Hand and Wrist Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Nearly Invisible Intraneural Cyst: a New and Emerging Part of the Spectrum
NEUROSURGICAL FOCUS Neurosurg Focus 42 (3):E10, 2017 The nearly invisible intraneural cyst: a new and emerging part of the spectrum Thomas J. Wilson, MD,1 Marie-Noëlle Hébert-Blouin, MD,2 Naveen S. Murthy, MD,3 Joaquín J. García, MD,4 Kimberly K. Amrami, MD,3 and Robert J. Spinner, MD1 Departments of 1Neurosurgery, 3Radiology, and 4Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota; and 2Department of Neurosurgery, McGill University Health Centre, Montreal, Quebec, Canada OBJECTIVE The authors have observed that a subset of patients referred for evaluation of peroneal neuropathy with “negative” findings on MRI of the knee have subtle evidence of a peroneal intraneural ganglion cyst on subsequent closer inspection. The objective of this study was to introduce the nearly invisible peroneal intraneural ganglion cyst and provide illustrative cases. The authors further wanted to identify clues to the presence of a nearly invisible cyst. METHODS Illustrative cases demonstrating nearly invisible peroneal intraneural ganglion cysts were retrospectively reviewed and are presented. Case history and physical examination, imaging, and intraoperative findings were reviewed for each case. The outcomes of interest were the size and configuration of peroneal intraneural ganglion cysts over time, relative to various interventions that were performed, and in relation to physical examination and electrodiagnostic find- ings. RESULTS The authors present a series of cases that highlight the dynamic nature of peroneal intraneural ganglion cysts and introduce the nearly invisible cyst as a new and emerging part of the spectrum. The cases demonstrate changes in size and morphology over time of both the intraneural and extraneural compartments of these cysts. -

Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -
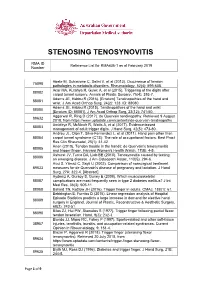
Reference List Concerning De Quervain Tenosynovitis
STENOSING TENOSYNOVITIS RMA ID Reference List for RMA436-1 as at February 2019 Number Abate M, Schiavone C, Salini V, et al (2013). Occurrence of tendon 75098 pathologies in metabolic disorders. Rheumatology, 52(4): 599-608. Acar MA, Kutahya H, Gulec A, et al (2015). Triggering of the digits after 88082 carpal tunnel surgery. Annals of Plastic Surgery, 75(4): 393-7. Adams JE, Habbu R (2016). [Erratum] Tendinopathies of the hand and 88081 wrist. J Am Acad Orthop Surg, 24(2): 123. ID: 88080. Adams JE, Habbu R (2015). Tendinopathies of the hand and wrist 88080 [Erratum ID: 88081]. J Am Acad Orthop Surg, 23(12): 741-50. Aggarwal R, Ring D (2017). de Quervain tendinopathy. Retrieved 9 August 89632 2018, from https://www.uptodate.com/contents/de-quervain-tendinopathy Amirfeyz R, McNinch R, Watts A, et al (2017). Evidence-based 88083 management of adult trigger digits. J Hand Surg, 42(5): 473-80. Andreu JL, Oton T, Silva-Fernandez L, et al (2011). Hand pain other than 88084 carpal tunnel syndrome (CTS): The role of occupational factors. Best Pract Res Clin Rheumatol, 25(1): 31-42. Anon (2010). Tendon trouble in the hands: de Quervain's tenosynovitis 88085 and trigger finger. Harvard Women's Health Watch, 17(8): 4-5. Ashurst JV, Turco DA, Lieb BE (2010). Tenosynovitis caused by texting: 88086 an emerging disease. J Am Osteopath Assoc, 110(5): 294-6. Avci S, Yilmaz C, Sayli U (2002). Comparison of nonsurgical treatment 89633 measures for de Quervain's disease of pregnancy and lactation. J Hand Surg, 27A: 322-4. -

De Quervain's Syndrome
De Quervain's syndrome What is it? Treatment options are: Through a transverse or longitudinal De Quervain's syndrome is a painful condition 1. Avoiding activities that cause pain, if incision, and protecting the nerve that affects tendons where they run through a possible branches just under the skin, the surgeon tunnel on the thumb side of the wrist. widens the tendon tunnel by slitting its roof. The tunnel roof forms again as the 2. Using a wrist/thumb splint, which can split heals, but it is wider and the What is the cause? often be obtained from a sports shop or a physiotherapist. It needs to immobilize tendons have sufficient room to move the thumb as well as the wrist. without pain. It appears without obvious cause in many cases. Pain relief is usually rapid. The scar may Mothers of small babies seem particularly prone 3. Steroid injection relieves the pain in be sore and unsightly for several weeks. to it, but whether this is due to hormonal Because the nerve branches were gently changes after pregnancy or due to lifting the about 70% of cases. The risks of injection are small, but it very occasionally causes moved to see the tunnel, transient baby repeatedly is not known. There is little temporary numbness can occur on the evidence that it is caused by work activities, but some thinning or colour change in the skin at the site of injection. back of the hand or thumb. Other risks the pain can certainly be aggravated by hand are the risks of any surgery such as use at work, at home, in the garden or at sport. -

(UED). a Health Care Provider Shall Determine the Nature of an Upper Extremity Disorder Before Initiating Treatment
1 REVISOR 5221.6300 5221.6300 UPPER EXTREMITY DISORDERS. Subpart 1. Diagnostic procedures for treatment of upper extremity disorders (UED). A health care provider shall determine the nature of an upper extremity disorder before initiating treatment. A. An appropriate history and physical examination must be performed and documented. Based on the history and physical examination the health care provider must at each visit assign the patient to the appropriate clinical category according to subitems (1) to (6). The diagnosis must be documented in the medical record. Patients may have multiple disorders requiring assignment to more than one clinical category. This part does not apply to upper extremity conditions due to a visceral, vascular, infectious, immunological, metabolic, endocrine, systemic neurologic, or neoplastic disease process, fractures, lacerations, amputations, or sprains or strains with complete tissue disruption. (1) Epicondylitis. This clinical category includes medial epicondylitis and lateral epicondylitis, ICD-9-CM codes 726.31 and 726.32. (2) Tendonitis of the forearm, wrist, and hand. This clinical category encompasses any inflammation, pain, tenderness, or dysfunction or irritation of a tendon, tendon sheath, tendon insertion, or musculotendinous junction in the upper extremity at or distal to the elbow due to mechanical injury or irritation, including, but not limited to, the diagnoses of tendonitis, tenosynovitis, tendovaginitis, peritendinitis, extensor tendinitis, de Quervain's syndrome, intersection syndrome, flexor tendinitis, and trigger digit, including, but not limited to, ICD-9-CM codes 726.4, 726.8, 726.9, 726.90, 727, 727.0, 727.00, 727.03, 727.04, 727.05, 727.09, 727.2, 727.3, 727.4 to 727.49, 727.8 to 727.82, 727.89, and 727.9. -

Top Hand, and Wrist Problems
12/10/2016 TOP HAND, AND WRIST Disclosures PROBLEMS: HOW TO • None SPOT THEM IN CLINIC Nicolas H. Lee, MS MD [email protected] UCSF Dept of Orthopaedic Surgery Assistant Clinical Professor Hand, Upper Extremity and Microvascular Surgery Dec. 10 th , 2016 Outline Outline • Carpal Tunnel Syndrome •Carpal Tunnel Syndrome • Trigger Finger • • Basal Joint arthritis Trigger Finger • Basal Joint arthritis • De Quervain tenosynovitis • De Quervain tenosynovitis • Mallet Finger • Mallet Finger • Ganglion cyst • Ganglion cyst 1 12/10/2016 Carpal Tunnel Syndrome • Compression of median nerve in carpal tunnel • Irritation of the nerve presents as numbness/pain 10 structures 9 flexor tendons Median nerve https://www.pinterest.com/pin/429812358163325007/ Anatomy (motor) Etiology 1. Idiopathic – most common 2. Anatomic – rare • Thenar Muscle (OAF) 3. Systemic – DM, hypothyroidism • Opponens Pollicis (deep) 4. **** Occupational Exposure • Abductor Pollicis Brevis (superficial) **** “A direct relationship between repetitive work • Flexor Pollicis Brevis activity (eg, keyboarding) and CTS has never been (superficial 1/2) objectively demonstrated.” 1 http://teachmeanatomy.info/upper-limb/muscles/hand/ 2 12/10/2016 Rare anatomic causes Carpal Tunnel Syndrome ● HPI – systemic risk factors Tenosynovitis CMC arthritis ◦ More common in: Ganglion Fracture 1) Diabetics 2) Hypothyroidism 3) Pregnancy (20-45%) Persistent Median artery Acromegaly Abnormal muscle Tumor Carpal Tunnel Syndrome ● CC: ◦ “I wake up at night and my hands are asleep” ◦ “I have to shake them to get the blood flowing again” ◦ “I have to run them under warm water and then I can go back to sleep” ◦ “Fingers go numb when I drive” ◦ “My hand goes numb when I use my cell phone” ◦ “I am always dropping things” Carpal Tunnel Syndrome Cranford, C.S. -

Cytomorphological Study of Articular and Periarticular Cystic Lesions Dr.Sneha Saini, Dr.Madhu Sinha , Dr
International J. of Healthcare and Biomedical Research, Volume: 06, Issue: 04, July 2018, 23- 36 Original article: Cytomorphological study of articular and periarticular cystic lesions Dr.Sneha Saini, Dr.Madhu Sinha , Dr. Natasha S. Gulati , Dr. Abhijit Das, Dr. Man Mohan Mehndiratta 1. Dr.Sneha Saini- Senior Resident, Janakpuri Superspeciality Hospital (JSSH) 2. Dr.Madhu Sinha- Specialist(Pathology), Janakpuri Superspeciality Hospital (JSSH) 3. Dr. Natasha S. Gulati- Specialist(Cytology), Janakpuri Superspeciality Hospital (JSSH) 4. Dr. Abhijit Das- Assistant Professor, Janakpuri Superspeciality Hospital (JSSH) 5. Dr. Man Mohan Mehndiratta, Director, Janakpuri Superspeciality Hospital (JSSH) Corresponding Author: Dr.Sneha Saini , Senior Resident, Janakpuri Superspeciality Hospital (JSSH) ABSTRACT: AIMS AND OBJECTIVES:- To study cytomorphology of articular and periarticular cystic lesions and to assess the efficacy of fine needle aspiration cytology (FNAC) in diagnosis and management of articular and periarticular cystic lesions. MATERIAL AND METHODS:- Our study was a retrospective study done over a period of 2 years from Jan 2015 to Jan 2017 in Cytology section of Pathology department of our hospital. Sixteen cases including ganglion cysts, synovial cysts and popliteal cysts from different articular and periarticular sites were studied. RESULTS:- In our study out of 16 cases, there were 10 (62.5%) cases of ganglion cysts, 3 (18.7%) cases of synovial cysts and 3 (18.7%) cases of popliteal cysts. The male to female ratio (M: F) for these lesions was 1:1.6 and were predominantly found in third decade (21-30 years). CONCLUSION:- FNAC offers a great diagnostic utility in articular and periarticular cystic lesions being an OPD procedure having low cost. -
![De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH](https://docslib.b-cdn.net/cover/6782/de-quervains-tenosynovitis-11-lee-kh-kang-cn-lee-bg-a-case-control-study-with-prospe-tively-jung-ws-kim-dy-lee-ch-886782.webp)
De Quervain's Tenosynovitis: [11] Lee KH, Kang CN, Lee BG, a Case-Control Study with Prospe Tively Jung WS, Kim DY, Lee CH
Chapter De Quervain’s Tenosynovitis: Effective Diagnosis and Evidence-Based Treatment Jenson Mak Abstract De Quervain’s tenosynovitis (DQT) is a repetitive stress condition located at the first dorsal compartment of the wrist at the radial styloid. The extensor pollicis brevis (EPB) and abductor pollicis longus (APL) tendons and each tendon sheath are inflamed and this may result in thickening of the first dorsal extensor sheath. Workers who perform repetitive activities of the wrist and hand and those who rou- tinely use their thumbs in grasping and pinching motions in a repetitive manner are most susceptible to DQT. Conservative treatments include activity modification, modalities, orthotics, and manual therapy. This chapter identifies, in an evidence base manner through the literature, the most effective diagnostic measures for DQT. It also examines the evidence base on (or lack thereof) the treatment or treat- ment combinations to reduce pain and improve functional outcomes for patients with DQT. Keywords: De Quervain’s tenosynovitis, diagnosis, treatment, workplace, evidence-based 1. Introduction In 1893, Paul Jules Tillaux described a painful crepitus sign (Aïe crépitant de Tillaux)—tenosynovitis of the adductor and the short extensor of the thumb. In 1894, Fritz de Quervain, a Swiss surgeon, first described tenosynovitis on December 18, 1894, in Mrs. D., a 35-year-old woman who had severe pain in the extensor muscle region of the thumb, excluding tuberculosis. “It is a condition affecting the tendon sheaths of the abductor pollicis longus, and the extensor pollicis brevis. It has definite symptoms and signs. The condition may affect other extensor tendons at the wrist” [1]. -

Research Article Prevalence and Awareness Evaluation of De
Available online www.ijpras.com International Journal of Pharmaceutical Research & Allied Sciences, 2020, 9(4):151-157 ISSN : 2277-3657 Research Article CODEN(USA) : IJPRPM Prevalence and Awareness Evaluation of De Quervain’s Tenosynovitis among Students in the Kingdom of Saudi Arabia Bashar Reada1, Nawaf Alshaebi2*, Khalid Almaghrabi2, Abdullah Alshuaibi2, Arwa Abulnaja3, Khames Alzahrani4 1 Department of Medicine, MBBS, FSCSC, College of Medicine, King Abdulaziz University Hospital, Jeddah, KSA. 2 Department of Medicine, Undergraduate, College of Medicine, King Abdulaziz University, Jeddah, KSA. 3 Department of Medicine, Medical Intern, College of Medicine, King Abdulaziz University, Jeddah, KSA. 4 Department of Medicine, BDS, Ministry of Health, Jeddah, Saudi Arabia. *Email: nawafalshaebi @ hotmail.com ABSTRACT Introduction: De Quervain's tenosynovitis is characterized by inflammation and thickening of the tendons of the extensor pollicis brevis and abductor pollicis longus muscles and the synovial sheath, leading to a common cause of wrist pain that typically occurs in adults. This condition has been given several other names such as texting tenosynovitis, BlackBerry thumb, washerwoman's sprain, gamer’s thumb, teen texting tendonitis, WhatsAppitis, and radial styloid tenosynovitis, all of which involve repeated thumb pinching and wrist movement. Objectives: The purpose of this study was to determine the prevalence of de Quervain’s tenosynovitis among students using smartphones in Saudi Arabia. Many studies have been conducted on this disease in other countries, but not many have been performed in Saudi Arabia. Our aim was to obtain more information about the disease prevalence among students in Saudi Arabia. Our secondary objective was to determine the correlation of the condition with different demographics and risk factors in our study population, such as age, sex, and time spent texting. -

Intraosseous Ganglion Cyst of the Humeral Head in a Competitive Flat Water Paddler: Case Report
0008-3194/2011/294–301/$2.00/©JCCA 2011 Intraosseous ganglion cyst of the humeral head in a competitive flat water paddler: case report Brad Muir, HBSc (Kin), DC, FRCCSS(C)* Jaclyn A. Kissel, BSc, DC, FRCCSS(C) Dominique Forand Yedon, BScKin, DC, FRCCSS(C) Objective: To present the diagnostic and clinical features Objectif : soumettre un diagnostic et les caractéristiques of an intraosseous ganglion cyst of the humeral head of cliniques d’un kyste ganglionnaire intraosseux de la a female flat water canoe athlete. tête humérale d’une athlète pratiquant le canoë en eau Clinical Features: An 18-year old female flat water plate. canoeist complaining of right shoulder pain following a Caractéristiques cliniques : une canoéiste en eau plate strenuous paddling training camp. de 18 ans se plaint de douleurs à l’épaule droite suite à Intervention and outcome: A trial of passive care un camp d’entraînement très exigeant. was conducted, including soft tissue therapy, spinal Intervention et résultat : un essai de soins passifs manipulative therapy, acupuncture, and rehabilitation. fut mené, notamment la thérapie des parties molles, The patient seemed to be responding with treatment, but la manipulation rachidienne, l’acupuncture et la pain would always resume with paddling. A diagnostic réhabilitation. La patiente semble avoir bien réagi ultrasound displayed mild thickening and effusion in the au traitement, mais la douleur revient lorsqu’elle subacromial/subdeltoid bursae. Continued passive care recommence à ramer. Un ultrason diagnostic démontra was not able to resolve the symptoms and she underwent un épaississement léger et une effusion dans les an MRI which revealed an intraosseus ganglion cyst bourses sous-acromiales/des courts rotateurs de subjacent to the lesser tuberosity and floor of the l’épaule. -

De Quervain's Syndrome
De Quervain’s Syndrome This leaflet offers more information about de Quervain’s syndrome. If you have any further questions or concerns, please speak to your hand therapist on the contact number given at the end of this leaflet. What is de Quervain’s and why have I got it? De Quervain’s syndrome, de Quervain’s tendinitis and de Quervain’s tenosynovitis are terms used to describe a tendinosis of the sheath or tunnel that covers two tendons that help move the thumb. Tendinosis is a name given to tendons that show chronic changes and thickening, rather than an acute inflammation. De Quervain’s syndrome is a set of symptoms that result from tendon degeneration, not inflammation. The two tendons involved are the tendons of the extensor pollicis brevis and abductor pollicis longus muscles of the thumb. These two muscles run side by side in their tunnel and both move the thumb away from the hand. The cause of de Quervain’s syndrome is not known, however it is much more common in women. Extensor pollicis brevis Abductor pollicis longus What are the signs and symptoms? De Quervain’s syndrome is characterised by pain and localised swelling at the base of thumb and the thumb side of the wrist. Pain is often worse with activities that involve gripping and squeezing combined with bending the wrist, such as when squeezing out a cloth or lifting up objects. This pain can spread into the thumb, up the arm and can be very limiting. Page 1 of 3 How can hand therapy help? Hand therapy treatment for de Quervain’s syndrome can help manage the symptoms, but there is no evidence that certain treatments work better than others. -

Functional Diagnostics and Physiotherapeutic Treatment in De Quervain Syndrome / Diagnostyka Funkcjonalna I Leczenie Fizjoterapeutyczne W Zespole De Quer
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/342083638 FUNCTIONAL DIAGNOSTICS AND PHYSIOTHERAPEUTIC TREATMENT IN DE QUERVAIN SYNDROME / DIAGNOSTYKA FUNKCJONALNA I LECZENIE FIZJOTERAPEUTYCZNE W ZESPOLE DE QUER.... Article in Health Problems of Civilization · June 2020 DOI: 10.5114/hpc.2020.95502 CITATIONS READS 0 233 1 author: Kamil Zaworski Pope John Paul II State School of Higher Education 25 PUBLICATIONS 12 CITATIONS SEE PROFILE All content following this page was uploaded by Kamil Zaworski on 10 June 2020. The user has requested enhancement of the downloaded file. REVIEW PAPER Health Problems of Civilization ISSN 2353-6942 ARTYKUŁ PRZEGLĄDOWY FUNCTIONAL DIAGNOSTICS AND PHYSIOTHERAPEUTIC TREATMENT IN DE QUERVAIN SYNDROME DIAGNOSTYKA FUNKCJONALNA I LECZENIE FIZJOTERAPEUTYCZNE W ZESPOLE DE QUERVAINA Kamil Zaworski 1(A,B,D,E,F) 1 Pope John Paul II State School of Higher Education in Biała Podlaska, Poland Summary Authors’ contribution Wkład autorów: De Quervain syndrome involves the inflammation of the common tendon sheath of the A. Study design/planning abductor pollicis longus (APL) and the extensor pollicis brevis (EPB) in the region of the zaplanowanie badań radial styloid process. This condition can be caused by microtraumas that occur in the course B. Data collection/entry of repetitive mechanical activities and systemic diseases of the connective tissue, such as zebranie danych rheumatoid arthritis. The symptom of de Quervain syndrome is pain in the forearm at the C. Data analysis/statistics height of the radial styloid process. The pain intensifies during the extension of the thumb. interpretacjadane – analiza danych i statystyki Other symptoms include redness and swelling in the region.