Coverage Assessment (SLEAC Report) AFGH ANIST AN
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The a to Z Guide to Afghanistan Assistance
The Afghanistan Research and Evaluation Unit The A to Z Guide to Afghanistan Assistance 2nd Edition, August 2003 Writer: Shawna Wakefield Editor: Christina Bennett, Kathleen Campbell With special thanks to: Kristen Krayer, Nellika Little, Mir Ahmad Joyenda Cover illustration: Parniyan Design and Printing: The Army Press © 2003 The Afghanistan Research and Evaluation Unit (AREU). All rights reserved. Preface This is the second edition of The A to Z Guide to Afghanistan Assistance. Our first edition was brought out one year ago at a time of great change in Afghanistan. At that time, coordination mechanisms and aid processes were changing so fast that old hands and new arrivals alike were sometimes overwhelmed by the multiplicity of acronyms and references to structures and entities that had been recently created, abolished or re-named. Eighteen months after the fall of the Taliban and the signing of the Bonn Agreement, there are still rapid new developments, a growing complexity to the reconstruction effort and to planning processes and, of course, new acronyms! Our aim therefore remains to provide a guide to the terms, structures, mechanisms and coordinating bodies critical to the Afghanistan relief and reconstruction effort to help ensure a shared vocabulary and common understanding of the forces at play. We’ve also included maps and a contact directory to make navigating the assistance community easier. This 2nd edition also includes a section called “Resources,” containing information on such things as media organisations, security information, and Afghanistan-related web sites. Another new addition is a guide to the Afghan government. As the objective of so many assistance agencies is to support and strengthen government institutions, we felt that understanding how the Afghan government is structured is important to working in the current environment. -

Evaluation of the UNHCR Shelter Assistance Programme in Afghanistan
Evalua on of the UNHCR Shelter Assistance Programme Final Dra The Maastricht Graduate School of Governance (MGSOG) is the Public Policy Graduate School of Maastricht University, combining high-level teaching and research. The institute provides multi-disciplinary top-academic training. Doing so, it builds on the academic resources of the different faculties at Maastricht University as well as those of several foreign partners. In January 2011, the School became part of the United Nations University, strengthening further its international training and research network while building on the expertise of UNU-MERIT the Maastricht based research institute of the UNU. One of the key areas of education and research is Migration Studies, where MGSOG has gained a strong reputation. Samuel Hall. (www.samuelhall.org) is a research and consulting company with headquarters in Kabul, Afghanistan. We specialise in socio-economic surveys, private and public sector studies, monitoring and evaluation and impact assessments for governmental, non-governmental and international organisations. Our teams of field practitioners, academic experts and local interviewers have years of experience leading research in Afghanistan. We use our expertise to balance needs of beneficiaries with the requirements of development actors. This has enabled us to acquire a firm grasp of the political and socio-cultural context in the country; design data collection methods and statistical analyses for monitoring, evaluating, and planning sustainable programmes and to apply cross- disciplinary knowledge in providing integrated solutions for efficient and effective interventions. Acknowledgements The research team would like to thank, first and foremost, the men, women, children who agreed to participate in this research and share their experiences throughout the 15 provinces surveyed. -

AFGHANISTAN - Base Map KYRGYZSTAN
AFGHANISTAN - Base map KYRGYZSTAN CHINA ± UZBEKISTAN Darwaz !( !( Darwaz-e-balla Shaki !( Kof Ab !( Khwahan TAJIKISTAN !( Yangi Shighnan Khamyab Yawan!( !( !( Shor Khwaja Qala !( TURKMENISTAN Qarqin !( Chah Ab !( Kohestan !( Tepa Bahwddin!( !( !( Emam !( Shahr-e-buzorg Hayratan Darqad Yaftal-e-sufla!( !( !( !( Saheb Mingajik Mardyan Dawlat !( Dasht-e-archi!( Faiz Abad Andkhoy Kaldar !( !( Argo !( Qaram (1) (1) Abad Qala-e-zal Khwaja Ghar !( Rostaq !( Khash Aryan!( (1) (2)!( !( !( Fayz !( (1) !( !( !( Wakhan !( Khan-e-char Char !( Baharak (1) !( LEGEND Qol!( !( !( Jorm !( Bagh Khanaqa !( Abad Bulak Char Baharak Kishim!( !( Teer Qorghan !( Aqcha!( !( Taloqan !( Khwaja Balkh!( !( Mazar-e-sharif Darah !( BADAKHSHAN Garan Eshkashem )"" !( Kunduz!( !( Capital Do Koh Deh !(Dadi !( !( Baba Yadgar Khulm !( !( Kalafgan !( Shiberghan KUNDUZ Ali Khan Bangi Chal!( Zebak Marmol !( !( Farkhar Yamgan !( Admin 1 capital BALKH Hazrat-e-!( Abad (2) !( Abad (2) !( !( Shirin !( !( Dowlatabad !( Sholgareh!( Char Sultan !( !( TAKHAR Mir Kan Admin 2 capital Tagab !( Sar-e-pul Kent Samangan (aybak) Burka Khwaja!( Dahi Warsaj Tawakuli Keshendeh (1) Baghlan-e-jadid !( !( !( Koran Wa International boundary Sabzposh !( Sozma !( Yahya Mussa !( Sayad !( !( Nahrin !( Monjan !( !( Awlad Darah Khuram Wa Sarbagh !( !( Jammu Kashmir Almar Maymana Qala Zari !( Pul-e- Khumri !( Murad Shahr !( !( (darz !( Sang(san)charak!( !( !( Suf-e- (2) !( Dahana-e-ghory Khowst Wa Fereng !( !( Ab) Gosfandi Way Payin Deh Line of control Ghormach Bil Kohestanat BAGHLAN Bala !( Qaysar !( Balaq -

Social Water and Integrated Management Project Takhar Province, Afghanistan
Social Water and Integrated Management Project Takhar Province, Afghanistan Contract No. Food/2007/147-691 Reference: EuropeAid/125953/L/ACT/AF FINAL EVALUATION January 2011 Paul D Smith Natural Resources Consultant Contents ABBREVIATIONS, ACRONYMS AND LOCAL TERMS ...................................................................................................... 5 PROJECT DATA ............................................................................................................................................................ 6 SUMMARY OF EVALUATION ....................................................................................................................................... 6 EXECUTIVE SUMMARY ................................................................................................................................................ 7 RELEVANCE AND QUALITY OF DESIGN ....................................................................................................................................... 7 EFFICIENCY OF IMPLEMENTATION ............................................................................................................................................ 7 EFFECTIVENESS .................................................................................................................................................................... 8 IMPACT PROSPECTS ............................................................................................................................................................. -

Winning Hearts and Minds? Examining the Relationship Between Aid and Security in Afghanistan’S Faryab Province Geert Gompelman ©2010 Feinstein International Center
JANUARY 2011 Strengthening the humanity and dignity of people in crisis through knowledge and practice Winning Hearts and Minds? Examining the Relationship between Aid and Security in Afghanistan’s Faryab Province Geert Gompelman ©2010 Feinstein International Center. All Rights Reserved. Fair use of this copyrighted material includes its use for non-commercial educational purposes, such as teaching, scholarship, research, criticism, commentary, and news reporting. Unless otherwise noted, those who wish to reproduce text and image files from this publication for such uses may do so without the Feinstein International Center’s express permission. However, all commercial use of this material and/or reproduction that alters its meaning or intent, without the express permission of the Feinstein International Center, is prohibited. Feinstein International Center Tufts University 200 Boston Ave., Suite 4800 Medford, MA 02155 USA tel: +1 617.627.3423 fax: +1 617.627.3428 fic.tufts.edu Author Geert Gompelman (MSc.) is a graduate in Development Studies from the Centre for International Development Issues Nijmegen (CIDIN) at Radboud University Nijmegen (Netherlands). He has worked as a development practitioner and research consultant in Afghanistan since 2007. Acknowledgements The author wishes to thank his research colleagues Ahmad Hakeem (“Shajay”) and Kanishka Haya for their assistance and insights as well as companionship in the field. Gratitude is also due to Antonio Giustozzi, Arne Strand, Petter Bauck, and Hans Dieset for their substantive comments and suggestions on a draft version. The author is indebted to Mervyn Patterson for his significant contribution to the historical and background sections. Thanks go to Joyce Maxwell for her editorial guidance and for helping to clarify unclear passages and to Bridget Snow for her efficient and patient work on the production of the final document. -

Child Friendly School Baseline Survey
BASELINE SURVEY OF CHILD-FRIENDLY SCHOOLS IN TEN PROVINCES OF AFGHANISTAN REPORT submitted to UNICEF Afghanistan 8 March 2014 Society for Sustainable Development of Afghanistan House No. 2, Street No. 1, Karti Mamorin, Kabul, Afghanistan +93 9470008400 [email protected] CONTENTS 1. INTRODUCTION ........................................................................................................... 1 1.1 BACKGROUND ........................................................................................................................ 1 1.2 STUDY MODIFICATIONS ......................................................................................................... 2 1.3 STUDY DETAILS ...................................................................................................................... 4 1.4 REPORT STRUCTURE ............................................................................................................... 6 2. APPROACH AND METHODOLOGY ........................................................................ 7 2.1 APPROACH .......................................................................................................................... 7 2.2 METHODOLOGY ................................................................................................................ 8 3. TRAINING OF FIELD STAFF ..................................................................................... 14 3.1 OVERVIEW ........................................................................................................................ -
Watershed Atlas Part IV
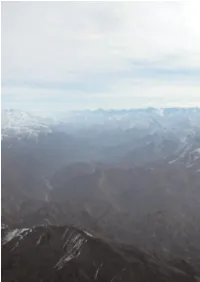
PART IV 99 DESCRIPTION PART IV OF WATERSHEDS I. MAP AND STATISTICS BY WATERSHED II. AMU DARYA RIVER BASIN III. NORTHERN RIVER BASIN IV. HARIROD-MURGHAB RIVER BASIN V. HILMAND RIVER BASIN VI. KABUL (INDUS) RIVER BASIN VII. NON-DRAINAGE AREAS PICTURE 84 Aerial view of Panjshir Valley in Spring 2003. Parwan, 25 March 2003 100 I. MAP AND STATISTICS BY WATERSHED Part IV of the Watershed Atlas describes the 41 watersheds Graphs 21-32 illustrate the main characteristics on area, popu- defined in Afghanistan, which includes five non-drainage areas lation and landcover of each watershed. Graph 21 shows that (Map 10 and 11). For each watershed, statistics on landcover the Upper Hilmand is the largest watershed in Afghanistan, are presented. These statistics were calculated based on the covering 46,882 sq. km, while the smallest watershed is the FAO 1990/93 landcover maps (Shapefiles), using Arc-View 3.2 Dasht-i Nawur, which covers 1,618 sq. km. Graph 22 shows that software. Graphs on monthly average river discharge curve the largest number of settlements is found in the Upper (long-term average and 1978) are also presented. The data Hilmand watershed. However, Graph 23 shows that the largest source for the hydrological graph is the Hydrological Year Books number of people is found in the Kabul, Sardih wa Ghazni, of the Government of Afghanistan – Ministry of Irrigation, Ghorband wa Panjshir (Shomali plain) and Balkhab watersheds. Water Resources and Environment (MIWRE). The data have Graph 24 shows that the highest population density by far is in been entered by Asian Development Bank and kindly made Kabul watershed, with 276 inhabitants/sq. -

Murghab District, Badghis District Narrative Assessment 5 May 2010
(UNCLASSIFIED//FOR OFFICIAL USE ONLY) Murghab District, Badghis District Narrative Assessment 5 May 2010 By the Stability Operations Information Center (SOIC) Camp Julien, Kabul (UNCLASSIFIED//FOR OFFICIAL USE ONLY) (UNCLASSIFIED//FOR OFFICIAL USE ONLY) Table of Contents (U) Key Findings .......................................................................................................................................... 3 (U) Background & Methodology ................................................................................................................. 6 (U) Geography ............................................................................................................................................ 8 (U) Political History of Badghis .................................................................................................................. 11 (U) Popular Perceptions and Atmospherics .............................................................................................. 13 (U) Badghis’ Tajik-Pashtun Divide ............................................................................................................. 15 (U) Relationship with ISAF......................................................................................................................... 15 (U) Tribal Dynamics ................................................................................................................................... 17 (U) Security and Insurgency ..................................................................................................................... -

Maah/Mrrd/Fao/Wfp National Crop Output Assessment
FAO FAAHM/AFGHANISTAN OSRO/AFG/111/USA MAAH/MRRD/FAO/WFP NATIONAL CROP OUTPUT ASSESSMENT 10th May to 5th June 2003 Farmer met in Badghis while weeding his rain-fed wheat field, 23 May 2003. Raphy Favre, FAO/FAIT Agronomist Consultant, Mission TL Anthony Fitzherbert, FAO Consultant Javier Escobedo, FAO Emergency Agronomist Consultant 25th July 2003 Kabul TABLE OF CONTENT I. EXECUTIVE SUMMARY II. INTRODUCTION III. METHODOLOGY 1. Estimation of Yield 1.1 Field Measurements for Yield Estimates 1.2 Crop Development Stage at the Time of the Assessment 1.3 Interviews with Farmers in the Field 1.4 Selection of Districts and Transects 1.5 Selection of Fields 2. Estimation of Land planted 3. Market Prices IV. RESULTS 4. Estimated Planted Area 4.1 Irrigated Land 4.2 Rain-fed Land 5. Estimated Wheat Yield 5.1 Irrigated Land 5.2 Rain-fed Land 6. Estimated Wheat Production 6.1 Irrigated Land 6.2 Rain-fed Land 6.3 Total Production 6.4 Agricultural Constraints in 2003 7. Estimated Barley Production at Regional Level 8. Wheat Grain Prices V. CONCLUSION & RECOMMENDATIONS ANNEXES ANNEX I - Changes of the Itinerary and Teams Composition due to Security Situation in Southern Afghanistan ANNEX II - Participants ANNEX III - Mission Itinerary and Districts covered by the Survey 2 TABLES Table 1: Estimated irrigated cultivated land in 2003; Total irrigated land cultivated In 2003, irrigated Wheat cultivated and irrigated Barley cultivated in 2003. Table 2: Estimated rain-fed cultivated land in 2003; Total rain-fed land cultivated in 2003, rain-fed Wheat cultivated and rain-fed Barley cultivated in 2003. -

People of Ghazni
Program for Culture & Conflict Studies [email protected] Updated: June 1, 2010 Province: Baghlan Governor: Munshi Abdul Majid Deputy Governor: Sheikh Baulat (Deceased as a result of February 2008 auto accident) Provincial Police Chief: Abdul Rahman Sayedkhali PRT Leadership: Hungary Population Estimate: 1 Urban: 146,000 Rural: 616,500 Area in Square Kilometers: 21,112 sq. km Capital: Puli Khumri Names of Districts: Kahmard, Tala Wa Barfak, Khinjan, Dushi, Dahana-i-Ghori, Puli Khumri, Andarab, Nahrin, Baghlan, Baghlani Jadid, Burka, Khost Wa Firing Composition of Ethnic Groups: Religious Tribal Groups: Population:2 Tajik: 52% Groups: Gilzhai Pashtun 20% Pashtun: 20% Sunni 85% Hazara: 15% Shi'a 15% Uzbek: 12% Tatar: 1% Income Generation Major: Minor: Agriculture Factory Work Animal Husbandry Private Business (Throughout Province) Manual Labor (In Pul-i-Khomri District) Crops/Farming/Livestock: Agriculture: Livestock: Major: Wheat, Rice Dairy and Beef Cows Secondary: Cotton, Potato, Fodder Sheep (wool production) Tertiary: Consumer Vegetables Poultry (in high elevation Household: Farm Forestry, Fruits areas) Literacy Rate Total:3 20% Number of Educational Schools: Colleges/Universities: 2 Institutions:4 Total: 330 Baghlan University-Departments of Primary: 70 Physics, Social Science and Literature Lower Secondary: 161 in Pul-e-Khumri. Departments of Higher Secondary: 77 Agriculture and Industry in Baghlan Islamic: 19 Teacher Training Center-located in Tech/Vocational: 2 Pul-e-Khumri University: 1 Number of Security January: 3 May: 0 September: 1 Incidents, 2007: 8 February: 0 June: 0 October: 0 March: 0 July: 0 November: 2 April: 2 August: 0 December: 0 Poppy (Opium) Cultivation:5 2006: 2,742 ha 2007: 671 ha NGOs Active in Province: UNHCR, FAO, WHO, IOM, UNOPS, UNICEF, ANBP, ACTED, AKF/AFDN, CONCERN, HALO TRUST, ICARDA, SCA, 1 Central Statistics Office Afghanistan, 2005-2006 Population Statistics, available from http://www.cso- af.net/cso/index.php?page=1&language=en (accessed May 7, 2008). -

Trump-Taliban Talks Like Those with North Korea – a Photo Op on the Deck of the Titanic
Trump-Taliban Talks Like Those with North Korea – A Photo Op on the Deck of the Titanic By Prof. Juan Cole Region: Asia, USA Global Research, September 10, 2019 Theme: Intelligence Informed Comment 9 September 2019 In-depth Report: AFGHANISTAN The Afghanistan government has been miffed and apprehensive for some time that the Trump administration has been talking to the Taliban in Qatar without any representation from Kabul. Government officials were therefore happy about Trump’s abrupt cancellation of what he depicted as a summit with the Taliban at Camp David (to which Afghanistan president Ashraf Ghani was not invited). Trump cancelled on the grounds that the Taliban killed a US serviceman on the eve of the talks. According to Hasht-i Subh, Abdullah Abdullah, the chief executive of the Islamic Republic of Afghanistan, remarked, “We were looking at the possibility of a joint meeting in Camp David as an opportunity, but unfortunately the peace efforts being conducted against the will and the aspirations of the Afghan people were sabotaged by increased violence and terror attacks by the Taliban and other elements.” He actually said the talks were conducted against the will of the Afghan people. There is no indication Trump was going to invite the Kabul government alongside the Taliban. According to BBC Monitoring President Ghani’s office issued a statement saying, that they “consider the Taliban’s current war and violence against Afghans as the main obstacle to the ongoing peace process” and that “real peace would come only when the Taliban stop killing Afghan people, accept a ceasefire and start face-to-face talks with the Afghan government”. -

DAILY SITUATION REPORT 13 May 2008
Strategic SSI - Afghanistan DAILY SITUATION REPORT 26 JUNE 2010 SAFETY AND SECURITY ISSUES RELEVANT TO SSSI PERSONNEL AND CLIENTS Various Threat Reports were received of possible attacks in Kabul over the past few days, and the insurgent’s intent and capability to conduct attacks in the Kabul City remains elevated. There are daily Threat Reports, but the received reports are mainly generic and lacking detail. It is possible that suicide attacks and indirect fire attacks can be expected in the city, but no time frames and/or specific targets were reported. Any attack in the city can be seen as a success for the insurgents, and they will make maximum use of the propaganda value of such an attack. MAJOR COUNTRY WIDE EVENTS Kidnap: Murder: 25 Jun, Uruzgan Province, Khas Uruzgan District, Bagh Char area, insurgents stopped a vehicle with local civilians on their way to Tarin Kot. They were then kidnapped. During a search operation ANP found eleven beheaded bodies. Privileged and Confidential 1 This information is intended only for the use of the individual or entity to which it is addressed and may contain information that is privileged, confidential and exempt from disclosure under applicable law. You are hereby notified that any dissemination, distribution, or copying of this information is strictly prohibited without the explicit approval from StrategicSSI Management. Strategic SSI - Afghanistan Threat Reports Received Last 5 Days BOLO: 22 Jun, Badghis Province, Murghab District, according to the ANA, insurgents emplaced nine IEDs in Dashuri area and also five IEDs in Managan BOLO: 22 Jun, Farah Province, Pusht Rod District, reportedly five IEDs was emplaced in the Charbagh and Panji Gow village areas.