyadh 11426, Saudi Arabia Spontaneous spinal epidural hematoma (SSEH) is an uncommon cause of acute nontraumatic myelopathy. We report a 14 year-old boy who had tetraplegia on awakening. Diagnosis of spinal epidural hematoma was made by magnetic resonance imaging. Despite spinal cord decompression within 9 h from onset, he remained tetraplegic. No cause for the bleeding was found. The pathogenic hypotheses of SSEH are discussed and the importance of rapid diagnosis and treatment is emphasized. Keywords: spinal cord; epidural hematoma; magnetic resonance imaging (MRI); acute myelopathy; tetraplegia Introduction Spinal epidural hematoma is a very rare cause of acute stimulation. Urinary retention and priapism were spinal cord compression. It is important to recognize it present. An acute cervical spinal cord disorder was since early diagnosis and prompt surgical evacuation suspected and an urgent magnetic resonance imaging provide the maximum chance of functional recovery. (MRI) examination ordered. This was performed at Spinal epidural hematoma has been reported in 3 pm and on T1 and T2-weighted images, revealed an association with blood dyscrasias, coagulopathies, iso-intense mass, centered at the level of C6 (a `double anti-coagulant treatment, infection, tumor, pregnancy cord' image) (Figure 1). This was compressing the and vascular malformations, but approximately half of dorsal aspect of the spinal cord. -

Pro Kickboxing Rules.Pdf
KICKBOXING RULES & REGULATIONS Professional Rules -Each match is three rounds in duration, with each round lasting three minutes. Title fights are five rounds in duration, with each round lasting three minutes. -The match can end by Knockout, Technical Knockout, Decision, Disqualification or No contest. A “No Contest” results from a fighter being unable to continue due to an inadvertent foul, etc. -The fighter, corner, referee, ring doctor and NHBWC all have full authority to stop the fight. -The fight is scored by three judges on a 10-Point Must Scoring System. -The three-knockdown rule is in effect. Three knockdowns in round results in a technical knockout. -The mandatory eight count is in effect (the referee must count to at least "eight" on all knockdowns). -The standing eight count is in effect (the referee has the right to declare a knockdown on a fighter who appears to be in a dangerous condition to continue in the match). -If a fighter intentionally spits out their mouthpiece, they’re given a warning. If it happens again, they’ll immediately receive a point deduction. If they do it again, they’re disqualified. -If a fighter turns their back to the opponent not in a striking motion, he will be given a standing eight count. If it happens again, they’re disqualified. -A fighter can be saved by the bell only in the last round. -Allowed to sweep a standing opponent (one or more leg on the ground). -Elbows and Knees to the head are allowed. -When catching a kick, the fighter is allowed to strike more than once as long as it does not exceed one step.