NMR-Based Newborn Urine Screening for Optimized Detection of Inherited
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperammonemia in Review: Pathophysiology, Diagnosis, and Treatment
Pediatr Nephrol DOI 10.1007/s00467-011-1838-5 EDUCATIONAL REVIEW Hyperammonemia in review: pathophysiology, diagnosis, and treatment Ari Auron & Patrick D. Brophy Received: 23 September 2010 /Revised: 9 January 2011 /Accepted: 12 January 2011 # IPNA 2011 Abstract Ammonia is an important source of nitrogen and is the breakdown and catabolism of dietary and bodily proteins, required for amino acid synthesis. It is also necessary for respectively. In healthy individuals, amino acids that are not normal acid-base balance. When present in high concentra- needed for protein synthesis are metabolized in various tions, ammonia is toxic. Endogenous ammonia intoxication chemical pathways, with the rest of the nitrogen waste being can occur when there is impaired capacity of the body to converted to urea. Ammonia is important for normal animal excrete nitrogenous waste, as seen with congenital enzymatic acid-base balance. During exercise, ammonia is produced in deficiencies. A variety of environmental causes and medica- skeletal muscle from deamination of adenosine monophos- tions may also lead to ammonia toxicity. Hyperammonemia phate and amino acid catabolism. In the brain, the latter refers to a clinical condition associated with elevated processes plus the activity of glutamate dehydrogenase ammonia levels manifested by a variety of symptoms and mediate ammonia production. After formation of ammonium signs, including significant central nervous system (CNS) from glutamine, α-ketoglutarate, a byproduct, may be abnormalities. Appropriate and timely management requires a degraded to produce two molecules of bicarbonate, which solid understanding of the fundamental pathophysiology, are then available to buffer acids produced by dietary sources. differential diagnosis, and treatment approaches available. -

Inherited Metabolic Disease
Inherited metabolic disease Dr Neil W Hopper SRH Areas for discussion • Introduction to IEMs • Presentation • Initial treatment and investigation of IEMs • Hypoglycaemia • Hyperammonaemia • Other presentations • Management of intercurrent illness • Chronic management Inherited Metabolic Diseases • Result from a block to an essential pathway in the body's metabolism. • Huge number of conditions • All rare – very rare (except for one – 1:500) • Presentation can be non-specific so index of suspicion important • Mostly AR inheritance – ask about consanguinity Incidence (W. Midlands) • Amino acid disorders (excluding phenylketonuria) — 18.7 per 100,000 • Phenylketonuria — 8.1 per 100,000 • Organic acidemias — 12.6 per 100,000 • Urea cycle diseases — 4.5 per 100,000 • Glycogen storage diseases — 6.8 per 100,000 • Lysosomal storage diseases — 19.3 per 100,000 • Peroxisomal disorders — 7.4 per 100,000 • Mitochondrial diseases — 20.3 per 100,000 Pathophysiological classification • Disorders that result in toxic accumulation – Disorders of protein metabolism (eg, amino acidopathies, organic acidopathies, urea cycle defects) – Disorders of carbohydrate intolerance – Lysosomal storage disorders • Disorders of energy production, utilization – Fatty acid oxidation defects – Disorders of carbohydrate utilization, production (ie, glycogen storage disorders, disorders of gluconeogenesis and glycogenolysis) – Mitochondrial disorders – Peroxisomal disorders IMD presentations • ? IMD presentations • Screening – MCAD, PKU • Progressive unexplained neonatal -

Summary Current Practices Report
18/10/2011 EU Tender “Evaluation of population newborn screening practices for rare disorders in Member States of the European Union” Short Executive Summary of the Report on the practices of newborn screening for rare disorders implemented in Member States of the European Union, Candidate, Potential Candidate and EFTA Countries Authors: Peter Burgard1, Martina Cornel2, Francesco Di Filippo4, Gisela Haege1, Georg F. Hoffmann1, Martin Lindner1, J. Gerard Loeber3, Tessel Rigter2, Kathrin Rupp1, 4 Domenica Taruscio4,Luciano Vittozzi , Stephanie Weinreich2 1 Department of Pediatrics , University Hospital - Heidelberg (DE) 2 VU University Medical Centre - Amsterdam (NL) 3 RIVM - Bilthoven (NL) 4 National Centre for Rare Diseases - Rome (IT) The opinions expressed in this document are those of the Contractor only and do not represent the official position of the Executive Agency for Health and Consumers. This work is funded by the European Union with a grant of Euro 399755 (Contract number 2009 62 06 of the Executive Agency for Health and Consumers) 1 18/10/2011 Abbreviations 3hmg 3-Hydroxy-3-methylglutaric aciduria 3mcc 3-Methylcrotonyl-CoA carboxylase deficiency/3-Methylglutacon aciduria/2-methyl-3-OH- butyric aciduria AAD Disorders of amino acid metabolism arg Argininemia asa Argininosuccinic aciduria bio Biotinidase deficiency bkt Beta-ketothiolase deficiency btha S, beta 0-thalassemia cah Congenital adrenal hyperplasia cf Cystic fibrosis ch Primary congenital hypothyroidism citI Citrullinemia type I citII Citrullinemia type II cpt I Carnitin -

Argininosuccinate Lyase Deficiency
©American College of Medical Genetics and Genomics GENETEST REVIEW Argininosuccinate lyase deficiency Sandesh C.S. Nagamani, MD1, Ayelet Erez, MD, PhD1 and Brendan Lee, MD, PhD1,2 The urea cycle consists of six consecutive enzymatic reactions that citrulline together with elevated argininosuccinic acid in the plasma convert waste nitrogen into urea. Deficiencies of any of these enzymes or urine. Molecular genetic testing of ASL and assay of ASL enzyme of the cycle result in urea cycle disorders (UCDs), a group of inborn activity are helpful when the biochemical findings are equivocal. errors of hepatic metabolism that often result in life-threatening However, there is no correlation between the genotype or enzyme hyperammonemia. Argininosuccinate lyase (ASL) catalyzes the activity and clinical outcome. Treatment of acute metabolic decom- fourth reaction in this cycle, resulting in the breakdown of arginino- pensations with hyperammonemia involves discontinuing oral pro- succinic acid to arginine and fumarate. ASL deficiency (ASLD) is the tein intake, supplementing oral intake with intravenous lipids and/ second most common UCD, with a prevalence of ~1 in 70,000 live or glucose, and use of intravenous arginine and nitrogen-scavenging births. ASLD can manifest as either a severe neonatal-onset form therapy. Dietary restriction of protein and dietary supplementation with hyperammonemia within the first few days after birth or as a with arginine are the mainstays in long-term management. Ortho- late-onset form with episodic hyperammonemia and/or long-term topic liver transplantation (OLT) is best considered only in patients complications that include liver dysfunction, neurocognitive deficits, with recurrent hyperammonemia or metabolic decompensations and hypertension. -

What Disorders Are Screened for by the Newborn Screen?
What disorders are screened for by the newborn screen? Endocrine Disorders The endocrine system is important to regulate the hormones in our bodies. Hormones are special signals sent to various parts of the body. They control many things such as growth and development. The goal of newborn screening is to identify these babies early so that treatment can be started to keep them healthy. To learn more about these specific disorders please click on the name of the disorder below: English: Congenital Adrenal Hyperplasia Esapnol Hiperplasia Suprarrenal Congenital - - http://www.newbornscreening.info/Parents/otherdisorders/CAH.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/CAH.html - Congenital Hypothyroidism (Hipotiroidismo Congénito) - http://www.newbornscreening.info/Parents/otherdisorders/CH.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/CH.html Hematologic Conditions Hemoglobin is a special part of our red blood cells. It is important for carrying oxygen to the parts of the body where it is needed. When people have problems with their hemoglobin they can have intense pain, and they often get sick more than other children. Over time, the lack of oxygen to the body can cause damage to the organs. The goal of newborn screening is to identify babies with these conditions so that they can get early treatment to help keep them healthy. To learn more about these specific disorders click here (XXX). - Sickle Cell Anemia (Anemia de Célula Falciforme) - http://www.newbornscreening.info/Parents/otherdisorders/SCD.html - http://www.newbornscreening.info/spanish/parent/Other_disorder/SCD.html - SC Disease (See Previous Link) - Sickle Beta Thalassemia (See Previous Link) Enzyme Deficiencies Enzymes are special proteins in our body that allow for chemical reactions to take place. -

A Curated Gene List for Reporting Results of Newborn Genomic Sequencing
© American College of Medical Genetics and Genomics ORIGINAL RESEARCH ARTICLE A curated gene list for reporting results of newborn genomic sequencing Ozge Ceyhan-Birsoy, PhD1,2,3, Kalotina Machini, PhD1,2,3, Matthew S. Lebo, PhD1,2,3, Tim W. Yu, MD3,4,5, Pankaj B. Agrawal, MD, MMSC3,4,6, Richard B. Parad, MD, MPH3,7, Ingrid A. Holm, MD, MPH3,4, Amy McGuire, PhD8, Robert C. Green, MD, MPH3,9,10, Alan H. Beggs, PhD3,4, Heidi L. Rehm, PhD1,2,3,10; for the BabySeq Project Purpose: Genomic sequencing (GS) for newborns may enable detec- of newborn GS (nGS), and used our curated list for the first 15 new- tion of conditions for which early knowledge can improve health out- borns sequenced in this project. comes. One of the major challenges hindering its broader application Results: Here, we present our curated list for 1,514 gene–disease is the time it takes to assess the clinical relevance of detected variants associations. Overall, 954 genes met our criteria for return in nGS. and the genes they impact so that disease risk is reported appropri- This reference list eliminated manual assessment for 41% of rare vari- ately. ants identified in 15 newborns. Methods: To facilitate rapid interpretation of GS results in new- Conclusion: Our list provides a resource that can assist in guiding borns, we curated a catalog of genes with putative pediatric relevance the interpretive scope of clinical GS for newborns and potentially for their validity based on the ClinGen clinical validity classification other populations. framework criteria, age of onset, penetrance, and mode of inheri- tance through systematic evaluation of published evidence. -

JB Review Featured Article
J. Biochem. 2011;150(3):257–266 doi:10.1093/jb/mvr090 JB Review The scent of disease: volatile organic compounds of the human body related to disease and disorder Received May 27, 2011; accepted July 6, 2011; published online July 19, 2011 Mika Shirasu and Kazushige Touhara* Human body odours also have this function; we emit a wide array of volatile organic compounds (VOCs), Department of Applied Biological Chemistry, Graduate School of both odorous and non-odorous, from our bodies. The Agricultural and Life Sciences, The University of Tokyo, Tokyo113-8657, Japan VOCs emitted from different areas of the human body vary with age, diet, sex, physiological status and pos- *Kazushige Touhara, Department of Applied Biological Chemistry, sibly genetic background. Therefore, body odours can The University of Tokyo, 1-1-1 Yayoi, Bunkyo-ku, Tokyo, Japan 113-8657. Tel: þ03 5841 5109, Fax: þ03 5841 8024, be considered as individual ‘odour-fingerprints’. email: [email protected] Pathological processes, such as infection and en- dogenous metabolic disorders, can influence our daily Hundreds of volatile organic compounds (VOCs) are odour fingerprints by producing new VOCs or by emitted from the human body, and the components of changing the ratio of VOCs that are produced nor- VOCs usually reflect the metabolic condition of an in- mally. Therefore, it is not surprising that physicians Downloaded from dividual. Therefore, contracting an infectious or meta- have used their olfactory senses to diagnose physical bolic disease often results in a change in body odour. conditions of patients. Around 400 BD, Hippocrates Recent progresses in analytical techniques allow rapid recognized the diagnostic usefulness of body odours analyses of VOCs derived from breath, blood, skin and and reported on several disease-specific odours ema- urine. -

Annual Symposium of the Society for the Study of Inborn Errors of Metabolism Birmingham, UK, 4 – 7 September 2012
J Inherit Metab Dis (2012) 35 (Suppl 1):S1–S182 DOI 10.1007/s10545-012-9512-z ABSTRACTS Annual Symposium of the Society for the Study of Inborn Errors of Metabolism Birmingham, UK, 4 – 7 September 2012 This supplement was not sponsored by outside commercial interests. It was funded entirely by the SSIEM. 01. Amino Acids and PKU O-002 NATURAL INHIBITORS OF CARNOSINASE (CN1) O-001 Peters V1 ,AdelmannK2 ,YardB2 , Klingbeil K1 ,SchmittCP1 , Zschocke J3 3-HYDROXYISOBUTYRIC ACID DEHYDROGENASE DEFICIENCY: 1Zentrum für Kinder- und Jugendmedizin de, Heidelberg, Germany IDENTIFICATION OF A NEW INBORN ERROR OF VALINE 2Universitätsklinik, Mannheim, Germany METABOLISM 3Humangenetik, Innsbruck, Austria Wanders RJA1 , Ruiter JPN1 , Loupatty F.1 , Ferdinandusse S.1 , Waterham HR1 , Pasquini E.1 Background: Carnosinase degrades histidine-containing dipeptides 1Div Metab Dis, Univ Child Hosp, Amsterdam, Netherlands such as carnosine and anserine which are known to have several protective functions, especially as antioxidant agents. We recently Background, Objectives: Until now only few patients with an established showed that low carnosinase activities protect from diabetic nephrop- defect in the valine degradation pathway have been identified. Known athy, probably due to higher histidine-dipeptide concentrations. We deficiencies include 3-hydroxyisobutyryl-CoA hydrolase deficiency and now characterized the carnosinase metabolism in children and identi- methylmalonic semialdehyde dehydrogenase (MMSADH) deficiency. On fied natural inhibitors of carnosinase. the other hand many patients with 3-hydroxyisobutyric aciduria have been Results: Whereas serum carnosinase activity and protein concentrations described with a presumed defect in the valine degradation pathway. To correlate in adults, children have lower carnosinase activity although pro- identify the enzymatic and molecular defect in a group of patients with 3- tein concentrations were within the same level as for adults. -

Ex Vivo Gene Therapy: a “Cultured” Surgical Approach to Curing Inherited Liver Disease
Mini Review Open Access J Surg Volume 10 Issue 3 - March 2019 Copyright © All rights are reserved by Joseph B Lillegard DOI: 10.19080/OAJS.2019.10.555788 Ex Vivo Gene Therapy: A “Cultured” Surgical Approach to Curing Inherited Liver Disease Caitlin J VanLith1, Robert A Kaiser1,2, Clara T Nicolas1 and Joseph B Lillegard1,2,3* 1Department of Surgery, Mayo Clinic, Rochester, MN, USA 2Midwest Fetal Care Center, Children’s Hospital of Minnesota, Minneapolis, MN, USA 3Pediatric Surgical Associates, Minneapolis, MN, USA Received: February 22, 2019; Published: March 21, 2019 *Corresponding author: Joseph B Lillegard, Midwest Fetal Care Center, Children’s Hospital of Minnesota, Minneapolis, Minnesota, USA and Mayo Clinic, Rochester, Minnesota, USA Introduction Inborn errors of metabolism (IEMs) are a group of inherited diseases caused by mutations in a single gene [1], many of which transplant remains the only curative option. Between 1988 and 2018, 12.8% of 17,009 pediatric liver transplants in the United States(see were primarily due to an inherited liver). disease. are identified in Table 1. Though individually rare, combined incidence is about 1 in 1,000 live births [2]. While maintenance www.optn.transplant.hrsa.gov/data/ Table 1: List of 35 of the most common Inborn Errors of Metabolism. therapies exist for some of these liver-related diseases, Inborn Error of Metabolism Abbreviation Hereditary Tyrosinemia type 1 HT1 Wilson Disease Wilson Glycogen Storage Disease 1 GSD1 Carnitine Palmitoyl Transferase Deficiency Type 2 CPT2 Glycogen Storage -

(12) Patent Application Publication (10) Pub. No.: US 2006/0134109 A1 Gaitanaris Et Al
US 2006O134109A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0134109 A1 Gaitanaris et al. (43) Pub. Date: Jun. 22, 2006 (54) GPROTEIN COUPLED RECEPTORS AND in-part of application No. 60/461.329, filed on Apr. 9. USES THEREOF 2003. (75) Inventors: George A. Gaitanaris, Seattle, WA Publication Classification (US); John E. Bergmann, Mercer Island, WA (US); Alexander Gragerov, (51) Int. Cl. Seattle, WA (US); John Hohmann, La CI2O I/68 (2006.01) Conner, WA (US); Fusheng Li, Seattle, C7H 2L/04 (2006.01) WA (US); Linda Madisen, Seattle, WA (US); Kellie L. McIlwain, Renton, WA CI2P 2/06 (2006.01) (US); Maria N. Pavlova, Seattle, WA A 6LX 39/395 (2006.01) (US); Demitri Vassilatis, Seattle, WA C07K I4/705 (2006.01) (US); Hongkui Zeng, Shoreline, WA (52) U.S. Cl. ......................... 424/143.1: 435/6: 435/69.1; 435/320.1; 435/325; 530/350; (US) 536/23.5 Correspondence Address: SEED INTELLECTUAL PROPERTY LAW GROUP PLLC (57) ABSTRACT 701 FIFTHAVE SUTE 63OO The present invention provides GPCR polypeptides and SEATTLE, WA 98104-7092 (US) polynucleotides, recombinant materials, and transgenic (73) Assignee: Nura Inc., Seattle, WA (US) mice, as well as methods for their production. The polypep tides and polynucleotides are useful, for example, in meth (21) Appl. No.: 10/527,265 ods of diagnosis and treatment of diseases and disorders. The invention also provides methods for identifying com (22) PCT Fed: Sep. 9, 2003 pounds (e.g., agonists or antagonists) using the GPCR polypeptides and polynucleotides of the invention, and for (86) PCT No.: PCT/USO3/28226 treating conditions associated with GPCR dysfunction with the GPCR polypeptides, polynucleotides, or identified com Related U.S. -
Test Requisition Form (Dna & Genetic Tests)
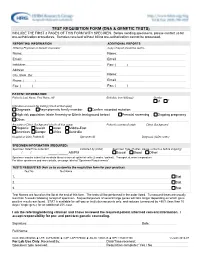
TEST REQUISITION FORM (DNA & GENETIC TESTS) INCLUDE THE FIRST 3 PAGES OF THIS FORM WITH SPECIMEN. Before sending specimens, please contact us for pre-authorization procedures. Samples received without billing pre-authorization cannot be processed. REPORTING INFORMATION ADDITIONAL REPORTS Ordering Physician or Genetic Counselor Copy of report should be sent to Name: Name: Email: Email: Institution: Fax: ( ) Address: City, State, Zip: Name: Phone: ( ) Email: Fax: ( ) Fax: ( ) PATIENT INFORMATION Patient's Last Name, First Name, MI Birthdate (mm/dd/yyyy) Gender M F Indication or reason for testing (check all that apply) Diagnosis Asymptomatic family member Confirm recorded mutation: High risk population (state Ancestry or Ethnic background below) Prenatal screening Ongoing pregnancy Other: Ancestry or Ethnic Background (check all that apply) Patient's country of origin Ethnic Background Hispanic Jewish Asian Middle-East Americas Europe Africa Australia Hospital or Clinic Patient ID Specimen ID Diagnosis (ICD9 codes) SPECIMEN INFORMATION (REQUIRED) Specimen Date/Time Collected Collected by (initial) Specimen Type (If other, please contact us before shipping) / / _____:_____ AM/PM Buccal Blood Other: Specimen may be submitted as whole blood or buccal epithelial cells (2 swabs / patient). Transport at room temperature. For other specimens and more details, see page labeled "Specimen Requirements". TESTS REQUESTED (Ask us to customize the requisition form for your practice) Test No. Test Name 1. Stat 2. Stat 3. Stat Test Names are found on the list at the end of this form. The tests will be performed in the order listed. Turnaround times are usually less than 5 weeks following receipt of specimen. Sequential panels of several large genes will take longer depending on which gene positive results are found. -

Enteral Nutrition
UnitedHealthcare® Commercial Coverage Determination Guideline Enteral Nutrition Guideline Number: CDG.027.03 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ........................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Definitions ........................................................................................... 2 Supplies and Repairs/ Replacements Applicable Codes .............................................................................. 3 References .......................................................................................10 Community Plan Policy Guideline History/Revision Information .......................................10 • Oral and Enteral Nutrition Instructions for Use .........................................................................10 Coverage Rationale Indications for Coverage Certain plans may include coverage for enteral nutrition (enteral formulas and low protein modified food products). Refer to the member specific benefit plan document to determine if this coverage applies. For Plans with Language that Cover Enteral Nutrition For plans that cover enteral nutrition, if there is a difference between a member specific benefit plan document and the information below, the member specific benefit plan document should be used for making benefit determinations. Note: Check state mandate applicability before proceeding with the following. Benefits are provided