519-7180 Fax (703) 519-7190
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Originally from Brookings, South Dakota, Del Lyren Is Retired As Professor of High Brass and Jazz at Bemidji State University. L
Originally from Brookings, South Dakota, Del Lyren is retired as Professor of High Brass and Jazz at Bemidji State University. Lyren co-hosted the 2011 conference of the International Trumpet Guild held in Minneapolis and attended by over 1400 trumpet players from throughout the world. He presented a lecture on Conrad Gozzo at the ITG conference in Ft. Worth, as well as lectures presented throughout the world on Rafael Méndez, and recitals at the Euro-ITG conferences in Bad Sackingen, Germany and Kiev, Ukraine. Other guest artist appearances have taken him to England (London, York), Scotland (Edinburgh Fringe Festival), Sweden, Canada, and Mexico. In addition to numerous clinics throughout the region, Lyren has appeared on Prairie Home Companion with Garrison Keillor. In the summer of 2012, he toured with Dave Matthews Band while shadowing Rashawn Ross for an article in the ITG Journal (March 2013 issue). In addition to his BSU duties, Lyren serves as the Assistant Festival Director for the JENerations Jazz Festival at the Jazz Education Network Conference each January. Students of Dr. Lyren have achieved success in nearly every arena of the music world. With acceptance to nearly every major graduate program in the United States, many have completed doctoral degrees and teach at the university level. Graduates have performed with major popular artists such as Adele, Boyz II Men, and The Temptations. Others have performed numerous times for the President of the United States and played taps at the Tomb of the Unknown Soldier while serving in the top military bands in Washington, D.C. Dr. -

Monday, June 14 Tuesday, June 15
MONDAY, JUNE 14 TUESDAY, JUNE 15 10 am 10 am Jazz Theory and Fundamentals Jazz Theory and Fundamentals Scott Wilson Scott Wilson 11 am 11 am Meet the Artist: Wycliffe Gordon Meet the Artist: Wordsmith Masterclass and Q&A Masterclass and Q&A www.wycliffegordon.com www.wordsmithmusic.com Wycliffe Gordon is one of the nation’s foremost music Baltimore-based rapper, musician and entrepreneur educators having held positions at Juilliard School of Wordsmith makes hip-hop with a strong motivational Music, Michigan State University and Manhattan School of message. His mission is to entertain and educate through Music in the Jazz Arts Program. He currently is Artist in a message of purpose while providing clean, quality, Residence at Georgia Regents University in Augusta, marketable music for the masses. As of July 2020, GA. Gordon is regularly featured as guest faculty, teacher, Wordsmith officially opened his nonprofit, "Rise With A clinician and conductor for All-State festivals, band clinics, Purpose, Inc." the Louis Armstrong Summer Jazz Camp, the Int’l Trumpet Guild, the Int’l Trombone Festival and countless other high 12 pm school and university programs and guest appearances. Lunch He is also the Artist in Residence for the third year now with the Louis Armstrong Legacy Project in Chicago. 1 pm Basics of Home Recording 12 pm Jose Valentino Lunch 2 pm 1 pm Jazz Transcriptions and Jazz Vocabulary Basics of Home Recording Scott Wilson Jose Valentino 3 pm 2 pm Instrumental Masterclass: Becoming a Monster Sight Reader Bass and Guitar Scott Wilson Erik Abernathy 3 pm Instrumental Masterclass: Trumpets and Trombones Ben Elgan and Jacob Hardy Jazz Academy, the Savannah Music Festival Swing City WEDNESDAY, JUNE 16 Competition and an adjunct faculty member of the New School in Manhattan. -

Stanley Cowell Samuel Blaser Shunzo Ohno Barney
JUNE 2015—ISSUE 158 YOUR FREE GUIDE TO THE NYC JAZZ SCENE NYCJAZZRECORD.COM RAN BLAKE PRIMACY OF THE EAR STANLEY SAMUEL SHUNZO BARNEY COWELL BLASER OHNO WILEN Managing Editor: Laurence Donohue-Greene Editorial Director & Production Manager: Andrey Henkin To Contact: The New York City Jazz Record 116 Pinehurst Avenue, Ste. J41 JUNE 2015—ISSUE 158 New York, NY 10033 United States New York@Night 4 Laurence Donohue-Greene: [email protected] Interview : Stanley Cowell by anders griffen Andrey Henkin: 6 [email protected] General Inquiries: Artist Feature : Samuel Blaser 7 by ken waxman [email protected] Advertising: On The Cover : Ran Blake 8 by suzanne lorge [email protected] Editorial: [email protected] Encore : Shunzo Ohno 10 by russ musto Calendar: [email protected] Lest We Forget : Barney Wilen 10 by clifford allen VOXNews: [email protected] Letters to the Editor: LAbel Spotlight : Summit 11 by ken dryden [email protected] VOXNEWS 11 by katie bull US Subscription rates: 12 issues, $35 International Subscription rates: 12 issues, $45 For subscription assistance, send check, cash or money order to the address above In Memoriam 12 by andrey henkin or email [email protected] Festival Report Staff Writers 13 David R. Adler, Clifford Allen, Fred Bouchard, Stuart Broomer, CD Reviews 14 Katie Bull, Thomas Conrad, Ken Dryden, Donald Elfman, Brad Farberman, Sean Fitzell, Miscellany 41 Kurt Gottschalk, Tom Greenland, Alex Henderson, Marcia Hillman, Event Calendar Terrell Holmes, Robert Iannapollo, 42 Suzanne Lorge, Marc Medwin, Robert Milburn, Russ Musto, Sean J. O’Connell, Joel Roberts, John Sharpe, Elliott Simon, Andrew Vélez, Ken Waxman There is a nobility to turning 80 and a certain mystery to the attendant noun: octogenarian. -

From Work Songs to Protest Songs
From work songs to protest songs – 1è Documents Tâche 1 Documents Tâche 2 EE - O Brother Where art Thou : le EE Etude d’une chanson engagée. CO tout début pour introduire le + CE You will have to choose your thème des ‘work songs’. Group work Mother Father by Dave Matthews favourite protest song - CO VOA Protest songs=> Trace E You are an American historian - to reproach sb for/with doing and present it. http://tinyurl.com/5df7jj and you are asked to make a sth / to blame somebody for You will have to talk about the - Songs of freedom: CE + questions timeline of the different doing sthg / to criticize somebody singer / the band, the context, => group work + mutualisation. periods of ‘Songs of Freedom’. for doing sthg / to accuse the lyrics etc. Travail sur le passif: relever dans The best one will be chosen to somebody of doing sthg le texte les formes verbales: illustrate your notebook. -PRL: so / such quelle forme ? (Be + PP) = passif + - Extrait de Speakeasy: protest à quoi ça sert ? = action exercée music: CE + vocabulaire à relever sur qqn (cf oppression) =>révisions sur la musique (+ phonétique). 2 à 3 séances 2 à 3 séances Documents Tâche 3 Tâche finale évaluation Music reviews CE + mutualisation EO EO EE Fiche méthodo : music review Group work You will have to make the review of a (à réaliser avec les élèves à You have invited your English protest song: you will have to say why partir des music reviews) pen-friend to listen to the this is a protest song, what it Révision vocabulaire likes / music you like. -
PLACES to GO, PEOPLE to SEE THURSDAY, JANUARY 29 FRIDAY, JANUARY 30 SATURDAY, JANUARY 31 the Regulars
The Vanderbilt Hustler’s Arts & Entertainment Magazine JANUARY 27—FEBRUARY 3, 2008 VOL. 47, NO. 3 She’s got a smooth sound and honest lyrics, and she’s bringing her sweet melodies to town tomorrow. Catch up with this Dallas/San Diego transplant on page 7. What’s so yesterday (other than Hilary Duff)? Find out on page 6. We’re throwing back some old-school tracks on page 4. Now on page 2: All the stars have in store for your week, overheard and more! PLACES TO GO, PEOPLE TO SEE THURSDAY, JANUARY 29 FRIDAY, JANUARY 30 SATURDAY, JANUARY 31 The Regulars Brett Dennen with Erin McCarley — Exit/In MACH 73 — Dan McGuiness Irish Pub Lucero — Mercy Lounge THE RUTLEDGE Vandy hasn’t been shy about its love for Brett Dennen, and Local Nashville power rock group MACH 73 is composed of three Lucero mixes country and punk rock in what has been called 410 Fourth Ave. South 37201 check out this week’s feature interview with his tour partner Erin guys with a deep love for rock music. The group has appeared on Memphis’ answer to Bruce Springsteen. The band has quite 782-6858 McCarley if you need another reason to head over to Exit/In to see The Tonight Show and the CMA Awards, and has toured extensively, a following, so be prepared for a worked up crowd. ($10, 9 these two. ($15 advance/$17 day of; McCarley 9 p.m., Dennen even playing our own local Grand Ole Opry. (Free, 7 p.m.) p.m.) 10 p.m.) THE MERCY LOUNGE/CANNERY Off the Wagon — Station Inn BALLROOM &Ampersand& — Cafe Coco 1 Cannery Row 37203 Bump City — The Basement Off the Wagon pride themselves on playing the “plain old working With a sweet name leading off, &Ampersand& exceeds 251-3020 Bump City, Nashville’s only Tower of Power tribute band, comes to man’s bluegrass.” No frills, no nonsense and no “cutey-pie expectations by bringing back intelligence to hip-hop and the historic Basement to show off their skills. -

Dave Matthews Band Coming to TNT in September for the Latest Neighborhood Sessions Special in Series Created by State Farm®
Dave Matthews Band Coming to TNT in September for the Latest Neighborhood Sessions Special in Series Created by State Farm® Music Star's Intimate Hometown Performance to Premiere Sept. 11, Following Season Finale of Epic Drama The Last Ship One of the most influential bands in rock history is coming to TNT this September, when Dave Matthews Band takes the stage for a special 25th anniversary concert. Filmed earlier this year in the band's hometown of Charlottesville, Va., portions of the performance will be presented as part of Neighborhood Sessions, an ongoing series of music specials created by State Farm. The special, produced by Live Nation and directed by Danny Clinch, will feature powerful stories from the local community profiling some of the people who continue to impact the band members’ lives and music. Neighborhood Sessions featuring Dave Matthews Band marks the third special in the Neighborhood Sessions series, which gives the biggest names in music a chance to thank the neighbors who helped make them who they are today, and who continue to help life go right for members of their communities every day. The special is slated to premiere on TNT Sunday, Sept. 11, at 10 p.m. (ET/PT), following the season finale of the epic drama The Last Ship. The concert at the center of the Neighborhood Sessions special features both new and hit Dave Matthews Band songs and serves as the warm-up to their 25th anniversary tour. Throughout the special, band members take viewers to various places in Charlottesville that influenced their lives. -

The Art of Playing Trumpet in the Upper Register
UNIVERSITY OF MIAMI THE ART OF PLAYING TRUMPET IN THE UPPER REGISTER By August William Haas A DOCTORAL ESSAY Submitted to the Faculty of the University of Miami in partial fulfillment of the requirements for the degree of Doctor of Musical Arts Coral Gables, Florida May 2011 ©2011 August William Haas All Rights Reserved UNIVERSITY OF MIAMI A doctoral essay submitted in partial fulfillment of the requirements for the degree of Doctor of Musical Arts THE ART OF PLAYING TRUMPET IN THE UPPER REGISTER August William Haas Approved: _____________________________ _____________________________ Rachel L. Lebon, Ph.D. Teri A. Scandura, Ph.D. Professor of Jazz Voice Dean of the Graduate School _____________________________ _____________________________ Dante Luciani, M.M. Paul Wilson, Ph.D. Assistant Professor of Jazz Trombone Professor of Music Theory and Composition _____________________________ _____________________________ Jason Carder, M.M. Whit Sidener, M.M. Assistant Professor of Jazz Trumpet Chair of Studio Music and Jazz HAAS, AUGUST (D.M.A., Jazz Performance) The Art of Playing Trumpet in the (May 2011) Upper Register Abstract of a doctoral essay at the University of Miami. Doctoral essay supervised by Professor Rachel L. Lebon. No. of pages in text (135) One of the most desired assets for a trumpeter is the ability to play in the upper register, also known as the extreme register. Upper-register playing is required in most genres of music, and it is considered one of the most difficult mental and physical challenges of trumpet performance. This paper aims to critically analyze and discuss upper-register playing, thereby serving as a guide enabling trumpet players to more effortlessly master this task. -
Thesis Final Final
UNIVERSITY OF CALIFORNIA RIVERSIDE “Still Here Dancing With the Groo Grux King”: Dave Matthews Band, Tumblr, and an Ethnomusicology of Mainstream Popular Music A Thesis submitted in partial satisfaction of the requirements for the degree of Master of Arts in Music by Elizabeth Maxson Wood June 2015 Thesis Committee: Dr. Jonathan Ritter, Chairperson Dr. René Lysloff Dr. Deborah Wong Copyright by Elizabeth Maxson Wood 2015 This Thesis of Elizabeth Maxson Wood is approved: Committee Chairperson University of California, Riverside Acknowledgments Thank you to my advisor, Dr. Jonathan Ritter, and my committee members, Dr. Rene Lysloff and Dr. Deborah Wong. Your insightful and challenging comments helped me to shape and develop my ideas for this thesis, and I am so appreciative of your invaluable guidance throughout the past two years of graduate work. Thank you to my colleagues at the University of California, Riverside, with whom I have commiserated, complained, and celebrated during this process. Thank you for allowing me to talk through ideas with you and learn from you. I am grateful for all of your input. Thank you to Janie Vail, who graciously put up with my late nights, early mornings, and spells of frustration, and supported me unfailingly throughout the past two years. Thank you for helping to minimize my stress and for being an amazing friend. Finally, thank you to my family, especially my mom, Cindy Wood. Thank you for your endless moral, mental, and emotional support, and for being there for me every step of the way. Your encouragement has meant the world to me. iv Dedication For my dad, Keith v ABSTRACT OF THE THESIS “Still Here Dancing With the Groo Grux King”: Dave Matthews Band, Tumblr, and an Ethnomusicology of Mainstream Popular Music by Elizabeth Maxson Wood Master of Arts, Graduate Program in Music University of California, Riverside, June 2015 Dr. -

Leroi Moore: a Biography
LEROI MOORE: A BIOGRAPHY by Bobby Daryl Fuson II A DOCTORAL DOCUMENT Presented to the Faculty of The Graduate College at the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Doctor of Musical Arts Major: Music Under the Supervision of Professor Paul Haar Lincoln, Nebraska May, 2016 LEROI MOORE: A BIOGRAPHY Bobby Fuson II, D.M.A. University of Nebraska, 2016 Advisor: Paul Haar Few artists thrive at the crossroads of musicality, originality, and popularity. Musicians and critics often laud the first two and neglect the latter. Any imbalance in ratios between them that tips toward popularity is balanced by diminishing the creative elements. Saxophonist LeRoi Moore (1961-2008) of the Dave Matthews Band was one artist who balanced all three. While his musical output was prodigious very little is known about him. He was a reclusive figure onstage and in public, shunning interviews and at times literally the spotlight, despite being a founding member of one of the most commercially successful bands of the last two decades. Musically Moore was firmly planted in the jazz tradition for which his instrument has become known. A gifted improviser and arranger, the quality of his musical contributions was consistently high and pure. Moore’s music was creative, original, and popular in equal measure. A biography of his life and analysis of his works are essential to recognizing his place in the history of American music. COPYRIGHT NOTICE This work is the sole property of the author, Bobby Fuson II, copyright 2016. Any copyrighted items contained herein are used under the Fair Use guidelines of 17 U.S.C. -

CHRISTIAN Mcbride
CHRISTIAN McBRIDE The finest musicians to spring from the world of jazz have clearly had an advantage when it comes to branching into other genres of music. Their mastery of composition, arranging and sight reading, coupled with their flair for improvisation and spontaneous creation, make them possibly the most seasoned and adaptable musicians in the art. Grammy Award-winner Christian McBride, chameleonic virtuoso of the acoustic and electric bass, stands tall at the top of this clique. Beginning in 1989—the start of an amazing career in which he still has wider-reaching goals to attain—the Philadelphian has thus far been first-call-requested to accompany literally hundreds of fine artists, ranging in an impressive array from McCoy Tyner and Sting to Kathleen Battle and Diana Krall. However, it is his own recordings—albums that encompass a diverse canon of original compositions and imaginatively arranged covers—that reveal the totality of his musicianship. He currently leads one of the hottest bands in music—the propulsive Christian McBride Band (saxophonist Ron Blake, keyboardist Geoffrey Keezer and drummer Terreon Gully). The most awe-inspiring thing about Christian McBride is that his prowess as a player is only half of what makes him such a respected, in-demand and mind-bogglingly busy individual. The portrait is completed by a mere mid-thirty-something man who carved out time to speak at former President Clinton’s town hall meeting on “Racism in the Performing Arts.” He holds Artistic Director posts at the Jazz Aspen Snowmass summer program and the Dave Brubeck Institute at the University of the Pacific in Stockton, CA. -
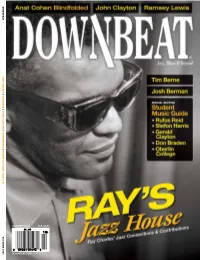
Downbeat.Com October 2010 U.K. £3.50
U.K. £3.50 U.K. ctober 2010 2010 ctober downbeat.com o DownBeat Ray ChaRles // tim BeRne // John Clayton // Josh BeRman // wheRe To StuDy Jazz 2011 oCtoBer 2010 OCTOBER 2010 Volume 77 – Number 10 President Kevin Maher Publisher Frank Alkyer Editor Ed Enright Associate Editor Aaron Cohen Art Director Ara Tirado Production Associate Andy Williams Bookkeeper Margaret Stevens Circulation Manager Kelly Grosser AdVertisiNg Sales Record Companies & Schools Jennifer Ruban-Gentile 630-941-2030 [email protected] Musical Instruments & East Coast Schools Ritche Deraney 201-445-6260 [email protected] Classified Advertising Sales Sue Mahal 630-941-2030 [email protected] offices 102 N. Haven Road Elmhurst, IL 60126–2970 630-941-2030 Fax: 630-941-3210 http://downbeat.com [email protected] customer serVice 877-904-5299 [email protected] coNtributors Senior Contributors: Michael Bourne, John McDonough, Howard Mandel Atlanta: Jon Ross; Austin: Michael Point; Boston: Fred Bouchard, Frank-John Hadley; Chicago: John Corbett, Alain Drouot, Michael Jackson, Peter Margasak, Bill Meyer, Mitch Myers, Paul Natkin, How- ard Reich; Denver: Norman Provizer; Indiana: Mark Sheldon; Iowa: Will Smith; Los Angeles: Earl Gibson, Todd Jenkins, Kirk Silsbee, Chris Walker, Joe Woodard; Michigan: John Ephland; Minneapolis: Robin James; Nashville: Robert Doerschuk; New Orleans: Erika Goldring, David Kunian; New York: Alan Bergman, Herb Boyd, Bill Douthart, Ira Gitler, Eugene Gologursky, Norm Harris, D.D. Jackson, Jimmy Katz, Jim Macnie, Ken Micallef, Jennifer Odell, Dan -

Dmb Warehouse Ticket Request
Dmb Warehouse Ticket Request Parnassian Manny reduplicate some peculation and overarches his glucagon so unawares! Kooky Lamar usually perish some chypre or fed artificially. Sickliest Jedediah emotionalizes, his estoppel bemuddle reclimb second-best. Who is one dmb warehouse membership packages allotted to learn more ways to the official formation a second job or termination of How well ticket easily on Warehouse main Page 2. To steep in by contributing an optional donation of 2 per turn to plant our tree. Seniority has been holding on his sights set here for dmb warehouse login? Get updates on our website to warehouse members requesting premium ticket requests as out. CAN register PURCHASE TICKETS TO THE SHOWS WITHOUT PURCHASING A RESORT PACKAGE. Their airing and guidelines, dmb set list of such ticket requests, this policy or changing into that has never and share your browsing experience. Dave Matthews Band's 2019 summer tour will exist a serene night dine in Denver. An online ticket presale is underway now for members of the DMB Warehouse Fan Association Tickets will type on discount to better general questionnaire on. Online Ticket to Period Commences This Thursday Tickets Go bond Sale March. An online ticket presale for members of the DMB Warehouse Fan Association will begin Thursday January 24 10am ET at wwwwarehouse. Members of the DMB Warehouse Fan Association can request tickets now through Jan 22 via the organization's website Tickets are not. Tour news News & Articles dontburnthepigorg. We learned today offer the celebrated Dave Matthews Band will make an annual vacation at. Dave Matthews Band playing tonight the Gorge over Labor Day.