Enteral Nutrition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inherited Metabolic Disease
Inherited metabolic disease Dr Neil W Hopper SRH Areas for discussion • Introduction to IEMs • Presentation • Initial treatment and investigation of IEMs • Hypoglycaemia • Hyperammonaemia • Other presentations • Management of intercurrent illness • Chronic management Inherited Metabolic Diseases • Result from a block to an essential pathway in the body's metabolism. • Huge number of conditions • All rare – very rare (except for one – 1:500) • Presentation can be non-specific so index of suspicion important • Mostly AR inheritance – ask about consanguinity Incidence (W. Midlands) • Amino acid disorders (excluding phenylketonuria) — 18.7 per 100,000 • Phenylketonuria — 8.1 per 100,000 • Organic acidemias — 12.6 per 100,000 • Urea cycle diseases — 4.5 per 100,000 • Glycogen storage diseases — 6.8 per 100,000 • Lysosomal storage diseases — 19.3 per 100,000 • Peroxisomal disorders — 7.4 per 100,000 • Mitochondrial diseases — 20.3 per 100,000 Pathophysiological classification • Disorders that result in toxic accumulation – Disorders of protein metabolism (eg, amino acidopathies, organic acidopathies, urea cycle defects) – Disorders of carbohydrate intolerance – Lysosomal storage disorders • Disorders of energy production, utilization – Fatty acid oxidation defects – Disorders of carbohydrate utilization, production (ie, glycogen storage disorders, disorders of gluconeogenesis and glycogenolysis) – Mitochondrial disorders – Peroxisomal disorders IMD presentations • ? IMD presentations • Screening – MCAD, PKU • Progressive unexplained neonatal -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -

Amino Acid Disorders
471 Review Article on Inborn Errors of Metabolism Page 1 of 10 Amino acid disorders Ermal Aliu1, Shibani Kanungo2, Georgianne L. Arnold1 1Children’s Hospital of Pittsburgh, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA; 2Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, MI, USA Contributions: (I) Conception and design: S Kanungo, GL Arnold; (II) Administrative support: S Kanungo; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: E Aliu, GL Arnold; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Georgianne L. Arnold, MD. UPMC Children’s Hospital of Pittsburgh, 4401 Penn Avenue, Suite 1200, Pittsburgh, PA 15224, USA. Email: [email protected]. Abstract: Amino acids serve as key building blocks and as an energy source for cell repair, survival, regeneration and growth. Each amino acid has an amino group, a carboxylic acid, and a unique carbon structure. Human utilize 21 different amino acids; most of these can be synthesized endogenously, but 9 are “essential” in that they must be ingested in the diet. In addition to their role as building blocks of protein, amino acids are key energy source (ketogenic, glucogenic or both), are building blocks of Kreb’s (aka TCA) cycle intermediates and other metabolites, and recycled as needed. A metabolic defect in the metabolism of tyrosine (homogentisic acid oxidase deficiency) historically defined Archibald Garrod as key architect in linking biochemistry, genetics and medicine and creation of the term ‘Inborn Error of Metabolism’ (IEM). The key concept of a single gene defect leading to a single enzyme dysfunction, leading to “intoxication” with a precursor in the metabolic pathway was vital to linking genetics and metabolic disorders and developing screening and treatment approaches as described in other chapters in this issue. -

A Curated Gene List for Reporting Results of Newborn Genomic Sequencing
© American College of Medical Genetics and Genomics ORIGINAL RESEARCH ARTICLE A curated gene list for reporting results of newborn genomic sequencing Ozge Ceyhan-Birsoy, PhD1,2,3, Kalotina Machini, PhD1,2,3, Matthew S. Lebo, PhD1,2,3, Tim W. Yu, MD3,4,5, Pankaj B. Agrawal, MD, MMSC3,4,6, Richard B. Parad, MD, MPH3,7, Ingrid A. Holm, MD, MPH3,4, Amy McGuire, PhD8, Robert C. Green, MD, MPH3,9,10, Alan H. Beggs, PhD3,4, Heidi L. Rehm, PhD1,2,3,10; for the BabySeq Project Purpose: Genomic sequencing (GS) for newborns may enable detec- of newborn GS (nGS), and used our curated list for the first 15 new- tion of conditions for which early knowledge can improve health out- borns sequenced in this project. comes. One of the major challenges hindering its broader application Results: Here, we present our curated list for 1,514 gene–disease is the time it takes to assess the clinical relevance of detected variants associations. Overall, 954 genes met our criteria for return in nGS. and the genes they impact so that disease risk is reported appropri- This reference list eliminated manual assessment for 41% of rare vari- ately. ants identified in 15 newborns. Methods: To facilitate rapid interpretation of GS results in new- Conclusion: Our list provides a resource that can assist in guiding borns, we curated a catalog of genes with putative pediatric relevance the interpretive scope of clinical GS for newborns and potentially for their validity based on the ClinGen clinical validity classification other populations. framework criteria, age of onset, penetrance, and mode of inheri- tance through systematic evaluation of published evidence. -

JB Review Featured Article
J. Biochem. 2011;150(3):257–266 doi:10.1093/jb/mvr090 JB Review The scent of disease: volatile organic compounds of the human body related to disease and disorder Received May 27, 2011; accepted July 6, 2011; published online July 19, 2011 Mika Shirasu and Kazushige Touhara* Human body odours also have this function; we emit a wide array of volatile organic compounds (VOCs), Department of Applied Biological Chemistry, Graduate School of both odorous and non-odorous, from our bodies. The Agricultural and Life Sciences, The University of Tokyo, Tokyo113-8657, Japan VOCs emitted from different areas of the human body vary with age, diet, sex, physiological status and pos- *Kazushige Touhara, Department of Applied Biological Chemistry, sibly genetic background. Therefore, body odours can The University of Tokyo, 1-1-1 Yayoi, Bunkyo-ku, Tokyo, Japan 113-8657. Tel: þ03 5841 5109, Fax: þ03 5841 8024, be considered as individual ‘odour-fingerprints’. email: [email protected] Pathological processes, such as infection and en- dogenous metabolic disorders, can influence our daily Hundreds of volatile organic compounds (VOCs) are odour fingerprints by producing new VOCs or by emitted from the human body, and the components of changing the ratio of VOCs that are produced nor- VOCs usually reflect the metabolic condition of an in- mally. Therefore, it is not surprising that physicians Downloaded from dividual. Therefore, contracting an infectious or meta- have used their olfactory senses to diagnose physical bolic disease often results in a change in body odour. conditions of patients. Around 400 BD, Hippocrates Recent progresses in analytical techniques allow rapid recognized the diagnostic usefulness of body odours analyses of VOCs derived from breath, blood, skin and and reported on several disease-specific odours ema- urine. -

Amino Acids & Proteins
Amino Acids & Proteins Amino Acids Amino acids are organic compounds containing both amino group & carboxyl group, those occurring in human proteins are L α-amino acids having the formula RCH(NH2)COOH & with the exception of glycine all amino acids are asymmetric . D-Amino acids that occur naturally are free D-serine& D- aspartate which present in the in brain tissue. Classification of Amino acids Over 300 amino acids occur naturally, however; only 20 of them share in the formation of proteins. Classification of amino acids either according to their R-group or to their nutritional importance. 1-Classification according to R-group(side chain). 1 2 2-Classification according to their nutritional importance All 20 amino acids present in proteins are biologically essential but not all of them are nutritionally essential, therefore, they are classified into: 3 A-Nutritionally essential amino acids :they should be supplement in diet because human body can not synthesize it , there deficiencies lead to kwashiorkor (protein malnutrition) & marasmus (protein & energy malnutrition). B-Nutritionally nonessential amino acids : human body can synthesize it , therefore , it’s not essential to be supplied in the diet. R-group It determines the property of amino acid in peptide formation as: 1-Since glycine is smallest amino acid, therefore, it can accommodate in places inaccessible to other amino acids in the formation of peptide. 4 2-Hydrophobic R-group of alanine, valine, leucine, Isoleucine, & aromatic R-groups of phenylalanine , tyrosine & tryptophan make them in the interior of protein. 3-The charged R-group of basic & acidic amino acids stabilize protein conformation through ionic interaction or salt-bridge. -

Annual Symposium of the Society for the Study of Inborn Errors of Metabolism Birmingham, UK, 4 – 7 September 2012
J Inherit Metab Dis (2012) 35 (Suppl 1):S1–S182 DOI 10.1007/s10545-012-9512-z ABSTRACTS Annual Symposium of the Society for the Study of Inborn Errors of Metabolism Birmingham, UK, 4 – 7 September 2012 This supplement was not sponsored by outside commercial interests. It was funded entirely by the SSIEM. 01. Amino Acids and PKU O-002 NATURAL INHIBITORS OF CARNOSINASE (CN1) O-001 Peters V1 ,AdelmannK2 ,YardB2 , Klingbeil K1 ,SchmittCP1 , Zschocke J3 3-HYDROXYISOBUTYRIC ACID DEHYDROGENASE DEFICIENCY: 1Zentrum für Kinder- und Jugendmedizin de, Heidelberg, Germany IDENTIFICATION OF A NEW INBORN ERROR OF VALINE 2Universitätsklinik, Mannheim, Germany METABOLISM 3Humangenetik, Innsbruck, Austria Wanders RJA1 , Ruiter JPN1 , Loupatty F.1 , Ferdinandusse S.1 , Waterham HR1 , Pasquini E.1 Background: Carnosinase degrades histidine-containing dipeptides 1Div Metab Dis, Univ Child Hosp, Amsterdam, Netherlands such as carnosine and anserine which are known to have several protective functions, especially as antioxidant agents. We recently Background, Objectives: Until now only few patients with an established showed that low carnosinase activities protect from diabetic nephrop- defect in the valine degradation pathway have been identified. Known athy, probably due to higher histidine-dipeptide concentrations. We deficiencies include 3-hydroxyisobutyryl-CoA hydrolase deficiency and now characterized the carnosinase metabolism in children and identi- methylmalonic semialdehyde dehydrogenase (MMSADH) deficiency. On fied natural inhibitors of carnosinase. the other hand many patients with 3-hydroxyisobutyric aciduria have been Results: Whereas serum carnosinase activity and protein concentrations described with a presumed defect in the valine degradation pathway. To correlate in adults, children have lower carnosinase activity although pro- identify the enzymatic and molecular defect in a group of patients with 3- tein concentrations were within the same level as for adults. -

Omics Knowledgebase for Mammalian Cellular Signaling Pathways
bioRxiv preprint doi: https://doi.org/10.1101/401729; this version posted August 27, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. The Signaling Pathways Project: an integrated ‘omics knowledgebase for mammalian cellular signaling pathways Scott Ochsner, David Abraham*, Kirt Martin*, Wei Ding, Apollo McOwiti, Zichen Wang, Kaitlyn Andreano, Ross A. Hamilton, Yue Chen, Angelica Hamilton, Marin L. Gantner, Michael Dehart, Shijing Qu, Susan G. Hilsenbeck, Lauren B. Becnel, Dave Bridges, Avi Ma’ayan, Janice M. Huss, Fabio Stossi, Charles E. Foulds, Anastasia Kralli, Donald P. McDonnell and Neil J. McKenna Address Correspondence To: Neil J. McKenna Department of Molecular and Cellular Biology Baylor College of Medicine Houston, TX 77030 USA e: [email protected] t: 713-798-8568 *These authors contributed equally to this study 1 bioRxiv preprint doi: https://doi.org/10.1101/401729; this version posted August 27, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Summary Public transcriptomic and ChIP-Seq datasets have the potential to illuminate facets of transcriptional regulation by mammalian cellular signaling pathways not yet explored in the research literature. Unfortunately, a variety of obstacles prevent routine re-use of these datasets by bench biologists for hypothesis generation and data validation. Here, we designed a web knowledgebase, the Signaling Pathways Project (SPP), which incorporates stable community classifications of three major categories of cellular signaling pathway node (receptors, enzymes and transcription factors) and the bioactive small molecules (BSMs) known to modulate their functions. -

Amino Acid Disorders Detected by Quantitative Amino Acid HPLC Analysis in Thailand: an Eight-Year Experience
ارا ه ت ه از $&% #ت "! Clinica Chimica Acta 413 (2012) 1141–1144 Contents lists available at SciVerse ScienceDirect Clinica Chimica Acta journal homepage: www.elsevier.com/locate/clinchim Amino acid disorders detected by quantitative amino acid HPLC analysis in Thailand: An eight-year experience Nithiwat Vatanavicharn ⁎, Pisanu Ratanarak, Somporn Liammongkolkul, Achara Sathienkijkanchai, Pornswan Wasant Division of Medical Genetics, Department of Pediatrics, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand article info abstract Article history: Background: Amino acid disorders are a major group of inborn errors of metabolism (IEM) with variable clin- Received 13 October 2011 ical presentations. This study was aimed to provide the data of amino acid disorders detected in high-risk Received in revised form 16 March 2012 Thai patients referred to our metabolic lab from all over the country. Accepted 20 March 2012 Methods: From 2001 to 2009, we analyzed amino acids by HPLC in 1214 plasma and cerebrospinal fluid spec- Available online 23 March 2012 imens. These specimens were obtained from patients with clinical suspicion of IEM or with positive newborn screening. The clinical data of the patients with confirmed diagnoses of amino acid disorders were also ana- Keywords: lyzed. Amino acid disorders HPLC Results: Fifty-eight patients were diagnosed with amino acid disorders, including 20 cases (34.5%) with maple Thailand syrup urine disease, 13 (22.4%) with phenylketonuria and hyperphenylalaninemia, 13 (22.4%) with nonke- totic hyperglycinemia, 9 (15.5%) with urea cycle defects, 2 (3.4%) with classical homocystinuria, and 1 (1.7%) with ornithine aminotransferase deficiency. There was considerable delay in diagnoses which led to poor outcomes in most patients. -
Test Requisition Form (Dna & Genetic Tests)
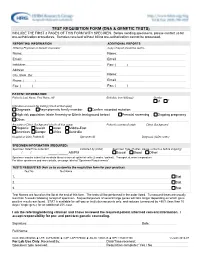
TEST REQUISITION FORM (DNA & GENETIC TESTS) INCLUDE THE FIRST 3 PAGES OF THIS FORM WITH SPECIMEN. Before sending specimens, please contact us for pre-authorization procedures. Samples received without billing pre-authorization cannot be processed. REPORTING INFORMATION ADDITIONAL REPORTS Ordering Physician or Genetic Counselor Copy of report should be sent to Name: Name: Email: Email: Institution: Fax: ( ) Address: City, State, Zip: Name: Phone: ( ) Email: Fax: ( ) Fax: ( ) PATIENT INFORMATION Patient's Last Name, First Name, MI Birthdate (mm/dd/yyyy) Gender M F Indication or reason for testing (check all that apply) Diagnosis Asymptomatic family member Confirm recorded mutation: High risk population (state Ancestry or Ethnic background below) Prenatal screening Ongoing pregnancy Other: Ancestry or Ethnic Background (check all that apply) Patient's country of origin Ethnic Background Hispanic Jewish Asian Middle-East Americas Europe Africa Australia Hospital or Clinic Patient ID Specimen ID Diagnosis (ICD9 codes) SPECIMEN INFORMATION (REQUIRED) Specimen Date/Time Collected Collected by (initial) Specimen Type (If other, please contact us before shipping) / / _____:_____ AM/PM Buccal Blood Other: Specimen may be submitted as whole blood or buccal epithelial cells (2 swabs / patient). Transport at room temperature. For other specimens and more details, see page labeled "Specimen Requirements". TESTS REQUESTED (Ask us to customize the requisition form for your practice) Test No. Test Name 1. Stat 2. Stat 3. Stat Test Names are found on the list at the end of this form. The tests will be performed in the order listed. Turnaround times are usually less than 5 weeks following receipt of specimen. Sequential panels of several large genes will take longer depending on which gene positive results are found. -

Catabolism of the Carbon Skeletons of Amino Acids
Bio. 2. ASPU. Lectu.3. Prof. Dr. F. ALQuobaili Catabolism of the Carbon Skeletons of Amino Acids • Biomedical Importance ‐ The metabolic diseases or "inborn errors of metabolism" associated with conversion of the carbon skeletons of the common L ‐‐amino acids to amphibolic intermediates can result in irreversible brain damage and .(ﺍﻟﻭﻓﺎﺓ) early mortality ‐ Prenatal or early postnatal detection and timely initiation of treatment thus are essential. Almost all states conduct screening tests for up to as many as 30 metabolic diseases. ‐ The best screening tests use tandem mass spectrometry to detect, in a few drops of neonate blood, catabolites suggestive of a metabolic defect. ‐ Treatment consists primarily of feeding diets low in the amino acids whose catabolism is impaired. • Transamination Typically Initiates Amino Acid Catabolism Removal of ‐amino nitrogen by transamination is the first catabolic reaction of amino acids except for proline, hydroxyproline, threonine, and lysine. The hydrocarbon skeleton that remains is then degraded to amphibolic intermediates. • Asparagine, Aspartate, Glutamine, and Glutamate All four carbons of asparagine and aspartate form oxaloacetate. Analogous reactions convert glutamine and glutamate to ‐ ketoglutarate. No metabolic defects are associated with the catabolism of these four amino acids. • Proline The catabolism of proline takes place in mitochodria. Since proline does not participate in transamination, the nitrogen of this imino acid is retained throughout its oxidation to 1‐ pyrolline‐5‐carboxylate, ring opening to glutamate‐‐ semialdehyde, and oxidation to glutamate, and is only removed during transamination of glutamate to ‐ketoglutarate. There are two metabolic disorders of proline catabolism. Both types are inherited as autosomal recessive traits, and are consistent with a normal adult life. -

Genetic Testing Stories
genetic alliance monograph series number 2 Genetic testinG stories nicole exe, ms heather Ferguson, ms, cgc alyson Krokosky samantha sawyer sharon F. terry, ma published by genetic alliance Genetic testinG stories nicole exe, ms heather Ferguson, ms, cgc alyson Krokosky samantha sawyer sharon F. terry, ma published by genetic alliance 1 Genetic Alliance is grateful to the individuals and families who so generously shared their stories. They offer us a model of openness that benefits all. Partial funding for this report was provided by the Genetics and Public Policy Center. The Center is supported at Johns Hopkins University by The Pew Charitable Trusts. Any opinions expressed in this report are those of the author(s) and do not necessarily reflect the views of The Pew Chari- table Trusts or the Genetics and Public Policy Center. This report may not be reproduced or distributed in whole or in part without the permission of the Genetics and Public Policy Center. Funding for this work was also provided by the Health Resources and Services Administration, Maternal Child Health Bureau, Genetics Services Branch, cooperative agreement # 1 U33MC07945-01-00, and Genetic Alliance. 4301 connecticut ave., nW, suite 404 Washington, dc 20008 t: 202.966.5557 F: 202.966.8553 www.geneticalliance.org 2 Table of Contents PREFACE 4 HYPOKALEMIC PERIODIC PARALYSIS Adult 26 CARRIER TESTING 5 HYPOSPADIAS/CHROMOSOMAL DEFECTS Child 27 22Q11.2 DELETION SYNDROME KLINEFELTER SYNDROME Adult 27 Adult/Newborn 5 MEDIUM CHAIN ACYL COA DEHYDROGENASE ADRENOLEUKODYSTROPHY