Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Icare Eye Hospital Rate List 2015
ICARE EYE HOSPITAL & POST GRADUATE INSTITUTE E-3A, Sector – 26, Noida – 201301 Tel:- 0120-2477600 / 02, Counselor: 0120-2477621 Fax: 0120-2556389 / Appointments: 9811880015 Email: [email protected] / Web: www.icarehospital.org ICARE EYE HOSPITAL RATE LIST 2015 S No. PARTICULAR TARIFF (₹) I CONSULTATION NEW PATIENT VALID FOR 7 DAYS (FIRST TIME CONSULTATION : REGISTRATION + 1 ₹ 600/- CONSULTATION) 2 REVIEW CONSULTATION VALID FOR 7 DAYS ₹ 500/- 3 EMERGENCY CONSULTATION FOR 7 DAYS ₹ 800/- 4 LOW VISUAL AIDS ASSESSMENT CHARGES ₹ 600/- 5 VISION THERAPY CHARGES FOR PER SITTING ₹ 200/- 6 COST OF VISION THERAPY SOFTWARE (CD) ₹ 6,000/- 7 AMBLYOPIA (CD) ₹ 4,000/- II INVESTIGATIONS 1 Digital F.F.A (Fundus Fluoroscein Angiography)(Inclusive of Fundus photo) ₹ 2,500/- 2 Colour Fundus Photo - Digital ₹ 600/- 3 Colour Slit-lamp photo ₹ 600/- 4 Duplicate color prints (FFA/OCT/CLINICAL PHOTO) ₹ 300/- 5 Orthoptic ₹ 250/- 6 OCT (Optical Coherence Tomography) ₹ 2,500/- A Repeat OCT (within 2 months) with printout ₹ 800/- B Anterior Segment OCT ₹ 2,500/- 7 Ultrasonography (U/S) A A Scan – Single Eye ₹ 600/- B B Scan – Single Eye ₹ 1,000/- C UBM - Single Eye ₹ 1,500/- 8 Computerized field analysis A Humphrey Visual Fields (HVF) both eyes ₹ 1,500/- B Humphrey Visual Fields (HVF) One eye ₹ 750/- 9 Diurnal Variation of Tension (Day DVT ) A 5 times tension (Done in both eyes)] ₹ 500/- Page 1 10 Pachymetry (Both eyes) A Ultrasound (Central Corneal Thickness- CST) ₹ 600/- B Optical ₹ 600/- 11 Corneal Topography A Single Eye ₹ 1,000/- B Both Eyes ₹ 2,000/- 12 -

Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232)
Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT NUMBER JURISDICTION STATE(S) First Coast Service Options, Inc. A and B MAC 09101 - MAC A J - N Florida First Coast Service Options, Inc. A and B MAC 09102 - MAC B J - N Florida First Coast Service Options, Inc. A and B MAC 09201 - MAC A J - N Puerto Rico Virgin Islands First Coast Service Options, Inc. A and B MAC 09202 - MAC B J - N Puerto Rico First Coast Service Options, Inc. A and B MAC 09302 - MAC B J - N Virgin Islands LCD Information Document Information LCD ID Original Effective Date L36232 For services performed on or after 11/22/2015 LCD Title Revision Effective Date Diagnostic Evaluation and Medical Management of For services performed on or after 01/08/2019 Moderate-Severe Dry Eye Disease (DED) Revision Ending Date Proposed LCD in Comment Period N/A N/A Retirement Date Source Proposed LCD N/A DL36232 Notice Period Start Date AMA CPT / ADA CDT / AHA NUBC Copyright 10/08/2015 Statement CPT codes, descriptions and other data only are Notice Period End Date copyright 2019 American Medical Association. All Rights 11/22/2015 Reserved. Applicable FARS/HHSARS apply. Current Dental Terminology © 2019 American Dental Association. All rights reserved. Copyright © 2019, the American Hospital Association, Created on 01/02/2020. Page 1 of 12 Chicago, Illinois. -

Cataract Surgery
Cataract surgery From Wikipedia, the free encyclopedia Jump to: navigation, search This article includes a list of references, related reading or external links, but its sources remain unclear because it lacks inline citations. Please improve this article by introducing more precise citations. (May 2011) Cataract surgery Intervention Cataract in Human Eye- Magnified view seen on examination with a slit lamp ICD-9-CM 13.19 MeSH D002387 Cataract surgery is the removal of the natural lens of the eye (also called "crystalline lens") that has developed an opacification, which is referred to as a cataract. Metabolic changes of the crystalline lens fibers over time lead to the development of the cataract and loss of transparency, causing impairment or loss of vision. Many patients' first symptoms are strong glare from lights and small light sources at night, along with reduced acuity at low light levels. During cataract surgery, a patient's cloudy natural lens is removed and replaced with a synthetic lens to restore the lens's transparency.[1] Following surgical removal of the natural lens, an artificial intraocular lens implant is inserted (eye surgeons say that the lens is "implanted"). Cataract surgery is generally performed by an ophthalmologist (eye surgeon) in an ambulatory (rather than inpatient) setting, in a surgical center or hospital, using local anesthesia (either topical, peribulbar, or retrobulbar), usually causing little or no discomfort to the patient. Well over 90% of operations are successful in restoring useful vision, with a low complication rate.[2] Day care, high volume, minimally invasive, small incision phacoemulsification with quick post-op recovery has become the standard of care in cataract surgery all over the world. -

Fixing Patients' Problems
CAN TABLETS WORK FOR EMR? P. 12 • CODING TIPS FOR CROSS-LINKING P. 16 A FRESH ANGLE ON RESIDENT TRAINING P. 68 • SIXTH CRANIAL NERVE DYSFUNCTION IN KIDS P. 72 Review of Ophthalmology Vol. XXIV, No. 4 • April 2017 • Fighting for Patient Care • Avoiding Problems Using OCT • Managing Refractive Surprises Problems • Optical Biometry Roundup Care • Avoiding No. 4 • April 2017 • Fighting for Patient Review of Ophthalmology Vol. XXIV, STEM THE TIDE OF EXCESSIVE TEARING P. 76 • POST-INJECTION IOP SPIKES P. 96 April 2017 reviewofophthalmology.com Fixing Patients’ Problems Expert surgeons give you the tools you need to succeed. ALSO INSIDE: Sizing Up Optical Biometers P. 58 001_rp0417_fc-WB.indd 1 3/24/17 12:52 PM VISIT US AT ASCRS BOOTH #1022 It’s all in CHOOSE A SYSTEM THAT EMPOWERS YOUR EVERY MOVE. Technique is more than just the motions. Purposefully engineered for exceptional versatility and high-quality performance, the WHITESTAR SIGNATURE® PRO Phacoemulsification System gives you the clinical flexibility, confidence and control to free your focus for what matters most in each procedure. How do you phaco? Join the conversation at WWW.ABBOTTPHACO.COM Rx Only INDICATIONS: The WHITESTAR SIGNATURE® PRO System is a modular ophthalmic microsurgical system that facilitates anterior segment (cataract) surgery. The modular design allows the users to configure the system to meet their surgical requirements. IMPORTANT SAFETY INFORMATION: Risks and complications of cataract surgery may include broken ocular capsule or corneal burn. This device is only to be used by a trained, licensed physician. ATTENTION: Reference the labeling for a complete listing of Indications and Important Safety Information. -

Primary External Dacryocystorhinostomy
11 Primary External Dacryocystorhinostomy Richard H. Hart, Suzanne Powrie, and Geoffrey E. Rose The watering eye may be the result of excessive tear production, abnor- malities of lid position or movement, lacrimal canalicular pump failure, or obstruction of the outfl ow tract. With external dacryocystorhinos- tomy (DCR), the lacrimal sac is directly incorporated into the lateral wall of the nose, so that the canaliculi drain directly into the nasal cavity. The aims of surgery are twofold: to eliminate fl uid and mucus reten- tion within the lacrimal sac and prevent sac enlargement (as a muco- cele) – the latter leading to intermittent viscous ocular discharge – and to bypass the higher hydraulic resistance of the nasolacrimal duct, thereby increasing tear conductance and aiding the relief of epiphora. Indications for Surgery 1. Primary acquired nasolacrimal duct obstruction 2. Secondary acquired nasolacrimal duct obstruction attributed, for example, to dacryolithiasis, endonasal surgery, infl ammatory nasal or sinus disease, or prior midfacial injury 3. Persistent congenital nasolacrimal duct obstruction, often after unsuccessful probing or intubation of the nasolacrimal duct 4. Functional obstruction of lacrimal outfl ow with decreased tear conductance as a result of: (a) Stenosis, but not occlusion, of the nasolacrimal duct (b) Lacrimal canalicular pump failure from age-related laxity of the lower eyelid, or after facial nerve palsy 5. Acute or chronic dacryocystitis; the former group requiring initial treatment with systemic antibiotics Surgical Principles External DCR should establish a low-resistance drainage pathway between the conjunctival tear sac and the nasal cavity, by conversion of the lacrimal sac into part of the lateral nasal wall. -

Original Research Paper Anna Heinke Medicine
VOLUME-9, ISSUE-4, APRIL -2020 • PRINT ISSN No. 2277 - 8160 • DOI : 10.36106/gjra Original Research Paper Medicine THE EFFICACY OF TREATMENT WITH AFLIBERCEPT INTRAVITREAL INJECTIONS IN PATIENTS WITH WET AGE-RELATED MACULAR DEGENERATION". Department of Ophthalmology, School of Medicine in Katowice, Medical Anna Heinke University of Silesia, Katowice, Poland Katarzyna University Clinical Center, University Hospital Medical University of Silesia, Michalska- Katowice, Poland *Corresponding Author Małecka* ABSTRACT Purpose: The aim of this study was to evaluate the effectiveness and safety of treatment with aibercept administered intravitreally in patients with neovascular age-related macular degeneration after rst year of treatment. Moreover, the inuence of following factors on therapeutic success with aibercept was investigated: CNV type, lens status (pseudophakic vs phakic), patient's age, sex and the fact if patient was previously receiving anty-VEGF injections. Methods: A prospective clinical study was conducted on 90 eyes of patients (age 56 to 89 years old, 50 females, 40 males) who were diagnosed with choroidal neovascularisation (CNV) due to wet AMD. Before each injection best corrected visual acuity(BCVA) on Snellen chart, converted then to ETDRS scale for statistical purposes and central retinal thickness (CRT) using optical coherence tomography (OCT) were assessed. All patients received 3 doses of 2,0 mg intravitreal aibercept every 4 weeks, followed by aibercept injections every 2 months. The primary endpoint of the study was determined on best corrected visual acuity (BCVA) and changes observed in central retinal thickness (CRT) 3 months and 1 year after treatment with aibercept comparing with BCVA and OCT at the baseline. Results: After the rst year of treatment with aibercept a statistically signicant improvement of mean BCVA was observed. -

Topical Clear Aqueous Nanomicellar Formulations for Age
TOPICAL CLEAR AQUEOUS NANOMICELLAR FORMULATIONS FOR AGE-RELATED MACULAR DEGENERATION A DISSERTATION IN Pharmaceutical Sciences and Chemistry Presented to the Faculty of University of Missouri-Kansas City in partial fulfillment of requirements for the degree DOCTOR OF PHILOSOPHY by Meshal Alshamrani Pharm. D. King Abdul-Aziz University, Saudi Arabia, 2013 Kansas City, Missouri 2020 © 2020 MESHAL ALSHAMRANI ALL RIGHTS RESERVED TOPICAL CLEAR AQUEOUS NANOMICELLAR FORMULATIONS FOR AGE-RELATED MACULAR DEGENERATION Meshal Alshamrani, Candidate for the Doctor of Philosophy Degree University of Missouri-Kansas City, 2020 ABSTRACT Disorders affecting the posterior segment of eyes represent a significant burden to healthcare and patients’ wellbeing. Among the back of the eye disorders, age-related macular degeneration (AMD) is one of the major ailments responsible for blindness worldwide. There is currently no effective treatment available to cure AMD completely. Anti-VEGF therapy is currently considered the treatment of choice. However, it is invasive and does not offer substantial long-term relief to AMD patients. Other treatment options include thermal laser photocoagulation and surgery. None of these therapeutic approaches are safe and effective. Hence there is a real need for the development of an alternative therapeutic approach that is safe, effective and non-invasive. The objective of this study is to develop a clear, aqueous drug-loaded nanomicellar formulation utilizing FDA approved polymers, namely Hydrogenated castor oil 40 (HCO-40) and Octoxynol 40(OC-40) as a potential-therapeutics for AMD. Hydrophobic drugs such as curcumin (CUR), celecoxib (CXB), and resveratrol (RSV) were successfully solubilized and entrapped in the core of the nanomicelles. These nanomicellar constructs efficiently utilize their hydrophilic corona and evade the wash-out into the systemic circulation from both the conjunctival and choroidal blood vessels and lymphatics, thus overcoming the dynamic barrier. -

Oral Furosemide Therapy in Patients with Exudative Retinal Detachment
Case Report iMedPub Journals Annals of Clinical and Laboratory Research 2018 www.imedpub.com ISSN 2386-5180 Vol.6 No.3:240 DOI: 10.21767/2386-5180.100240 Oral Furosemide Therapy in Patients with Ichsan AM1,2*, Stevanie N1, Exudative Retinal Detachment Due to Habibah SM1,2 and Budu P1,2 Hypertensive Retinopathy-IV 1 Faculty of Medicine, Department of Ophthalmology, Hasanuddin University, Makassar, Indonesia 2 Celebes Eye Center ORBITA, Makassar, Indonesia Abstract Introduction: Hypertensive retinopathy is a condition characterized by a spectrum of retinal vascular signs in people with elevated blood pressure. This condition can be accompanied by exudative retinal detachment in hypertensive retinopathy *Corresponding author: grade IV. Furosemide is considered as a diuretic agent to force fluid absorption Ichsan AM across the retinal epithelium. This is consistent with a model for ion transport in the isolated RPE, in which active furosemide-inhibitable transport of chloride from [email protected] retina to choroid for a significant fraction of the short-circuit current. Objectives: To report the efficacy of oral furosemide in patients with exudative Faculty of Medicine, Department of retinal detachment due to hypertensive retinopathy-IV. Ophthalmology, Hasanuddin University, Case presentation: We reported two young patients, first patient with chronic Makassar, Indonesia. kidney disease complained with decreased of visual acuity to 20/100 in the right and 20/200 in the left eye. The second patient with preeclampsia suddenly Tel: +6281342280880 experienced bilateral visual loss to counting finger on both eyes. Those patients 1b showed sub-retinal fluid, macular star and cotton wool spots in both retina. Macular edema was seen by optical coherence tomography (OCT) examination in Citation: Ichsan AM, Stevanie N, Habibah both eyes. -
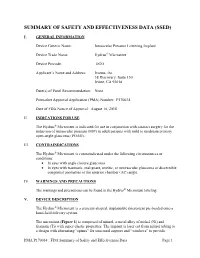
Summary of Safety and Effectivness (SSED)
SUMMARY OF SAFETY AND EFFECTIVENESS DATA (SSED) I. GENERAL INFORMATION Device Generic Name: Intraocular Pressure Lowering Implant Device Trade Name: Hydrus® Microstent Device Procode: OGO Applicant’s Name and Address: Ivantis, Inc. 38 Discovery, Suite 150 Irvine, CA 92618 Date(s) of Panel Recommendation: None Premarket Approval Application (PMA) Number: P170034 Date of FDA Notice of Approval: August 10, 2018 II. INDICATIONS FOR USE The Hydrus® Microstent is indicated for use in conjunction with cataract surgery for the reduction of intraocular pressure (IOP) in adult patients with mild to moderate primary open-angle glaucoma (POAG). III. CONTRAINDICATIONS The Hydrus® Microstent is contraindicated under the following circumstances or conditions: • In eyes with angle closure glaucoma • In eyes with traumatic, malignant, uveitic, or neovascular glaucoma or discernible congenital anomalies of the anterior chamber (AC) angle. IV. WARNINGS AND PRECAUTIONS The warnings and precautions can be found in the Hydrus® Microstent labeling. V. DEVICE DESCRIPTION The Hydrus® Microstent is a crescent-shaped, implantable microstent pre-loaded onto a hand-held delivery system. The microstent (Figure 1) is composed of nitinol, a metal alloy of nickel (Ni) and titanium (Ti) with super-elastic properties. The implant is laser cut from nitinol tubing to a design with alternating “spines” for structural support and “windows” to provide PMA P170034: FDA Summary of Safety and Effectiveness Data Page 1 outflow pathways for aqueous humor. After laser cutting, the shape of the implant is heat-set to a curvature intended to match the curvature of Schlemm’s canal and is electro- polished to create a smooth surface. The microstent is approximately 8 mm in overall length with major and minor axes of 292 µm and 185 µm, respectively. -

( 12 ) United States Patent
US010220021B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 ,220 ,021 B2 Solis Herrera ( 45 ) Date of Patent : Mar. 5 , 2019 (54 ) METHODS FOR TREATING AND 2005 /0148516 AL 7 /2005 Taniguchi et al. PREVENTING OCULAR DISEASES , 2010 /0010082 AL 1 /2010 Chong et al . DISORDERS , AND CONDITIONS WITH 2012 /0270907 Al 10 / 2012 Herrera MELANIN AND MELANIN ANALOGS, 2013 /0109745 Al 5 / 2013 Ji et al . PRECURSORS, AND DERIVATIVES FOREIGN PATENT DOCUMENTS (71 ) Applicant: Arturo Solis Herrera , Aguascalientes EP 1460134 A1 9 / 2004 MX( ) EP 2594268 A1 5 / 2013 JP 2009517396 A 4 / 2009 JP 2013531032 A 8 / 2013 (72 ) Inventor: Arturo Solis Herrera , Aguascalientes KR 20120008429 A 1 / 2012 (MX ) WO 1992007580 A1 5 / 1992 WO 20030060131 A1 7 / 2003 ( * ) Notice : Subject to any disclaimer, the term of this WO 20070064752 A2 6 / 2007 patent is extended or adjusted under 35 WO 2007102724 A2 9 / 2007 U . S . C . 154 (b ) by 0 days. WO 2012008674 A1 1 / 2012 ( 21 ) Appl. No. : 15 /509 , 532 OTHER PUBLICATIONS Sep . 8 , 2015 Int ' l Preliminary Report on Patentability dated Mar. 14 , 2017 in Int' l (22 ) PCT Filed : Application No. PCT/ IB2015 /001570 . Int' l Search Report dated Feb . 12 , 2016 in Int' l Application No . ( 86 ) PCT No .: PCT/ IB2015 / 001570 PCT/ IB2015 /001570 . $ 371 (c )( 1 ), Lai et al, “ Effect of Melanin on Traumatic Hyphema in Rabbits , " Arch . Ophthalmol ., vol. 177 , No. 6 , pp . 789 -793 ( 1999 ) . ( 2 ) Date : Mar. 8 , 2017 Office Action dated Aug . 7 , 2017 in CA Application No . 2960583. Office Action dated Aug. -

Operative Dictations in Ophthalmology Eric D
Operative Dictations in Ophthalmology Eric D. Rosenberg • Alanna S. Nattis Richard J. Nattis Editors Operative Dictations in Ophthalmology Editors Eric D. Rosenberg Alanna S. Nattis Ophthalmology Resident Cornea and Refractive Surgery Fellow Department of Ophthalmology Ophthalmic Consultants of Long Island New York Medical College Rockville Centre, NY, USA Valhalla, NY, USA Richard J. Nattis Chief of Ophthalmology and Clinical Professor Department of Ophthalmology Good Samaritan Hospital West Islip, NY, USA ISBN 978-3-319-45494-8 ISBN 978-3-319-45495-5 (eBook) DOI 10.1007/978-3-319-45495-5 Library of Congress Control Number: 2017932292 © Springer International Publishing Switzerland 2017 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. -

Curriculum Vitae
Kashkouli MB, CV CURRICULUM VITAE Mohsen Bahmani Kashkouli, MD Section Subject I Personal Information II 1. Executive Position 2. Journal Editor 3. Organizing a meeting 4. Journals’ reviewer, 5. Establishing an organization III Education IV Work Experience V Trained Fellows VI Edited Books/ Chapters VII Peer Reviewed Paper Publications VIII Courses Attended IX Directing Workshops/Courses/ Symposia X Conference Abstracts XI Invited (Guest) Speaker XII Awards XIII Innovations XIV Ongoing Research Projects XV Referees XVI Interests XVII Affiliations 1 Kashkouli MB, CV I. PERSONAL INFORMATION NAME: Mohsen Bahmani Kashkouli WORK ADDRESS University Hospital Private Office Rassoul Akram Hospital No.:49, West Brazil- South Sattarkhan-Niayesh Avenue Sheikhbahaee intersection, POBox: 14455-364 Tehran, Iran Tehran, Iran Phone: +98 21 66559595 Phone: +98 21 88065620 Fax: +98 21 66509162 Fax: +98 21 66558811 Email [email protected] DATE OF BIRTH: 09/January/1967 PLACE OF BIRTH: Gachsaran , Iran Language: Farsi, English, Turkish II. SCIENTIFIC & EXECUTIVE POSITIONS 1. Executive Positions 2. Professor, Head of Oculo-Facial Plastic Surgery, Rassoul Akram Hospital, Iran University of Medical Sciences (www.iums.ac.ir), Tehran, Iran. 3. Regional (Iran and Turkey) Vice President of Middle East African Council of Ophthalmology (MEACO).(www.meaco.org), Since Nov. 2019. 4. Vice President of Middle East African Council of Ophthalmology (MEACO) in Middle East (www.meaco.org), Since 2012. 5. Vice President, Middle East African Society of Ophthalmic Plastic and Reconstructive Surgery (MEASOPRS, www.meaco.org ), Since June 2016. 6. Scientific Coordinator, Middle East African Society of Ophthalmic Plastic and Reconstructive Surgery (MEASOPRS, www.meaco.org ), 2012-2016. 7. Scientific Director and chair of International relation section, Iranian Society of Ophthalmic Plastic and Reconstructive Suregry (IrSOPRS, www.irso.org/irsoprs), Tehran, Iran, Since 2007.