Monoaminergic System and Depression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Serotonin's Role in Alcohol's Effects on the Brain
NEUROTRANSMITTER REVIEW IMPERATO, A., AND DI CHIARA, G. Preferential stimulation of dopamine release in the nucleus accumbens of freely moving rats by ethanol. Journal SEROTONIN’S ROLE IN ALCOHOL’S of Pharmacology and Experimental Therapeutics 239:219–228, 1986. EFFECTS ON THE BRAIN KITAI, S.T., AND SURMEIER, D.J. Cholinergic and dopaminergic modula- tion of potassium conductances in neostriatal neurons. Advances in David M. Lovinger, Ph.D. Neurology 60:40–52, 1993. LE MOINE, C.; NORMAND, E.; GUITTENY, A.F.; FOUQUE, B.; TEOULE, R.; AND BLOCH, B. Dopamine receptor gene expression by enkephalin Serotonin is an important brain chemical that acts as a neurons in rat forebrain. Proceedings of the National Academy of Sciences neurotransmitter to communicate information among USA 87:230–234, 1990. nerve cells. Serotonin’s actions have been linked to al- LE MOINE, C.; NORMAND, E.; AND BLOCH, B. Phenotypical character- cohol’s effects on the brain and to alcohol abuse. ization of the rat striatal neurons expressing the D1 dopamine receptor Alcoholics and experimental animals that consume gene. Proceedings of the National Academy of Sciences USA 88: large quantities of alcohol show evidence of differences 4205–4209, 1991. in brain serotonin levels compared with nonalcoholics. LYNESS, W.H., AND SMITH F.L. Influence of dopaminergic and sero- Both short- and long-term alcohol exposure also affect tonergic neurons on intravenous ethanol self-administration in the rat. the serotonin receptors that convert the chemical sig- Pharmacology and Biochemistry of Behavior 42:187–192, 1992. nal produced by serotonin into functional changes in the signal-receiving cell. -

Pindolol of the Activation of Postsynaptic 5-HT1A Receptors
Potentiation by (-)Pindolol of the Activation of Postsynaptic 5-HT1A Receptors Induced by Venlafaxine Jean-Claude Béïque, Ph.D., Pierre Blier, M.D., Ph.D., Claude de Montigny, M.D., Ph.D., and Guy Debonnel, M.D. The increase of extracellular 5-HT in brain terminal regions antagonist WAY 100635 (100 g/kg, i.v.). A short-term produced by the acute administration of 5-HT reuptake treatment with VLX (20 mg/kg/day ϫ 2 days) resulted in a inhibitors (SSRI’s) is hampered by the activation of ca. 90% suppression of the firing activity of 5-HT neurons somatodendritic 5-HT1A autoreceptors in the raphe nuclei. in the dorsal raphe nucleus. This was prevented by the The present in vivo electrophysiological studies were coadministration of (-)pindolol (15 mg/kg/day ϫ 2 days). undertaken, in the rat, to assess the effects of the Taken together, these results indicate that (-)pindolol coadministration of venlafaxine, a dual 5-HT/NE reuptake potentiated the activation of postsynaptic 5-HT1A receptors inhibitor, and (-)pindolol on pre- and postsynaptic 5-HT1A resulting from 5-HT reuptake inhibition probably by receptor function. The acute administration of venlafaxine blocking the somatodendritic 5-HT1A autoreceptor, but not and of the SSRI paroxetine (5 mg/kg, i.v.) induced a its postsynaptic congener. These results support and extend suppression of the firing activity of dorsal hippocampus CA3 previous findings providing a biological substratum for the pyramidal neurons. This effect of venlafaxine was markedly efficacy of pindolol as an accelerating strategy in major potentiated by a pretreatment with (-)pindolol (15 mg/kg, depression. -

Homology Models of Melatonin Receptors: Challenges and Recent Advances
Int. J. Mol. Sci. 2013, 14, 8093-8121; doi:10.3390/ijms14048093 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review Homology Models of Melatonin Receptors: Challenges and Recent Advances Daniele Pala 1, Alessio Lodola 1, Annalida Bedini 2, Gilberto Spadoni 2 and Silvia Rivara 1,* 1 Dipartimento di Farmacia, Università degli Studi di Parma, Parco Area delle Scienze 27/A, 43124 Parma, Italy; E-Mails: [email protected] (D.P.); [email protected] (A.L.) 2 Dipartimento di Scienze Biomolecolari, Università degli Studi di Urbino “Carlo Bo”, Piazza Rinascimento 6, I-61029 Urbino, Italy; E-Mails: [email protected] (A.B.); [email protected] (G.S.) * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +39-0521-905-061; Fax: +39-0521-905-006. Received: 7 March 2013; in revised form: 28 March 2013 / Accepted: 28 March 2013 / Published: 12 April 2013 Abstract: Melatonin exerts many of its actions through the activation of two G protein-coupled receptors (GPCRs), named MT1 and MT2. So far, a number of different MT1 and MT2 receptor homology models, built either from the prototypic structure of rhodopsin or from recently solved X-ray structures of druggable GPCRs, have been proposed. These receptor models differ in the binding modes hypothesized for melatonin and melatonergic ligands, with distinct patterns of ligand-receptor interactions and putative bioactive conformations of ligands. The receptor models will be described, and they will be discussed in light of the available information from mutagenesis experiments and ligand-based pharmacophore models. -

The Serotonergic System in Migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone
J Headache Pain (2001) 2:S43–S46 © Springer-Verlag 2001 MIGRAINE AND PATHOPHYSIOLOGY Massimo Leone The serotonergic system in migraine Andrea Rigamonti Domenico D’Amico Licia Grazzi Susanna Usai Gennaro Bussone Abstract Serotonin (5-HT) and induce migraine attacks. Moreover serotonin receptors play an impor- different pharmacological preventive tant role in migraine pathophysiolo- therapies (pizotifen, cyproheptadine gy. Changes in platelet 5-HT content and methysergide) are antagonist of are not casually related, but they the same receptor class. On the other may reflect similar changes at a neu- side the activation of 5-HT1B-1D ronal level. Seven different classes receptors (triptans and ergotamines) of serotoninergic receptors are induce a vasocostriction, a block of known, nevertheless only 5-HT2B-2C neurogenic inflammation and pain M. Leone • A. Rigamonti • D. D’Amico and 5HT1B-1D are related to migraine transmission. L. Grazzi • S. Usai • G. Bussone (౧) syndrome. Pharmacological evi- C. Besta National Neurological Institute, Via Celoria 11, I-20133 Milan, Italy dences suggest that migraine is due Key words Serotonin • Migraine • e-mail: [email protected] to an hypersensitivity of 5-HT2B-2C Triptans • m-Chlorophenylpiperazine • Tel.: +39-02-2394264 receptors. m-Chlorophenylpiperazine Pathogenesis Fax: +39-02-70638067 (mCPP), a 5-HT2B-2C agonist, may The 5-HT receptor family is distinguished from all other 5- Introduction 1 HT receptors by the absence of introns in the genes; in addi- tion all are inhibitors of adenylate cyclase [1]. Serotonin (5-HT) and serotonin receptors play an important The 5-HT1A receptor has a high selective affinity for 8- role in migraine pathophysiology. -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Does Curcumin Or Pindolol Potentiate Fluoxetine's Antidepressant Effect
Research Paper Does Curcumin or Pindolol Potentiate Fluoxetine’s Antidepressant Effect by a Pharmacokinetic or Pharmacodynamic Interaction? H. A. S. MURAD*, M. I. SULIAMAN1, H. ABDALLAH2 AND MAY ABDULSATTAR1 Department of Pharmacology, Faculty of Medicine, Rabigh, King Abdulaziz University (KAU), Jeddah-21589, Saudi Arabia (SA) and Faculty of Medicine, Ain Shams University, Cairo-11541, Egypt. 1Department of Pharmacology, Faculty of Medicine, KAU, Jeddah-21589, SA. 2Department of Natural Products, Faculty of Pharmacy, KAU, Jeddah-21589, SA and Department of Pharmacognosy, Faculty of Pharmacy, Cairo University, Cairo-11541, Egypt Murad, et al.: Potentiation of Fluoxetine by Curcumin This study was designed to study potentiation of fluoxetine’s antidepressant effect by curcumin or pindolol. Twenty eight groups of mice (n=8) were used in three sets of experiments. In the first set, 9 groups were subjected to the forced swimming test after being treated intraperitoneally with three vehicles, fluoxetine (5 and 20 mg/kg), curcumin (20 mg/kg), pindolol (32 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg). One hour after the test, serum and brain fluoxetine and norfluoxetine levels were measured in mice receiving fluoxetine (5 and 20 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg). In the second set, the test was done after pretreatment with p-chlorophenylalanine. In the third set, the locomotor activity was measured. The immobility duration was significantly decreased in fluoxetine (20 mg/kg), curcumin (20 mg/kg), curcumin+fluoxetine (5 mg/kg) and pindolol+fluoxetine (5 mg/kg) groups. These decreases were reversed with p-chlorophenylalanine. -

Serotonin and Drug-Induced Therapeutic Responses in Major Depression, Obsessive–Compulsive and Panic Disorders Pierre Blier, M.D., Ph.D
Serotonin and Drug-Induced Therapeutic Responses in Major Depression, Obsessive–Compulsive and Panic Disorders Pierre Blier, M.D., Ph.D. and Claude de Montigny, M.D., Ph.D. The therapeutic effectiveness of antidepressant drugs in major development of treatment strategies producing greater efficacy depression was discovered by pure serendipity. It took over 20 and more rapid onset of antidepressant action; that, is lithium years before the neurobiological modifications that could addition and pindolol combination, respectively. It is expected mediate the antidepressive response were put into evidence. that the better understanding recently obtained of the Indeed, whereas the immediate biochemical effects of these mechanism of action of certain antidepressant drugs in drugs had been well documented, their antidepressant action obsessive– compulsive and panic disorders will also lead to generally does not become apparent before 2 to 3 weeks of more effective treatment strategies for those disorders. treatment. The different classes of antidepressant [Neuropsychopharmacology 21:91S–98S, 1999] treatments were subsequently shown to enhance serotonin © 1999 American College of Neuropsychopharmacology. neurotransmission albeit via different pre- and postsynaptic Published by Elsevier Science Inc. mechanisms. Clinical trials based on this hypothesis led to the KEY WORDS: Antidepressant; Electroconvulsive shocks; electroconvulsive shock treatment (ECT), which was Lithium; Pindolol; Hippocampus; Orbito-frontal cortex generally given only to hospitalized patients. It took several years after the demonstration of the In the late 1950s, the therapeutic effect of certain drugs antidepressant effect of iproniazide and imipramine to in major depression was discovered by serendipity. An understand that these drugs could interfere with the ca- antidepressant response was observed in patients with tabolism of monoamines. -
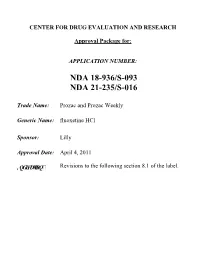
Prozac and Prozac Weekly (Fluoxetine Hcl)
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 Trade Name: Prozac and Prozac Weekly Generic Name: fluoxetine HCl Sponsor: Lilly Approval Date: April 4, 2011 ,QGLFDWLRQ Revisions to the following section 8.1 of the label. CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 CONTENTS Reviews / Information Included in this NDA Review. Approval Letter X Other Action Letters X Labeling Summary Review X Officer/Employee List Office Director Memo Cross Discipline Team Leader Review Medical Review(s) X Chemistry Review(s) Pharmacology Review(s) Statistical Review(s) Clinical Pharmacology/Biopharmaceutics Review(s) Other Reviews X Proprietary Name Review(s) Administrative/Correspondence Document(s) X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 18-936/S-093 NDA 21-235/S-016 APPROVAL LETTER DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 NDA 018936/S-091/S-093/S-095 NDA 021235/S-015/S-016/S-017 SUPPLEMENT APPROVAL Eli Lilly & Company Attention: Kevin C. Sheehan, MS, Pharm.D. Manager, Global Regulatory Affairs - US Lilly Corporate Center Indianapolis, IN 46285 Dear Dr. Sheehan: Please refer to your Supplemental New Drug Applications (sNDA) dated and received May 21, 2009 (018936/S-091 and 021235/S-015), November 6, 2009 (018936/S-093 and 021235/S-016), and April 14, 2010 (018936/S-095 and 021235/S-017), submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Prozac (fluoxetine hydrochloride) 10 mg, 20 mg, and 40 mg capsules and Prozac Weekly (fluoxetine hydrochloride) 90 mg delayed-release capsules. -

MDMA) Cause Selective Ablation of Serotonergic Axon Terminals in Forebrain: Lmmunocytochemical Evidence for Neurotoxicity
The Journal of Neuroscience, August 1988, 8(8): 2788-2803 Methylenedioxyamphetamine (MDA) and Methylenedioxymetham- phetamine (MDMA) Cause Selective Ablation of Serotonergic Axon Terminals in Forebrain: lmmunocytochemical Evidence for Neurotoxicity E. O’Hearn,” G. Battaglia, lab E. B. De Souza,’ M. J. Kuhar,’ and M. E. Molliver Departments of Neuroscience, and Neurology, The Johns Hopkins University School of Medicine, Baltimore, Maryland 21205, and ‘Neuroscience Branch, Addiction Research Center, National Institute on Drug Abuse, Baltimore, Maryland 21224 The psychotropic amphetamine derivatives 3,4-methylene- The synthetic amphetamine derivatives 3,4-methylenedioxy- dioxyamphetamine (MDA) and 3,4-methylenedioxymetham- amphetamine (MDA) and 3,4-methylenedioxymethamphet- phetamine (MDMA) have been used for recreational and amine (MDMA) are potent mood-altering drugs that have at- therapeutic purposes in man. In rats, these drugs cause large tained public interest (Seymour, 1986) due to their widespread, reductions in brain levels of serotonin (5HT). This study self-administration by young adults (e.g., Klein, 1985). These employs immunocytochemistry to characterize the neuro- drugs have also been proposed for medical use in psychotherapy toxic effects of these compounds upon monoaminergic neu- because they produce augmentation of mood and enhanced in- rons in the rat brain. Two weeks after systemic administra- sight (Naranjo et al., 1967; Yensen et al., 1976; Di Leo, 198 1; tion of MDA or MDMA (20 mg/kg, s.c., twice daily for 4 d), Greer and Tolbert, 1986; Grinspoon and Bakalar, 1986). How- there is profound loss of serotonergic (5HT) axons through- ever, concern has been raised about the safety of these com- out the forebrain; catecholamine axons are completely pounds based on evidence that they may be toxic to brain seroto- spared. -

Management of Major Depressive Disorder Clinical Practice Guidelines May 2014
Federal Bureau of Prisons Management of Major Depressive Disorder Clinical Practice Guidelines May 2014 Table of Contents 1. Purpose ............................................................................................................................................. 1 2. Introduction ...................................................................................................................................... 1 Natural History ................................................................................................................................. 2 Special Considerations ...................................................................................................................... 2 3. Screening ........................................................................................................................................... 3 Screening Questions .......................................................................................................................... 3 Further Screening Methods................................................................................................................ 4 4. Diagnosis ........................................................................................................................................... 4 Depression: Three Levels of Severity ............................................................................................... 4 Clinical Interview and Documentation of Risk Assessment...............................................................