District Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brief Industrial Profile of ARWAL District
Government of India Ministry of MSME Brief Industrial Profile of ARWAL District Carried out by MSME-Development Institute (Ministry of MSME, Govt. of India,) Patliputra Industrial Estate, Patna-13 Phone:- 0612-2262719, 2262208, 2263211 Fax: 0612-2262186 e-mail: [email protected] Web- www.msmedipatna.gov.in 1 Contents S. No. Topic Page No. 1. General Characteristics of the District 3 1.1 Location & Geographical Area 3 1.2 Topography 3 1.3 Availability of Minerals. 3 1.4 Forest 4 1.5 Administrative set up 4 2. District at a glance 4 2.1 Existing Status of Industrial Area in the District -------- 7 3. Industrial Scenario Of --------- 8 3.1 Industry at a Glance 8 3.2 Year Wise Trend Of Units Registered 8 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The 9 District 3.4 Large Scale Industries / Public Sector undertakings 10 3.5 Major Exportable Item 10 3.6 Growth Trend 10 3.7 Vendorisation / Ancillarisation of the Industry 10 3.8 Medium Scale Enterprises 10 3.8.1 List of the units in ------ & near by Area 10 3.8.2 Major Exportable Item 10 3.9 Service Enterprises 10 3.9.2 Potentials areas for service industry 11 3.10 Potential for new MSMEs 11 4. Existing Clusters of Micro & Small Enterprise 11 4.1 Detail Of Major Clusters 11 4.1.1 Manufacturing Sector 11 4.1.2 Service Sector 11 4.2 Details of Identified cluster 11 5. General issues raised by industry association during the course of 11 meeting 6 Steps to set up MSMEs 12 2 Brief Industrial Profile of Arwal District 1. -
District Health Action Plan 2011 – 2012
DISTRICT HEALTH ACTION PLAN 2011 – 2012 District Patna District Patna District Patna District Patna Kako Modanganj Jehanabad Ratni Faridpur District Nalanda Ghosi Makhdumpur District Arwal Hulasganj District Gaya Name of District: - Jehanabad Please purchase 'PDFcamp Printer' on http://www.verypdf.com/ to remove this message. Acknowledgements This District Health Action plan prepared Under a Short & Hard Process of about survey of one month and this was a good Opportunity to revisit the situation of health services status and national programmes in district as well as to have a positive dialogue with departments like Public Health Engineering, Women and Child Development, Maternal and Child Health care etc. This document is an outcome of a collective effort by a number of individuals, related to our institutions and programmes:- Smt. Palka Shahni ,Chairperson of District Health Society, Jehanabad was a source of inspiration towards this effort vide her inputs to this process during D.H.S review meetings. Dr.Arvind kumar (A.C.M.O) Nodal officer for this action plan who always supported this endeavor through his guiding words and language. Mr. Nimish Manan , District Programme Manager was in incharge for the development of the DHAP(2011-12) . Mr Ravi Shankar Kumar , Distirct Planning Coordinator has given full time effort in developing DHAP(2011-12). Mr. Kaushal Kumar Jha, District Account Manager has put huge effort in financial Planning. Mr. Arvind Kumar, M&E Officer is the technical advisor for the data introduced inside this DISTRICT HEALTH ACTION PLAN. Mr. Manish Mani & Sefali from PHRN have given huge support. All district level Programme officer for various Health Programmes, B.H.Ms, M.O.I .Cs, PHCs, Field Office Staff have supported with their full participations, cooperation and learning spirit through out this process. -

DISTRICT : Champaran-W
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Champaran-W 1 PUSHPASRI NARENDRA w/o- narendra kumar 06-Feb-72 BC 900 675 75 Nawada (21) Saharsa (6) Champaran-W Patna (35) Purnia (6) KUMAR vill- jagatpur (1) post- harnaut dist- nalanda pin code- 803110 2 RENU KUMARISRI SURENDRA c/o sri surendra prasad 05-Feb-69 BC 900 672 74.67 Nalanda (32) Kaimur (3) Jahanabad (25) Gaya (24) Champaran-W (2) PRASAD SINGH singh, village+post khaddi lodipur, via- akanger sarai, district- nalanda, bihar pin 801301 3 KUMARI APARNA ASHOK KUMAR vill- bhojit pur, post- 16-Apr-83 BC 700 511 73 Champaran-E (7) Champaran-W Madhubani (2) Darbhanga (13) Muzaffarpur (23) PRIYA ekangar sarai, dist- (3) nalanda. 4RINA KUMARISRI KUMAR MAHTO d/o sri kumar mahto, 08-Dec-83 SC 500 365 73 Champaran-E (6) Champaran-W Sitamarahi (8) Madhubani (4) Patna (69) village- sakhuanwan, (4) post- gounoli, p.s. walmiki nagar, district- pachim champaran, bihar pin 845107 5RINA KUMARIMANOJ KUMAR vill- muzaffarpur, post- 28-Oct-88 BC 700 508 72.57 Champaran-E (8) Champaran-W Madhubani (5) Darbhanga (16) Samastipur (29) kathoule, disst- nalanda. (5) 6 SUCHITRA VIKASH PRASAD w/o- vikash prasad, 08-Feb-83 BC 700 507 72.43 Champaran-W Champaran-E (9) Madhubani (8) Darbhanga (18) Samastipur (32) KUMARI vill+post- ajnaura, (6) nalanda 7KUMARI SRI AMRESH musahari nagin -

2011-2012 West-Champaran, Bihar
Ch F-X ang PD e w w m w Click to buy NOW! o . .c tr e ac ar DISTRICT HEALTH ACTION PLAN ker-softw 2011-2012 DISTRICT HEALTH SOCIETY West-Champaran, Bihar 1 Ch F-X ang PD e w w m PREFACE w o Click to buy NOW! . .c tr e ac ar ker-softw National Rural Health Mission (NRHM) is one of the major health schemes run by Ministry of health and family welfare, GoI. The basic concept of the mission is to enhance the access of Quality health services to the poorest of the poor of the society and improve the health status of the community. It envisages to improve the health status of the rural mass through various programmes. All the health services should be provided to the pregnant women such as ANC checkups, Post Natal Care, IFA tablets for restricting the enemia cases and other reproductive child health releted services. It also focuses on promotion of institutional delivery for restricting the infant and as well as maternal deaths. Immunization is also a very important component which plays a vital role in child and mother health. Family planning and control of other diseases are also other focus areas. The NRHM has a strong realization that it is important to involve community for the improvement of health status of the community through various stake holders such as ASHA, AWWs, PRI, NGOs etc. ASHA is a link worker between the client and the health service providers. The skill of the health functionaries such as ANMs LHVs should be upgraded through proper orientation to ensure quality of care in health services . -

Organization Profile
SANKALP JYOTI ORGANIZATION PROFILE Vision : To have healthy and self reliant society where equal opportunities are made available to the disadvantaged with special reference to women. Mission : To create a self reliant society of disadvantaged & marginalized groups who can avail equal opportunities in which woman play proactive role. Goal : Sustainable development of the society through women empowerment. Activities of the organization:- 1. We are actively participating in Mission Indradhanush(MI) program on Immunization in Bihar along with the support of BVHA, Alliance for Immunization in India & GAVI. 2. With the support of BVHA & KKS we conducted Skill Development Training Program on Beautician, Electrician, Masonry, Cycle-Motor repairing at 12 villages of Maner block in Patna districts of Bihar. 3. With the support of Agriculture department of GoB, We are mobilizing & mapping the farmers to develop the Bio-Gas plant in Patna, Gaya,Vaishali, Muzafarpur & Darbhanga district of Bihar. 4. Organized one day workshop on Bihar Baal Ghoshnapatra- Children Manifesto on the occasion of Bihar Legislative Assembly- 2015 with issues of Child, Health & Nutrition with the support of World Vision-Bihar in Kishanganj district 5. With the support of Dan Church Aid & IDF we procured the 7500 kg. SEED of rice to distribute among the dalit communities of Katra & Sonepur panchayat of Katra Block in Muzaffarpur district. 6. We are conducting Skill Development Training program on ICT, Yoga, Mass-communication, Soft Skill, Tailoring, Beauty Advisor under MES scheme of DGET in Patna district with the support of Ministry of Labour & employment Department, GOI. SANKALP JYOTI 7. We had translated the training material from English to Hindi on Emotional Resilience & Health under the Girls First project for the U.S. -
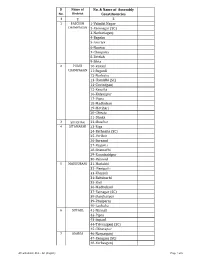
AC with District Dist
Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 1 PASCHIM 1-Valmiki Nagar CHAMPARAN 2-Ramnagar (SC) 3-Narkatiaganj 4-Bagaha 5-Lauriya 6-Nautan 7-Chanpatia 8-Bettiah 9-Sikta 2 PURVI 10-Raxaul CHAMPARAN 11-Sugauli 12-Narkatia 13-Harsidhi (SC) 14-Govindganj 15-Kesaria 16-Kalyanpur 17-Pipra 18-Madhuban 19-Motihari 20-Chiraia 21-Dhaka 3 SHEOHAR 22-Sheohar 4 SITAMARHI 23-Riga 24-Bathnaha (SC) 25-Parihar 26-Sursand 27-Bajpatti 28-Sitamarhi 29-Runnisaidpur 30-Belsand 5 MADHUBANI 31-Harlakhi 32- Benipatti 33-Khajauli 34-Babubarhi 35-Bisfi 36-Madhubani 37-Rajnagar (SC) 38-Jhanjharpur 39-Phulparas 40-Laukaha 6 SUPAUL 41-Nirmali 42-Pipra 43-Supaul 44-Triveniganj (SC) 45-Chhatapur 7 ARARIA 46-Narpatganj 47-Raniganj (SC) 48-Forbesganj AC with district Dist. - AC (English) Page 1 of 6 Sl Name of No. & Name of Assembly No. District Constituencies 1 2 3 49-Araria 50-Jokihat 51-Sikti 8 KISHANGANJ 52-Bahadurganj 53-Thakurganj 54-Kishanganj 55-Kochadhaman 9 PURNIA 56-Amour 57-Baisi 58-Kasba 59-Banmankhi (SC) 60-Rupauli 61-Dhamdaha 62-Purnia 10 KATIHAR 63-Katihar 64-Kadwa 65-Balrampur 66-Pranpur 67-Manihari (ST) 68-Barari 69-Korha (SC) 11 MADHEPURA 70-Alamnagar 71-Bihariganj 72-Singheshwar (SC) 73-Madhepura 12 SAHARSA 74-Sonbarsha (SC) 75-Saharsa 76-Simri Bakhtiarpur 77-Mahishi 13 DARBHANGA 78-Kusheshwar Asthan (SC) 79-Gaura Bauram 80-Benipur 81-Alinagar 82-Darbhanga Rural 83-Darbhanga 84-Hayaghat 85-Bahadurpur 86-Keoti 87-Jale 14 MUZAFFARPUR 88-Gaighat 89-Aurai 90-Minapur 91-Bochaha (SC) 92-Sakra (SC) 93-Kurhani 94-Muzaffarpur 95-Kanti 96-Baruraj AC with district Dist. -

Municipal Solid Waste Mangement in City Motihari
International Journal of Scientific & Engineering Research, Volume 8, Issue 4, April-2017 394 ISSN 2229-5518 MUNICIPAL SOLID WASTE MANGEMENT IN CITY MOTIHARI KUSUM KUMARI Ro ABSTRACT:Waste is a continually growing problem at global and regional as well as at local levels. Solid wastes arise from human and animal activities that are normally discarded as useless or unwanted. In other words, solid wastes may be defined as the organic and inorganic waste materials produced by various activities of the society and which have lost their value to the first user. As the result of rapid increase in production and consumption, urban society rejects and generates solid material regularly which leads to considerable increase in the volume of waste generated from several sources such as, domestic wastes, commercial wastes, institutional wastes and industrial wastes of most diverse categories. Management of solid waste may be defined as that discipline associated with the control of generation, storage, collection, transfer and transport, processing, and disposal of solid wastes in a manner that is in accord with the best principles of public health, economics, engineering, conservation, aesthetics, and other environmental considerations. In its scope, solid waste management includes all administrative, financial, legal, planning, and engineering functions involved in the whole spectrum of solutions to problems of solid wastes thrust upon the community by its inhabitants. Solid wastes have the potential to pollute all the vital components of living environment (i.e., air, land and water) at local and at global levels. The problem is compounded by trends in consumption and production patterns and by continuing urbanization of the world. -

National Highways Authority of India Request for Proposal for IE
National Highways Authority of India Request for Proposal for IE National Highways Authority of India (Ministry of Road Transport & Highways, Govt. of India) Regional Office, Patna, D-63, Sri Krishnapuri Patna (Bihar) Independent Engineer services for O&M Period for “the work of 4-laning of Kotwa – Mehsi- Muzaffarpur Section from km 440.00 to km 520.00 (Total Length 80.00 Km) of NH 28 in the State of Bihar. Tender No. - 62/RO-PATNA/NHAI/2019-20 REQUEST FOR PROPOSAL (RFP) March 2020 CONTENTS Particulars SECTION 1: INFORMATION TO CONSULTANTS .......................................................................... 1-8 SECTION 2: LETTER OF INVITATION TO CONSULTANTS ..................................................... 9-32 SECTION 3: FORMATS FOR SUBMISSION OF FIRMS CREDENTIALS .............................. 33-35 SECTION 4: FORMAT FOR SUBMISSION OF TECHNICAL PROPOSAL ............................. 36-52 SECTION 5: FORMAT FOR SUBMISSION OF FINANCIAL PROPOSAL. ............................. 53-58 SECTION 6: TERMS OF REFERENCE FOR INDEPENDENT ENGINEER ........................ 59-142 SECTION 7: DRAFT FORM OF CONTRACT ............................................................................ 143-190 REQUEST FOR PROPOSAL (RFP) SECTION 1: INFORMATION TO CONSULTANTS Sub.: Independent Engineer services for O&M Period for “the work of 4-laning of Kotwa – Mehsi- Muzaffarpur Section from km 440.00 to km 520.00 (Total Length 80.00 Km) of NH 28”. GENERAL:- 1. The National Highways Authority of India invites proposals for engaging an Independent Engineer (IE) on the basis of International Competitive Bidding for the following contract package in the State of Bihar. TABLE 1: DETAILS OF PROJECT S No Consultancy NH State Project Stretch Project Length Assignment Package No. (Km)/Total period Project Cost (Cr.) (months) 1 Independent Engineer Services 28 Bihar Kotwa – 80.00 km 36 Months for O&M Period for Mehsi- “the work of 4- Muzaffarpur laning of Kotwa – Section from Mehsi- km 440.00 to Muzaffarpur km 520.00 Section from km 440.00 to km 520.00 (Total Length 80.00 Km) of NH 28”. -

Deo List Bihar
Details of DEO-cum-DM Sl. No. District Name Name Designation E-mail Address Mobile No. 1 2 3 4 5 6 1 PASCHIM CHAMPARAN Kundan Kumar District Election Officer [email protected] 9473191294 2 PURVI CHAMPARAN Shirsat Kapil Ashok District Election Officer [email protected] 9473191301 3 SHEOHAR Avaneesh Kumar Singh District Election Officer [email protected] 9473191468 4 SITAMARHI Abhilasha Kumari Sharma District Election Officer [email protected] 9473191288 5 MADHUBANI Nilesh Ramchandra Deore District Election Officer [email protected] 9473191324 6 SUPAUL Sri Mahendra KUMAR District Election Officer [email protected] 9473191345 7 ARARIA Prashant Kumar District Election Officer [email protected] 9431228200 8 KISHANGANJ Aditya Prakash District Election Officer [email protected] 9473191371 9 PURNIA Rahul Kumar District Election Officer [email protected] 9473191358 10 KATIHAR Kanwal Tanuj District Election Officer [email protected] 9473191375 11 MADHEPURA Navdeep Shukla District Election Officer [email protected] 9473191353 12 SAHARSA Kaushal kumar District Election Officer [email protected] 9473191340 13 DARBHANGA Shri Thiyagrajan S. M. District Election Officer [email protected] 9473191317 14 MUZAFFARPUR Chandra Shekhar Singh District Election Officer [email protected] 9473191283 15 GOPALGANJ Arshad Aziz District Election Officer [email protected] 9473191278 16 SIWAN Amit Kumar Pandey District Election Officer [email protected] 9473191273 17 SARAN Subrat Kumar Sen District -

Glimpses of Sugarcane Varietal Screening and Improvement at Pusa, Bihar
ACTA SCIENTIFIC AGRICULTURE (ISSN: 2581-365X) Volume 4 Issue 3 March 2020 Review Article Glimpses of Sugarcane Varietal Screening and Improvement at Pusa, Bihar Balwant Kumar* Received: January 18, 2020 SRI, DRPCAU, Pusa, Bihar, India Published: February 08, 2020 Balwant Kumar, SRI, DRPCAU, Pusa, Bihar, India. *Corresponding Author: © All rights are reserved by Balwant DOI: 10.31080/ASAG.2020.04.0793 Kumar. Abstract Sugarcane is primarily grown in nine states of India namely; Uttar Pradesh, Maharashtra, Andhra Pradesh, Bihar, Gujarat, Haryana, Karnataka, Punjab, and Tamil Nadu. During early 19th century sugarcane cultivation started as cash crop and number of sugar facto- ries open keeping in view a glimpses of sugarcane varietal screening and Improvement has been reviewed and found that Bihar was rich in term of sugar factories and its 20-40% share in national sugar production was already reported. It was the introduction of Co seedling that replace local varieties under cultivation those were Co 210, Co213, Co 214, Co 313, Co 331, Co 513,Co 356, Co 395,Co 453,Co508 and CoK 32, Co 383, Co 622,Co 419,Co 617,Co1148 and Co 1158 while in present varietal scenario cultivated varieties are Co 0238, Co 0118, Co 98014, CoP 9301, CoLk 94184, CoP 112, CoSe 01434, CoP 09437, BO 154 and CoP 16437. It was also found that POJ 2878, Co285, Co281, CP 28/11, Co213 & Co205 were mainly responsible for improvement in high yield and high sugar. The varietal development and evaluation of sugarcane varieties started in Bihar by after that Central Sugarcane Research Institute was established 1932 since then total 281 clones were developed at SRI, while several Sugarcane varieties of other place were also evalu- ated. -

DISTRICT : Muzaffarpur
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Muzaffarpur 1 KIRAN KUMARIARVIND KUMAR kiran kumari c/o arvind 10-Dec-66 GEN 700 603 86.14 Muzaffarpur (1) Samastipur (1) Darbhanga (1) Vaishali (1) Champaran-E (1) kumar vill+po-parsara dis-muzaffarpur 2 ARCHANA SRI ARUN vill-ratanpur post- 11-Aug-85 ST 900 757 84.11 Muzaffarpur (2) KUMARI CHAUDHARY jagdishparn vhaya- kalyanapur dist- muzaffarpur pin-848302 3PREM LATA SHARI NAND LAL village raja bigha, p.s. 10-Jan-79 GEN 700 566 80.86 Saran (2) Muzaffarpur (3) Darbhanga (2) Gaya (4) Champaran-E (2) KUMARI PRASAD dhanarua. p.o barni district patna pin code 804452 4 REENA SINHASRI DINESH SINGH dinesh singh, d/o- sita 31-Dec-76 BC 900 721 80.11 Siwan (2) Begusarai (3) Muzaffarpur (4) Samastipur (4) Vaishali (5) sharan singh, vill- ruiya, post- ruiya bangra, p.s.- jiradei, distt- siwan 5NILAM SHRI GUJESHWER nilam srivastav c/o-shri 06-Jan-69 BC 700 554 79.14 Gopalganj (2) Siwan (3) Saran (3) Muzaffarpur (5) Patna (14) SRIVASTAV PRASAD akhilesh prasad vill-manichapar, po-hathua dis-gopalginj pin-841436 6 BEENA KUMARIMAHARANGHI vill-mahrana 01-Oct-75 BC 900 700 77.78 Munger (17) Lakhisarai (11) Bhagalpur (15) Muzaffarpur (6) Jamui (12) MATHO po-dahara dis-munger pin-811201 7 KANAK LATASRI ANIL KUMAR village+post- dahibhatta, 23-Dec-85 GEN 700 541 77.29 Gopalganj (5) -
West Champaran Introduction
DISTRICT PROFILE WEST CHAMPARAN INTRODUCTION West Champaran is an administrative district in the state of Bihar. West Champaran district was carved out of old champaran district in the year 1972. It is part of Tirhut division. West Champaran is surrounded by hilly region of Nepal in the North, Gopalganj & part of East Champaran district in the south, in the east it is surrounded by East Champaran and in the west Padrauna & Deoria districts of Uttar Pradesh. The mother-tongue of this region is Bhojpuri. The district has its border with Nepal, it has an international importance. The international border is open at five blocks of the district, namely, Bagha- II, Ramnagar, Gaunaha, Mainatand & Sikta, extending from north- west corner to south–east covering a distance of 35 kms . HISTORICAL BACKGROUND The history of the district during the late medieval period and the British period is linked with the history of Bettiah Raj. The British Raj palace occupies a large area in the centre of the town. In 1910 at the request of Maharani, the palace was built after the plan of Graham's palace in Calcutta. The Court Of Wards is at present holding the property of Bettiah Raj. The rise of nationalism in Bettiah in early 20th century is intimately connected with indigo plantation. Raj Kumar Shukla, an ordinary raiyat and indigo cultivator of Champaran met Gandhiji and explained the plight of the cultivators and the atrocities of the planters on the raiyats. Gandhijii came to Champaran in 1917 and listened to the problems of the cultivators and the started the movement known as Champaran Satyagraha movement to end the oppression of the British indigo planters.