Effects of High-Fat Diet Induced Obesity and Fructooligosaccharide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Mutations and Mechanisms in Dilated Cardiomyopathy
Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, … , Jessica R. Golbus, Megan J. Puckelwartz J Clin Invest. 2013;123(1):19-26. https://doi.org/10.1172/JCI62862. Review Series Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of congestive heart failure. In hypertrophic cardiomyopathy (HCM), cardiac output is limited by the thickened myocardium through impaired filling and outflow. Mutations in the genes encoding the thick filament components myosin heavy chain and myosin binding protein C (MYH7 and MYBPC3) together explain 75% of inherited HCMs, leading to the observation that HCM is a disease of the sarcomere. Many mutations are “private” or rare variants, often unique to families. In contrast, dilated cardiomyopathy (DCM) is far more genetically heterogeneous, with mutations in genes encoding cytoskeletal, nucleoskeletal, mitochondrial, and calcium-handling proteins. DCM is characterized by enlarged ventricular dimensions and impaired systolic and diastolic function. Private mutations account for most DCMs, with few hotspots or recurring mutations. More than 50 single genes are linked to inherited DCM, including many genes that also link to HCM. Relatively few clinical clues guide the diagnosis of inherited DCM, but emerging evidence supports the use of genetic testing to identify those patients at risk for faster disease progression, congestive heart failure, and arrhythmia. Find the latest version: https://jci.me/62862/pdf Review series Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, Jessica R. Golbus, and Megan J. Puckelwartz Department of Human Genetics, University of Chicago, Chicago, Illinois, USA. Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of conges- tive heart failure. -

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -

Unequal Allelic Expression of Wild-Type and Mutated B-Myosin in Familial Hypertrophic Cardiomyopathy
Basic Res Cardiol (2011) 106:1041–1055 DOI 10.1007/s00395-011-0205-9 ORIGINAL CONTRIBUTION Unequal allelic expression of wild-type and mutated b-myosin in familial hypertrophic cardiomyopathy Snigdha Tripathi • Imke Schultz • Edgar Becker • Judith Montag • Bianca Borchert • Antonio Francino • Francisco Navarro-Lopez • Andreas Perrot • Cemil O¨ zcelik • Karl-Josef Osterziel • William J. McKenna • Bernhard Brenner • Theresia Kraft Received: 26 May 2011 / Revised: 29 June 2011 / Accepted: 7 July 2011 / Published online: 19 July 2011 Ó The Author(s) 2011. This article is published with open access at Springerlink.com Abstract Familial hypertrophic cardiomyopathy (FHC) genotyped and clinically well-characterized FHC patients is an autosomal dominant disease, which in about 30% of were analyzed. The fraction of mutated MYH7-mRNA in the patients is caused by missense mutations in one allele five patients with mutation R723G averaged to 66 and 68% of the b-myosin heavy chain (b-MHC) gene (MYH7). To of total MYH7-mRNA in soleus and myocardium, respec- address potential molecular mechanisms underlying the tively. For mutations I736T, R719W and V606M, fractions family-specific prognosis, we determined the relative of mutated MYH7-mRNA in M. soleus were 39, 57 and expression of mutant versus wild-type MYH7-mRNA. We 29%, respectively. For all mutations, unequal abundance found a hitherto unknown mutation-dependent unequal was similar at the protein level. Importantly, fractions of expression of mutant to wild-type MYH7-mRNA, which is mutated transcripts were comparable among siblings, in paralleled by similar unequal expression of b-MHC at the younger relatives and unrelated carriers of the same protein level. -
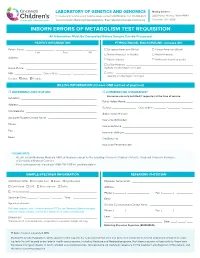
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

ACADS Rabbit Pab
Leader in Biomolecular Solutions for Life Science ACADS Rabbit pAb Catalog No.: A0945 2 Publications Basic Information Background Catalog No. This gene encodes a tetrameric mitochondrial flavoprotein, which is a member of the A0945 acyl-CoA dehydrogenase family. This enzyme catalyzes the initial step of the mitochondrial fatty acid beta-oxidation pathway. Mutations in this gene have been Observed MW associated with short-chain acyl-CoA dehydrogenase (SCAD) deficiency. Alternative 44kDa splicing results in two variants which encode different isoforms. Calculated MW 44kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 35 P16219 IHC 1:50 - 1:100 Immunogen 1:50 - 1:200 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-260 of human ACADS (NP_000008.1). Synonyms ACADS;ACAD3;SCAD Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using ACADS antibody (A0945) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 15s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunofluorescence analysis of U2OS embedded human liver cancer using embedded human liver damage using cells using ACADS antibody (A0945). Blue: ACADS antibody (A0945) at dilution of ACADS antibody (A0945) at dilution of DAPI for nuclear staining. -
PEX5 Regulates Autophagy Via the Mtorc1-TFEB Axis During Starvation
Eun et al. Experimental & Molecular Medicine (2018) 50:4 DOI 10.1038/s12276-017-0007-8 Experimental & Molecular Medicine ARTICLE Open Access PEX5 regulates autophagy via the mTORC1-TFEB axis during starvation So Young Eun1,JoonNoLee2,In-KooNam2, Zhi-qiang Liu1,Hong-SeobSo 1, Seong-Kyu Choe1 and RaeKil Park2 Abstract Defects in the PEX5 gene impair the import of peroxisomal matrix proteins, leading to nonfunctional peroxisomes and other associated pathological defects such as Zellweger syndrome. Although PEX5 regulates autophagy process in a stress condition, the mechanisms controlling autophagy by PEX5 under nutrient deprivation are largely unknown. Herein, we show a novel function of PEX5 in the regulation of autophagy via Transcription Factor EB (TFEB). Under serum-starved conditions, when PEX5 is depleted, the mammalian target of rapamycin (mTORC1) inhibitor TSC2 is downregulated, which results in increased phosphorylation of the mTORC1 substrates, including 70S6K, S6K, and 4E- BP-1. mTORC1 activation further suppresses the nuclear localization of TFEB, as indicated by decreased mRNA levels of TFEB, LIPA, and LAMP1. Interestingly, peroxisomal mRNA and protein levels are also reduced by TFEB inactivation, indicating that TFEB might control peroxisome biogenesis at a transcriptional level. Conversely, pharmacological inhibition of mTOR resulting from PEX5 depletion during nutrient starvation activates TFEB by promoting nuclear localization of the protein. In addition, mTORC1 inhibition recovers the damaged-peroxisome biogenesis. These data suggest that PEX5 may be a critical regulator of lysosomal gene expression and autophagy through the mTOR-TFEB- autophagy axis under nutrient deprivation. 1234567890():,; 1234567890():,; Introduction Mitochondrial antiviral-signaling protein (MAVS) func- Peroxisome is an essential cellular organelle for per- tions as an antiviral signaling platform to induce the forming various metabolic activities, including oxidation interferon-independent signaling pathways4. -

Positive Carrier Sample Report
RESULTS RECIPIENT FEMALE MALE UNIVERSITY MEDICAL CENTER JANE MILLER N/A Attn: Dr. Paul Smith DOB: 11/11/1977 123 Main Street Ethnicity: Northern European City, CA 10231 Sample Type: OG-510 Saliva Phone: (800) 555-1212 Date of Collection: 02/06/2020 Fax: (800) 555-1212 Date Received: 02/16/2020 NPI: 4253506008 Date Tested: 02/16/2020 Report Date: 02/18/2020 Barcode: 55200006634190 Accession ID: FAKERQSCARFAF Indication: Screening for genetic disease carrier status Foresight® Carrier Screen POSITIVE: CARRIER ABOUT THIS TEST The Myriad Foresight Carrier Screen utilizes sequencing, maximizing coverage across all DNA regions tested, to help you learn about your chance to have a child with a genetic disease. RESULTS SUMMARY Risk Details JANE MILLER Partner Panel Information Foresight Carrier Screen N/A Universal Panel Fundamental Plus Panel Fundamental Panel Fragile X Syndrome (176 conditions tested) POSITIVE: CARRIER CARRIER* The reproductive risk presented Smith‑Lemli‑Opitz Syndrome NM_001360.2(DHCR7):c. is based on a hypothetical 964-1G>C(aka IVS8-1G>C) pairing with a partner of the Reproductive Risk: 1 in 380 heterozygote same ethnic group. Carrier Inheritance: Autosomal Recessive testing should be considered. See "Next Steps". *Carriers generally do not experience symptoms. No disease-causing mutations were detected in any other gene tested. A complete list of all conditions tested can be found on page 6. Additional Findings Single Carrier Autosomal recessive additional findings CLINICAL NOTES NEXT STEPS • None • Carrier testing should be considered for the diseases specified above for the patient's partner, as both parents must be carriers before a child is at high risk of developing the disease. -

IL21R Expressing CD14+CD16+ Monocytes Expand in Multiple
Plasma Cell Disorders SUPPLEMENTARY APPENDIX IL21R expressing CD14 +CD16 + monocytes expand in multiple myeloma patients leading to increased osteoclasts Marina Bolzoni, 1 Domenica Ronchetti, 2,3 Paola Storti, 1,4 Gaetano Donofrio, 5 Valentina Marchica, 1,4 Federica Costa, 1 Luca Agnelli, 2,3 Denise Toscani, 1 Rosanna Vescovini, 1 Katia Todoerti, 6 Sabrina Bonomini, 7 Gabriella Sammarelli, 1,7 Andrea Vecchi, 8 Daniela Guasco, 1 Fabrizio Accardi, 1,7 Benedetta Dalla Palma, 1,7 Barbara Gamberi, 9 Carlo Ferrari, 8 Antonino Neri, 2,3 Franco Aversa 1,4,7 and Nicola Giuliani 1,4,7 1Myeloma Unit, Dept. of Medicine and Surgery, University of Parma; 2Dept. of Oncology and Hemato-Oncology, University of Milan; 3Hematology Unit, “Fondazione IRCCS Ca’ Granda”, Ospedale Maggiore Policlinico, Milan; 4CoreLab, University Hospital of Parma; 5Dept. of Medical-Veterinary Science, University of Parma; 6Laboratory of Pre-clinical and Translational Research, IRCCS-CROB, Referral Cancer Center of Basilicata, Rionero in Vulture; 7Hematology and BMT Center, University Hospital of Parma; 8Infectious Disease Unit, University Hospital of Parma and 9“Dip. Oncologico e Tecnologie Avanzate”, IRCCS Arcispedale Santa Maria Nuova, Reggio Emilia, Italy ©2017 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2016.153841 Received: August 5, 2016. Accepted: December 23, 2016. Pre-published: January 5, 2017. Correspondence: [email protected] SUPPLEMENTAL METHODS Immunophenotype of BM CD14+ in patients with monoclonal gammopathies. Briefly, 100 μl of total BM aspirate was incubated in the dark with anti-human HLA-DR-PE (clone L243; BD), anti-human CD14-PerCP-Cy 5.5, anti-human CD16-PE-Cy7 (clone B73.1; BD) and anti-human CD45-APC-H 7 (clone 2D1; BD) for 20 min. -

Annexin A2 Depletion Delays EGFR Endocytic Trafficking Via Cofilin
Oncogene (2014) 33, 2610–2619 & 2014 Macmillan Publishers Limited All rights reserved 0950-9232/14 www.nature.com/onc ORIGINAL ARTICLE Annexin A2 depletion delays EGFR endocytic trafficking via cofilin activation and enhances EGFR signaling and metastasis formation M de Graauw1, L Cao2,5, L Winkel3,5, MHAM van Miltenburg4,SEleDe´ve´ dec1, M Klop1,KYan2, C Pont1, V-M Rogkoti1, A Tijsma1, A Chaudhuri1, R Lalai1, L Price1, F Verbeek2 and B van de Water1 Enhanced epidermal growth factor receptor (EGFR) activity has been strongly linked to breast cancer progression and mediators of EGFR endocytosis may well be involved. We developed a semi-automated high-content fluorescence microscopy-based EGFR endocytosis screen to identify proteins that mediate EGFR endocytosis in human HBL100 breast cancer cells. Knockdown of 172 individual endocytosis and actin-regulatory genes with small interfering RNAs led to the identification of 14 genes of which the contribution to EGFR endocytosis in breast cancer is until now poorly defined, including DNAJC6, GDI2, FGD6, HAX1, NECAP2 and AnxA2. We show that depletion of the actin and endocytosis regulatory protein annexin A2 (AnxA2) in a panel of four triple negative breast cancer (TNBC) cell lines affected EGFR endocytosis. Depletion of AnxA2 in the aggressive and highly metastatic MDA-MB-231 TNBC cell line resulted in the inhibition of EGFR transport beyond the early endosomes. This inhibition coincided with enhanced epidermal growth factor (EGF)-induced cell migration and downstream signaling via c-Jun N-terminal kinase (JNK) and Akt. Moreover, AnxA2 knockdown increased lung metastasis formation in mice. The effect of AnxA2 knockdown on EGFR endocytosis in MDA-MB-231 was related to dephosphorylation/activation of the actin-severing protein cofilin, as re-expression of an inactive S3E- cofilin mutant, but not an active S3A-cofilin mutant, re-established EGFR endocytosis to control levels. -

2812 Matrix Vesicles: Structure, Composition, Formation and Function in Ca
[Frontiers in Bioscience 16, 2812-2902, June 1, 2011] Matrix vesicles: structure, composition, formation and function in calcification Roy E. Wuthier Department of Chemistry and Biochemistry, University of South Carolina, Columbia, SC 29208 TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Morphology of matrix vesicles (MVs) 3.1. Conventional transmission electron microscopy 3.2. Cryofixation, freeze-substitution electron microscopy 3.3. Freeze-fracture studies 4. Isolation of MVs 4.1. Crude collagenase digestion methods 4.2. Non-collagenase dependent methods 4.3. Cell culture methods 4.4. Modified collagenase digestion methods 4.5. Other isolation methods 5. MV proteins 5.1. Early SDS-PAGE studies 5.2. Isolation and identification of major MV proteins 5.3. Sequential extraction, separation and characterization of major MV proteins 5.4. Proteomic characterization of MV proteins 6. MV-associated extracellular matrix proteins 6.1. Type VI collagen 6.2. Type X collagen 6.3. Proteoglycan link protein and aggrecan core protein 6.4. Fibrillin-1 and fibrillin-2 7. MV annexins – acidic phospholipid-dependent ca2+-binding proteins 7.1. Annexin A5 7.2. Annexin A6 7.3. Annexin A2 7.4. Annexin A1 7.5. Annexin A11 and Annexin A4 8. MV enzymes 8.1. Tissue-nonspecific alkaline phosphatase(TNAP) 8.1.1. Molecular structure 8.1.2. Amino acid sequence 8.1.3. 3-D structure 8.1.4. Disposition in the MV membrane 8.1.5. Catalytic properties 8.1.6. Collagen-binding properties 8.2. Nucleotide pyrophosphate phosphodiesterase (NPP1, PC1) 8.3. PHOSPHO-1 (Phosphoethanolamine/Phosphocholine phosphatase 8.4. Acid phosphatase 8.5. -
Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity
International Journal of Molecular Sciences Review Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity Yannick Das, Daniëlle Swinkels and Myriam Baes * Lab of Cell Metabolism, Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, 3000 Leuven, Belgium; [email protected] (Y.D.); [email protected] (D.S.) * Correspondence: [email protected] Abstract: Peroxisomes are multifunctional organelles, well known for their role in cellular lipid homeostasis. Their importance is highlighted by the life-threatening diseases caused by peroxisomal dysfunction. Importantly, most patients suffering from peroxisomal biogenesis disorders, even those with a milder disease course, present with a number of ocular symptoms, including retinopathy. Patients with a selective defect in either peroxisomal α- or β-oxidation or ether lipid synthesis also suffer from vision problems. In this review, we thoroughly discuss the ophthalmological pathology in peroxisomal disorder patients and, where possible, the corresponding animal models, with a special emphasis on the retina. In addition, we attempt to link the observed retinal phenotype to the underlying biochemical alterations. It appears that the retinal pathology is highly variable and the lack of histopathological descriptions in patients hampers the translation of the findings in the mouse models. Furthermore, it becomes clear that there are still large gaps in the current knowledge on the contribution of the different metabolic disturbances to the retinopathy, but branched chain fatty acid accumulation and impaired retinal PUFA homeostasis are likely important factors. Citation: Das, Y.; Swinkels, D.; Baes, Keywords: peroxisome; Zellweger; metabolism; fatty acid; retina M. Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity.