Case 10 Brendan O'reilly
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Reference List Concerning De Quervain Tenosynovitis
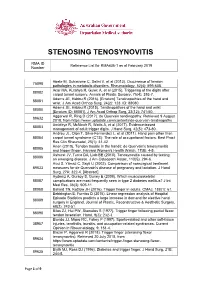
STENOSING TENOSYNOVITIS RMA ID Reference List for RMA436-1 as at February 2019 Number Abate M, Schiavone C, Salini V, et al (2013). Occurrence of tendon 75098 pathologies in metabolic disorders. Rheumatology, 52(4): 599-608. Acar MA, Kutahya H, Gulec A, et al (2015). Triggering of the digits after 88082 carpal tunnel surgery. Annals of Plastic Surgery, 75(4): 393-7. Adams JE, Habbu R (2016). [Erratum] Tendinopathies of the hand and 88081 wrist. J Am Acad Orthop Surg, 24(2): 123. ID: 88080. Adams JE, Habbu R (2015). Tendinopathies of the hand and wrist 88080 [Erratum ID: 88081]. J Am Acad Orthop Surg, 23(12): 741-50. Aggarwal R, Ring D (2017). de Quervain tendinopathy. Retrieved 9 August 89632 2018, from https://www.uptodate.com/contents/de-quervain-tendinopathy Amirfeyz R, McNinch R, Watts A, et al (2017). Evidence-based 88083 management of adult trigger digits. J Hand Surg, 42(5): 473-80. Andreu JL, Oton T, Silva-Fernandez L, et al (2011). Hand pain other than 88084 carpal tunnel syndrome (CTS): The role of occupational factors. Best Pract Res Clin Rheumatol, 25(1): 31-42. Anon (2010). Tendon trouble in the hands: de Quervain's tenosynovitis 88085 and trigger finger. Harvard Women's Health Watch, 17(8): 4-5. Ashurst JV, Turco DA, Lieb BE (2010). Tenosynovitis caused by texting: 88086 an emerging disease. J Am Osteopath Assoc, 110(5): 294-6. Avci S, Yilmaz C, Sayli U (2002). Comparison of nonsurgical treatment 89633 measures for de Quervain's disease of pregnancy and lactation. J Hand Surg, 27A: 322-4. -

De Quervain's Syndrome
De Quervain's syndrome What is it? Treatment options are: Through a transverse or longitudinal De Quervain's syndrome is a painful condition 1. Avoiding activities that cause pain, if incision, and protecting the nerve that affects tendons where they run through a possible branches just under the skin, the surgeon tunnel on the thumb side of the wrist. widens the tendon tunnel by slitting its roof. The tunnel roof forms again as the 2. Using a wrist/thumb splint, which can split heals, but it is wider and the What is the cause? often be obtained from a sports shop or a physiotherapist. It needs to immobilize tendons have sufficient room to move the thumb as well as the wrist. without pain. It appears without obvious cause in many cases. Pain relief is usually rapid. The scar may Mothers of small babies seem particularly prone 3. Steroid injection relieves the pain in be sore and unsightly for several weeks. to it, but whether this is due to hormonal Because the nerve branches were gently changes after pregnancy or due to lifting the about 70% of cases. The risks of injection are small, but it very occasionally causes moved to see the tunnel, transient baby repeatedly is not known. There is little temporary numbness can occur on the evidence that it is caused by work activities, but some thinning or colour change in the skin at the site of injection. back of the hand or thumb. Other risks the pain can certainly be aggravated by hand are the risks of any surgery such as use at work, at home, in the garden or at sport. -

(UED). a Health Care Provider Shall Determine the Nature of an Upper Extremity Disorder Before Initiating Treatment
1 REVISOR 5221.6300 5221.6300 UPPER EXTREMITY DISORDERS. Subpart 1. Diagnostic procedures for treatment of upper extremity disorders (UED). A health care provider shall determine the nature of an upper extremity disorder before initiating treatment. A. An appropriate history and physical examination must be performed and documented. Based on the history and physical examination the health care provider must at each visit assign the patient to the appropriate clinical category according to subitems (1) to (6). The diagnosis must be documented in the medical record. Patients may have multiple disorders requiring assignment to more than one clinical category. This part does not apply to upper extremity conditions due to a visceral, vascular, infectious, immunological, metabolic, endocrine, systemic neurologic, or neoplastic disease process, fractures, lacerations, amputations, or sprains or strains with complete tissue disruption. (1) Epicondylitis. This clinical category includes medial epicondylitis and lateral epicondylitis, ICD-9-CM codes 726.31 and 726.32. (2) Tendonitis of the forearm, wrist, and hand. This clinical category encompasses any inflammation, pain, tenderness, or dysfunction or irritation of a tendon, tendon sheath, tendon insertion, or musculotendinous junction in the upper extremity at or distal to the elbow due to mechanical injury or irritation, including, but not limited to, the diagnoses of tendonitis, tenosynovitis, tendovaginitis, peritendinitis, extensor tendinitis, de Quervain's syndrome, intersection syndrome, flexor tendinitis, and trigger digit, including, but not limited to, ICD-9-CM codes 726.4, 726.8, 726.9, 726.90, 727, 727.0, 727.00, 727.03, 727.04, 727.05, 727.09, 727.2, 727.3, 727.4 to 727.49, 727.8 to 727.82, 727.89, and 727.9. -
![De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH](https://docslib.b-cdn.net/cover/6782/de-quervains-tenosynovitis-11-lee-kh-kang-cn-lee-bg-a-case-control-study-with-prospe-tively-jung-ws-kim-dy-lee-ch-886782.webp)
De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH
Chapter De Quervain’s Tenosynovitis: Effective Diagnosis and Evidence-Based Treatment Jenson Mak Abstract De Quervain’s tenosynovitis (DQT) is a repetitive stress condition located at the first dorsal compartment of the wrist at the radial styloid. The extensor pollicis brevis (EPB) and abductor pollicis longus (APL) tendons and each tendon sheath are inflamed and this may result in thickening of the first dorsal extensor sheath. Workers who perform repetitive activities of the wrist and hand and those who rou- tinely use their thumbs in grasping and pinching motions in a repetitive manner are most susceptible to DQT. Conservative treatments include activity modification, modalities, orthotics, and manual therapy. This chapter identifies, in an evidence base manner through the literature, the most effective diagnostic measures for DQT. It also examines the evidence base on (or lack thereof) the treatment or treat- ment combinations to reduce pain and improve functional outcomes for patients with DQT. Keywords: De Quervain’s tenosynovitis, diagnosis, treatment, workplace, evidence-based 1. Introduction In 1893, Paul Jules Tillaux described a painful crepitus sign (Aïe crépitant de Tillaux)—tenosynovitis of the adductor and the short extensor of the thumb. In 1894, Fritz de Quervain, a Swiss surgeon, first described tenosynovitis on December 18, 1894, in Mrs. D., a 35-year-old woman who had severe pain in the extensor muscle region of the thumb, excluding tuberculosis. “It is a condition affecting the tendon sheaths of the abductor pollicis longus, and the extensor pollicis brevis. It has definite symptoms and signs. The condition may affect other extensor tendons at the wrist” [1]. -

Research Article Prevalence and Awareness Evaluation of De
Available online www.ijpras.com International Journal of Pharmaceutical Research & Allied Sciences, 2020, 9(4):151-157 ISSN : 2277-3657 Research Article CODEN(USA) : IJPRPM Prevalence and Awareness Evaluation of De Quervain’s Tenosynovitis among Students in the Kingdom of Saudi Arabia Bashar Reada1, Nawaf Alshaebi2*, Khalid Almaghrabi2, Abdullah Alshuaibi2, Arwa Abulnaja3, Khames Alzahrani4 1 Department of Medicine, MBBS, FSCSC, College of Medicine, King Abdulaziz University Hospital, Jeddah, KSA. 2 Department of Medicine, Undergraduate, College of Medicine, King Abdulaziz University, Jeddah, KSA. 3 Department of Medicine, Medical Intern, College of Medicine, King Abdulaziz University, Jeddah, KSA. 4 Department of Medicine, BDS, Ministry of Health, Jeddah, Saudi Arabia. *Email: nawafalshaebi @ hotmail.com ABSTRACT Introduction: De Quervain's tenosynovitis is characterized by inflammation and thickening of the tendons of the extensor pollicis brevis and abductor pollicis longus muscles and the synovial sheath, leading to a common cause of wrist pain that typically occurs in adults. This condition has been given several other names such as texting tenosynovitis, BlackBerry thumb, washerwoman's sprain, gamer’s thumb, teen texting tendonitis, WhatsAppitis, and radial styloid tenosynovitis, all of which involve repeated thumb pinching and wrist movement. Objectives: The purpose of this study was to determine the prevalence of de Quervain’s tenosynovitis among students using smartphones in Saudi Arabia. Many studies have been conducted on this disease in other countries, but not many have been performed in Saudi Arabia. Our aim was to obtain more information about the disease prevalence among students in Saudi Arabia. Our secondary objective was to determine the correlation of the condition with different demographics and risk factors in our study population, such as age, sex, and time spent texting. -

De Quervain's Syndrome
De Quervain’s Syndrome This leaflet offers more information about de Quervain’s syndrome. If you have any further questions or concerns, please speak to your hand therapist on the contact number given at the end of this leaflet. What is de Quervain’s and why have I got it? De Quervain’s syndrome, de Quervain’s tendinitis and de Quervain’s tenosynovitis are terms used to describe a tendinosis of the sheath or tunnel that covers two tendons that help move the thumb. Tendinosis is a name given to tendons that show chronic changes and thickening, rather than an acute inflammation. De Quervain’s syndrome is a set of symptoms that result from tendon degeneration, not inflammation. The two tendons involved are the tendons of the extensor pollicis brevis and abductor pollicis longus muscles of the thumb. These two muscles run side by side in their tunnel and both move the thumb away from the hand. The cause of de Quervain’s syndrome is not known, however it is much more common in women. Extensor pollicis brevis Abductor pollicis longus What are the signs and symptoms? De Quervain’s syndrome is characterised by pain and localised swelling at the base of thumb and the thumb side of the wrist. Pain is often worse with activities that involve gripping and squeezing combined with bending the wrist, such as when squeezing out a cloth or lifting up objects. This pain can spread into the thumb, up the arm and can be very limiting. Page 1 of 3 How can hand therapy help? Hand therapy treatment for de Quervain’s syndrome can help manage the symptoms, but there is no evidence that certain treatments work better than others. -

Functional Diagnostics and Physiotherapeutic Treatment in De Quervain Syndrome / Diagnostyka Funkcjonalna I Leczenie Fizjoterapeutyczne W Zespole De Quer
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/342083638 FUNCTIONAL DIAGNOSTICS AND PHYSIOTHERAPEUTIC TREATMENT IN DE QUERVAIN SYNDROME / DIAGNOSTYKA FUNKCJONALNA I LECZENIE FIZJOTERAPEUTYCZNE W ZESPOLE DE QUER.... Article in Health Problems of Civilization · June 2020 DOI: 10.5114/hpc.2020.95502 CITATIONS READS 0 233 1 author: Kamil Zaworski Pope John Paul II State School of Higher Education 25 PUBLICATIONS 12 CITATIONS SEE PROFILE All content following this page was uploaded by Kamil Zaworski on 10 June 2020. The user has requested enhancement of the downloaded file. REVIEW PAPER Health Problems of Civilization ISSN 2353-6942 ARTYKUŁ PRZEGLĄDOWY FUNCTIONAL DIAGNOSTICS AND PHYSIOTHERAPEUTIC TREATMENT IN DE QUERVAIN SYNDROME DIAGNOSTYKA FUNKCJONALNA I LECZENIE FIZJOTERAPEUTYCZNE W ZESPOLE DE QUERVAINA Kamil Zaworski 1(A,B,D,E,F) 1 Pope John Paul II State School of Higher Education in Biała Podlaska, Poland Summary Authors’ contribution Wkład autorów: De Quervain syndrome involves the inflammation of the common tendon sheath of the A. Study design/planning abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) in the region of the zaplanowanie badań radial styloid process. This condition can be caused by microtraumas that occur in the course B. Data collection/entry of repetitive mechanical activities and systemic diseases of the connective tissue, such as zebranie danych rheumatoid arthritis. The symptom of de Quervain syndrome is pain in the forearm at the C. Data analysis/statistics height of the radial styloid process. The pain intensifies during the extension of the thumb. interpretacjadane – analiza danych i statystyki Other symptoms include redness and swelling in the region. -

Wrist, Hand and Thumb Osteoarthritis
MSK self-management workbook Osteoarthritis (oa) of the wrist, hand and thumb DeQuervain’s Tenosynovitis July 2020 MSK Wrist and Hand Disclaimer This workbook provides general advice which may not be specific to you. It is important that if you are in pain that you see a health care professional for an assessment to rule out serious, albeit rare, pathology. Please talk to a health care provider if you have not seen one before. This workbook can be used on your own, however, we recommend that you do so alongside a health professional. Health and safety This workbook is designed to help you manage your condition. It is recommended that the workbook is used alongside advice from a health professional. Together you can work to help with your recovery. You may progress more rapidly or slowly through this workbook depending on your symptoms and other factors related to your condition. It is important that if you are experiencing pain during the activities in this workbook then you should discuss your symptoms with a health professional. Purpose of workbook This workbook provides a general overview of the management of your condition. The workbook is split into different sections with the main focus being education, self-management advice and exercise. We recommend reading all the sections over time, however, you may find that not all of this information is relevant to you. The exercise section gives you a choice of exercises, varying in difficulty. Begin with the level you feel is appropriate, based on your pain and confidence. You then have the option over time to make these exercises more challenging or reduce to a more basic level as required. -

De Quervain's Release Standard of Care PT
BRIGHAM & WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: de Quervain’s Syndrome: Surgical Management Physical Therapy management of the patient who had a release of the first extensor compartment. Case Type/Diagnosis: (diagnosis specific, impairment/dysfunction specific) 11 Since the first description of “washerwoman’s sprain” tenosynovitis of the first dorsal compartment has become a commonly recognized inflammatory disorder. The most radial of the extensor compartments on the dorsum of the wrist is occupied by the tendons of the extensor pollicis brevis and abductor pollicis longus. The tendons are enveloped in an osseofibrous canal lined by synovium, which, when subjected to excessive or repetitive mechanical stresses, responds in a characteristic fashion distinguished by pain, swelling, and limitation of motion of the thumb. In 1895,Fritz de Quervain, a Swiss surgeon, 1 was first credited with the recognition of this disease and so it bore his name. More accurately, Tillaux 2 and Gray 3 referred to this disorder before de Quervain. Anatomy: Twenty-four extrinsic tendons cross the wrist and provide power and dexterity in the hand. Each tendon passes through a series of tight fibrous -osseous canals designed to optimize the balance between motion and force production by maintaining the tendon in close approximation to the joint or joints it controls. There are six separate compartments under the dorsal carpal ligament each lined with a separate synovial sheath membrane. The first one is over the radial styloid and it contains the abductor pollicis longus and the extensor pollicis brevis tendons. These tendons pass through an unyielding osteoligamentous tunnel formed by a shallow groove in the radial styloid process and a tough overlying roof composed by the transverse fibers of the dorsal ligament. -

Information for Patients About Hand & Elbow Surgery
Information for Patients about Hand & Elbow Surgery Clinical Professor Allan Wang FRACS PhD FAOrthA Shoulder and Upper Limb Surgeon www.allanwangorthopaedics.com.au MURDOCH SUBIACO Murdoch Orthopaedic Clinic St John of God Subiaco Clinic St John of God Murdoch Clinic Suite 302, 25 McCourt St Suite 10, 100 Murdoch Drive Subiaco WA 6008 Murdoch WA 6150 Telephone: 08 6332 6390 Page | 2 Page | 3 Information for Patients about Hand and Elbow Surgery Introduction We have put this information booklet together to educate our patients about their Hand and Elbow condition, treatment options and post-surgical care. Please keep this booklet for future reference. It is not a detailed source of information and you may also wish to refer to our website www.allanwangorthopaedics.com.au for animated videos of surgical procedures. If you require further information or have concerns regarding your treatment please contact the office to discuss with Dr Wang or his staff. Contents Pages 1. Carpal Tunnel Syndrome 4 2. Cubital Tunnel Syndrome 6 3. Trigger Finger 7 4. De Quervain’s Tenodonitis 8 5. Ganglion Cysts 9 6. Arthritis at the Base of the Thumb 10 7. Wrist Arthroscopy 11 8. Dupuytren’s Disease 12 9. Lateral Epicondylitis 13 10. Elbow Arthroscopy 14 11. Post-Operative Instructions Hand & Elbow Surgery 15 Page | 4 Carpal Tunnel Syndrome What is it? Figure 1 Carpal tunnel syndroe is a condition aused by copression o te median nerve at te level o te wrist oint Here te edian nerve passes into te arpal tunnel along wit leor tendons and te tendon lining called tenosynoviu Carpal tunnel syndroe ocurs wen pressure builds up in te tunnel and tis an be due to swelling o te tenosynoviu ratures artritis luid retention during pregnany and certain conditions suc as diabetes and tyroid disease Symptoms en te pressure on te edian nerve becoes severe, you ay notice wrist pain tingling and nubness and lusiness in and oveents. -

Anti-Inflammatory Therapy in Tendinopathy: the Role Of
22 Anti-Inflammatory Therapy in Tendinopathy: The Role of Nonsteroidal Drugs and Corticosteroid Injections Wayne B. Leadbetter Anti-inflammatory therapy is commonly prescribed for Tissue Response to Tendon Injury the treatment of musculoskeletal soft tissue injury and tendinopathy [1–6]. Since either acute macrotraumatic or Because the most common objectives of anti-inflamma- chronic microtraumatic injury is often associated with tory therapy in tendon injury are the relief of excessive pain, stiffness, swelling, and loss of function, historically pain and inflammation, the following brief discussion may cardinal signs of an inflammatory process, nonsteroidal prove useful in forming a rationale for such treatment. anti-inflammatory drugs (NSAIDs) and a variety of syn- Injury is characterized as acute (i.e. macrotraumatic) or thetic derivatives of cortisol, an adrenal glucocorticoid, chronic (i.e. microtraumatic, overuse, cumulative trauma, have achieved widespread endorsement [1,7]. The popu- or repetitive motion disorder) [16,17]. Acute human larity of these agents testifies to the prevalent belief that tissue response is characterized by three phases: 1) acute such medical intervention can relieve the initial dis- vascular-inflammatory; 2) repair-regeneration; and 3) ability and improve the rate of recovery from injury.This maturation [18]. In normal tissue healing, inflammation utilization pattern has been documented by surveys plays an important initial role in this complex dynamic revealing that more than 17 million Americans consume process. The resulting restoration of anatomic tissue NSAIDs daily, and some 50 million Americans use continuity is the product of an orderly, progressive, and NSAIDs intermittently or routinely yearly; up to 30 interdependent biologic repair sequence. -

January 2012
THE UNIVERSITY OF TOLEDO MEDICAL CENTER ORTHOPAEDIC MONTHLY Growth in Children: Epiphyseal Contribution of Long Bone Growth There are growth plates within the long bones with varying distributions across the bone. The growth distribution in the humerus is about 80 percent in the proximal area and about 20 percent in the distal area. Displaced fractures of the proximal humerus in children are usually treated without surgery. The growth distribution in the ulna is about 80 percent proximal and about 20 percent in the distal area. Growth arrest in fracture involving the distal ulna is approximately 50 percent. Within the radius, about 25 percent of growth occurs in the proximal area, while 75 percent occurs in the distal area. Fractures at the distal radius usually heal and correct their angulation after closed reduction. Surgery is rarely necessary. Fractures involving the growth plates of the distal radius rarely involve growth arrest. Within the femur, the growth distribution is about 30 percent in the proximal area and about 70 percent in the distal area. Within the tibia, the growth distribution is about 55 percent Fractures involving the growth plates of the distal femur may cause proximal and 45 percent distal. In the fibula, growth distribution is major growth disturbances. It is expected that a child grows 1 cm per about 60 percent proximal and 40 percent distal. year from the distal femur growth plate. Males will grow-up until the A growth spurt occurs at the time of puberty. Puberty typically age of 16 years old, while females will grow-up until 14 years of age.