To This Drug but the Results Were Negative (J. D. Unpublished Observations). Since No Resistance Mechanism Had Been Detected To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Resistance to Paromomycinis Conferred by Rpsl Mutations
VOL.53 NO. 12, DEC.2000 THE JOURNAL OF ANTIBIOTICS pp.1424 - 1427 COMMUNICATIONS TO THE EDITOR Resistance to Paromomycinis Conferred by paromomycin at a frequency of 10 7 or 10 8, respectively. rpsL Mutations, Accompaniedby an Out of 77 randomly selected paromomycin resistant Enhanced Antibiotic Production in mutants, 4 strains, designated as KO-347-350, were found to produce actinorhodin in 7 to 10-fold greater amounts Streptomyces coelicolor A3 (2) than the parent strain (Table 1). In our previous studies10'11>14) we established that an antibiotic- Sir: overproducing characteristic frequently appears together Aminoglycoside antibiotics interfere with bacterial with the mutation within the rpsL gene. To address this protein synthesis by binding to the 3OS ribosomal relationship weexamined for the presence of mutations in subunit1>2). Their binding is known to stabilize the tRNA- rpsL. Strikingly, all antibiotic-overproducing mutants mRNAinteraction in the A-site by decreasing the tRNA (Class I) examined had rpsL mutations, resulting in the dissociation rates3). Eventually, aminoglycoside antibiotics alteration of amino acid residue 91 from proline to serine cause a decrease in translational accuracy and inhibit (Table 1). In contrast, another group of paromomycin translocation of the ribosome. Such detrimental effects of resistant mutant, (Class II; KO-351-356) which do not aminoglycoside antibiotics can be circumvented by overproduce antibiotic, was found to have no mutation mutations altering 16S rRNA4~6) or certain ribosomal within the rpsL gene. It should be pointed out that Class I proteins6^; these mutations have been found in either the mutants displayed a higher level of resistance to nucleotide 530 or 915 regions of 16S rRNAor in ribosomal paromomycin than that of Class II mutants (Table 1). -

Inhalation Solution, USP for Oral Inhalation Use What Is Tobramycin
PATIENT INFORMATION TOBRAMYCIN (TOE-BRA-MYE-SIN) Inhalation Solution, USP for oral inhalation use What is Tobramycin Inhalation Solution? Tobramycin inhalation solution is a prescription medicine that is used to treat people with cystic fibrosis who have a bacterial infection called Pseudomonas aeruginosa. Tobramycin inhalation solution contains an antibacterial medicine called tobramycin (an aminoglycoside). It is not known if tobramycin inhalation solution is safe and effective: in children under 6 years of age in people who have an FEV1 less than 25% or greater than 75% predicted in people who are colonized with a bacterium called Burkholderia cepacia Do not take tobramycin inhalation solution if you are allergic to tobramycin, any of the ingredients in tobramycin inhalation solution, or to any other aminoglycoside antibacterial. See the end of this Patient Information for a complete list of ingredients in tobramycin inhalation solution. Before you take tobramycin inhalation solution, tell your healthcare provider about all of your medical conditions, including if you: have or have had hearing problems (including noises in your ears such as ringing or hissing) have dizziness have or have had kidney problems have or have had problems with muscle weakness such as myasthenia gravis or Parkinson’s disease have or have had breathing problems such as wheezing, coughing, or chest tightness are pregnant or plan to become pregnant. Tobramycin inhalation solution is in a class of drugs that can harm your unborn baby. are breastfeeding or plan to breastfeed. It is not known if tobramycin passes into your breast milk. are receiving aminoglycoside therapy by injection or through a vein (intravenous) while taking tobramycin inhalation solution. -

Effects of Antibiotics on the Bactericidal Activity of Human Serum
Journal of Antimicrobial Chemotherapy (1982)9,141-148 Effects of antibiotics on the bactericidal activity of human serum Downloaded from https://academic.oup.com/jac/article/9/2/141/712569 by guest on 28 September 2021 Anna Fietta, Patrizia Mangiarotti and Giuliana Gialdroni Grassi Istituto Forlanini, University ofPavia, Italy The interaction between several antibiotics and either normal human serum or EGTA-chelated Mg-treated serum has been tested. Synergism has been observed with rifampicin, tetracycline and doxycycline, but not with minocycline, amino- glycosides (kanamycin, tobramycin, gentamicin, sisomicin and amikacin), chloramphenicol, fosfomycin and erythromycin. It has been demonstrated that Escherichia coli K12 strains bearing plasmids, conferring resistance to tetra- cycline, were killed in the presence of serum. Evidence has been presented that this synergistic action depends on com- plement and can be abolished by serum treatment with ethyleneglycol-tetraacetic acid. Introduction Interference of antimicrobial agents on several reactions involved in the host defence system has been demonstrated by many authors. It has been suggested that resistance to serum bactericidal activity can be an important factor in determining virulence of some Gram-negative bacteria (Durack & Beeson, 1977; Elgefors & Oiling, 1978; Howard & Glynn, 1971; McCabe et al., 1978; Medearis & Kenny, 1968; Oiling et al, 1973; Roantree & Rantz, 1960; Rowley, 1954), and serum bactericidal activity is an important mechanism of defence against bacterial invasion and spread (Agnella, 1978; McCabe et al, 1978; Roantree & Rantz, 1960; Johnston & Strand, 1977). Many Gram-negative Enterobacteriaceae causing bacteraemia are resistant to the bactericidal action of serum (Rowley & Wardlaw, 1958; Vosti & Randall, 1970). Conversion of serum-resistant Escherichia coli to serum-susceptible has been observed after treatment with diphenylamine (Feingold, 1969). -

P147-Bioorgchem-Kanamycin Nucleotidyltransferase-1999.Pdf
Bioorganic Chemistry 27, 395±408 (1999) Article ID bioo.1999.1144, available online at http://www.idealibrary.com on Kinetic Mechanism of Kanamycin Nucleotidyltransferase from Staphylococcus aureus1 Misty Chen-Goodspeed,* Janeen L. Vanhooke,² Hazel M. Holden,² and Frank M. Raushel*,2 *Department of Chemistry, Texas A&M University, College Station, Texas 77843; and ²Department of Biochemistry, Institute for Enzyme Research, University of Wisconsin, Madison, Wisconsin 53705 Received December 16, 1998 Kanamycin nucleotidyltransferase (KNTase) catalyzes the transfer of the adenyl group from MgATP to either the 4Ј or 4Љ-hydroxyl group of aminoglycoside antibiotics. The steady state kinetic parameters of the enzymatic reaction have been measured by initial velocity, product, and dead-end inhibition techniques. The kinetic mechanism is ordered where the antibiotic binds prior to MgATP and the modified antibiotic is the last product to be released. The effects of altering the relative solvent viscosity are consistent with the release of the products as the rate-limiting step. The pH profiles for Vmax and V/KATP show that a single ionizable group with apK of ϳ8.9 must be protonated for catalysis. The V/K profile for kanamycin as a function of pH is bell-shaped and indicates that one group must be protonated with a pK value of 8.5, while another group must be unprotonated with a pK value of 6.6. An analysis of the kinetic constants for 10 different aminoglycoside antibiotics and 5 nucleotide triphosphates indicates very little difference in the rate of catalysis or substrate binding among these substrates. ᭧ 1999 Academic Press Key Words: kanamycin nucleotidyltransferase; antibiotic modification. -

A New Mutation in 16S Rrna Ofescherichia Coli
464-466 Nucleic Acids Research, 1995, Vol. 23, No. 3 Q-D/ 1995 Oxford University Press A new mutation in 16S rRNA of Escherichia coli conferring spectinomycin resistance Urban Johanson and Diarmaid Hughes* Department of Molecular Biology, Uppsala University, Biomedical Center, S-751 24 Uppsala, Sweden Received September 24, 1994; Revised and Accepted December 30, 1994 ABSTRACT 1067 1089 A -U We report a novel mutation, Cl 066U in 16S rRNA which was selected for resistance to spectinomycin, an U @- G4C antibiotic which inhibits ribosomal translocation. The U,A,C e- G,U,A minimal inhibitory concentration (MIC) of spectinomy- A cin determined for this mutant (15 pg/ml) is greater U U than with the wild-type plasmid (5 ig/ml) but lower than 1062 1194 with the well known C1192U mutation (>80 pg/ml). The Cl 066U mutation also increases the cells sensitivity to Figure 1. Secondary structure of the upper part of helix 34 of 16S rRNA in fusidic acid, another antibiotic which inhibits transla- Ecoli (24) with the novel C1066U mutation indicated by an open U. In tion at the translocation stage, whereas C1192U is addition, all other known SpcR mutations are shown. The mutations are A1191G,C, Gi 193A in C.reinhardtii chloroplast (25); G1064A (20), A1191C, unchanged relative to the wild type. We discuss why Cl 192U (26) inN.tabacum chloroplast; GI 193A (20) inN.undulata chloroplast the acquisition of resistance to one of these drugs is and C1192U (1), C1192U,G,A (19), G1064U,C,A, G1064U-C1192A, often associated with hypersensitivity to the other. -

Guidance for Treatment of Covid-19 in Adults and Children
GUIDANCE FOR TREATMENT OF COVID-19 IN ADULTS AND CHILDREN Patient population: Adults and pediatric patients with COVID-19 infection, who are admitted on an inpatient floor or to the intensive care unit. Key points: Details regarding isolation/precautions, personal protective equipment, patient movement, family/visitor policy, and cleaning/disinfection can be found here. Clinical symptoms: Range from asymptomatic, uncomplicated upper respiratory tract viral infection to pneumonia, acute respiratory distress syndrome (ARDS), sepsis, and septic shock (Table 1) Diagnosis: See current COVID-19 testing recommendations. Treatment: Based on data from several randomized control trials, Remdesivir may provide a modest benefit in a subgroup of patients hospitalized with COVID-19. See further details regarding patient populations (see below) and Table 2. Table 1. Potential Treatment Recommendations by Severity of Disease for Patients 18 Years or Older Most COVID-19 therapeutics have not been studied in children under 18. The below treatment recommendations may apply to some children, however should be addressed on a case-by-case basis and discussed with Pediatric Infectious Diseases. See specific sections for further details Disease severity Potential Treatment Recommendations (per ID consult discretion based on details in Table 2) Post-exposure prophylaxis • See Post-Exposure Prophylaxis Guidelines No supplemental oxygen • Supportive care • Monoclonal Antibodies may be an option in certain high-risk patients (see eligibility criteria in Table 2) admitted for reasons other than COVID-19 who have mild to moderate symptoms of COVID-19 Low flow supplemental oxygen • Supportive care • Dexamethasone (Exception: Minimal supplemental oxygen (1-2 L) in adults with <7 days of symptoms—uncertain benefit) • Remdesivir High flow supplemental oxygen or non- • Supportive Care invasive mechanical ventilation • Dexamethasone • Tocilizumab (NOTE: currently on shortage and not available for treatment of COVID-19 in patients 18 years an older. -

Farrukh Javaid Malik
I Farrukh Javaid Malik THESIS PRESENTED TO OBTAIN THE GRADE OF DOCTOR OF THE UNIVERSITY OF BORDEAUX Doctoral School, SP2: Society, Politic, Public Health Specialization Pharmacoepidemiology and Pharmacovigilance By Farrukh Javaid Malik “Analysis of the medicines panorama in Pakistan – The case of antimicrobials: market offer width and consumption.” Under the direction of Prof. Dr. Albert FIGUERAS Defense Date: 28th November 2019 Members of Jury M. Francesco SALVO, Maître de conférences des universités – praticien hospitalier, President Université de Bordeaux M. Albert FIGUERAS, Professeur des universités – praticien hospitalier, Director Université Autonome de Barcelone Mme Antonia AGUSTI, Professeure, Vall dʹHebron University Hospital Referee Mme Montserrat BOSCH, Praticienne hospitalière, Vall dʹHebron University Hospital Referee II Abstract A country’s medicines market is an indicator of its healthcare system, the epidemiological profile, and the prevalent practices therein. It is not only the first logical step to study the characteristics of medicines authorized for marketing, but also a requisite to set up a pharmacovigilance system, thus promoting rational drug utilization. The three medicines market studies presented in the present document were conducted in Pakistan with the aim of describing the characteristics of the pharmaceutical products available in the country as well as their consumption at a national level, with a special focus on antimicrobials. The most important cause of antimicrobial resistance is the inappropriate consumption of antimicrobials. The results of the researches conducted in Pakistan showed some market deficiencies which could be addressed as part of the national antimicrobial stewardship programmes. III Résumé Le marché du médicament d’un pays est un indicateur de son système de santé, de son profil épidémiologique et des pratiques [de prescription] qui y règnent. -
Bacterial Conjunctivitis
Clinical Ophthalmology Dovepress open access to scientific and medical research Open Access Full Text Article EVIDENCE to PRactICE Bacterial conjunctivitis Cindy Hutnik1 Clinical question: What is the best treatment for bacterial conjunctivitis? Mohammad H Results: Topical antibiotics expedite recovery from bacterial conjunctivitis. The choice of Mohammad-Shahi2 antibiotic usually does not affect outcome. Implementation: Recognition of key distinguishing features of bacterial conjunctivitis 1Ivey Eye Institute, St Joseph Healthcare, London, Ontario; 2Faculty • Pitfalls that can be recognized in the history and physical examination of Medicine, McGill University, • Choice of antibiotic Montreal, Quebec, Canada • When to refer for specialist treatment. Keywords: bacterial conjunctivitis, topical antibiotics Bacterial conjunctivitis Definition: Bacterial conjunctivitis is inflammation of the conjunctiva as a result of bacterial infection. Etiology: Most commonly Staphylococcus species in adults, and Streptococcus pneumonia and the Gram-negative organisms Haemophilus influenzae and Moraxella catarrhalis in children. Contact lens wearers are at particular risk for Gram-negative infections. such as Pseudomonas aeruginosa. Neisseria gonorrhoeae is primarily a neonatal etiology. Incidence: One recent study estimates an annual incidence rate of 135 per 10,000 in the US.1 Economics: The same study found the estimated total direct and indirect cost of treating bacterial conjunctivitis in the US to be $589 million annually. Accounting for a 20% variation in annual inci- dence rate and treatment cost resulted in an estimated cost range of $377 to $857 million per year. Level of evidence used in this summary: Systematic reviews, meta-analyses, and random- ized controlled trials from 1990 to 2010. Search sources: Ovid MEDLINE, PubMed, Cochrane Library, NHS evidence, Clinical Evidence. -
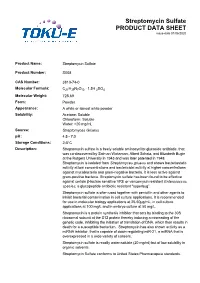
Streptomycin Sulfate PRODUCT DATA SHEET Issue Date 01/06/2020
Streptomycin Sulfate PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Streptomycin Sulfate Product Number: S008 CAS Number: 3810-74-0 Molecular Formula: C21H39N7O12 · 1.5H 2SO4 Molecular Weight: 728.69 Form: Powder Appearance: A white or almost white powder Solubility: Acetone: Soluble Chloroform: Soluble Water: >20 mg/mL Source: Streptomyces Griseus pH: 4.5 - 7.0 Storage Conditions: 28°C Description: Streptomycin sulfate is a freely soluble aminocyclitol glycoside antibiotic, that was co-discovered by Salman Waksman, Albert Schatz, and Elizabeth Bugie at the Rutgers University in 1943 and was later patented in 1948. Streptomycin is isolated from Streptomyces griseus and shows bacteriostatic activity at low concentrations and bactericidal activity at higher concentrations against mycobacteria and gram-negative bacteria. It is less active against gram-positive bacteria. Streptomycin sulfate has been found to be effective against certain βlactam sensitive VRE or vancomycin resistant Enterococcus species; a glycopeptide antibiotic resistant "superbug”. Streptomycin sulfate is often used together with penicillin and other agents to inhibit bacterial contamination in cell culture applications. It is recommended for use in molecular biology applications at 2550μg/mL, in cell culture applications at 100 mg/L and in embryo culture at 50 mg/L. Streptomycin is a protein synthesis inhibitor that acts by binding to the 30S ribosomal subunit at the S12 protein thereby inducing a misreading of the genetic code, inhibiting the initiation of translation of DNA, which then results in death for a susceptible bacterium. Streptomycin has also shown activity as a miRNA inhibitor, that is capable of down-regulating miR-21, a miRNA that is overexpressed in a wide variety of cancers. -

Neomycin—Production and Antibiotic Properties
NEOMYCIN—PRODUCTION AND ANTIBIOTIC PROPERTIES Selman A. Waksman, … , Hubert A. Lechevalier, Dale A. Harris J Clin Invest. 1949;28(5):934-939. https://doi.org/10.1172/JCI102182. Research Article Find the latest version: https://jci.me/102182/pdf NEOMYCIN-PRODUCTION AND ANTIBIOTIC PROPERTIES 1, 2 3 By SELMAN A. WAKSMAN, HUBERT A. LECHEVALIER, AND DALE A. HARRIS (From the Department of Microbiology, New Jersey Agricultural Experiment Station, Rutgers University, New Brunswick, N. J.) ANTIBIOTIC SURVEYS All these cultures proved to be highly active against mycobacteria. of During the last 10 years, a large number anti- Only few of the cultures, however, that gave biotics which are active against Gram-negative good activity by the agar-streak method yielded and Gram-positive bacteria, mycobacteria, rickett- filtrates which possessed corresponding potency. siae, and certain of the larger viruses were iso- This may be due to a variety of factors, such as lated (1) from various species and strains of the the formation by a single organism of more than genus Streptomyces. This served to focus atten- one antibiotic or the production of different anti- tion on the actinomycetes as potential producers of biotics under different conditions of culture. One antimicrobial agents that might possess promising of these cultures proved to be highly promising chemotherapeutic properties. The fact that nearly and was selected for more detailed investigations. 20 to 50%o of these organisms possess antimicrobial This culture was entered into the Collection as No. activities served to heighten this interest. Numer- 3535. The nature of its antimicrobial spectrum, ous surveys have been conducted. -

(ESVAC) Web-Based Sales and Animal Population
16 July 2019 EMA/210691/2015-Rev.2 Veterinary Medicines Division European Surveillance of Veterinary Antimicrobial Consumption (ESVAC) Sales Data and Animal Population Data Collection Protocol (version 3) Superseded by a new version Superseded Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of content 1. Introduction ....................................................................................................................... 3 1.1. Terms of reference ........................................................................................................... 3 1.2. Approach ........................................................................................................................ 3 1.3. Target groups of the protocol and templates ......................................................................... 4 1.4. Organization of the ESVAC project ...................................................................................... 4 1.5. Web based delivery of data ................................................................................................ 5 2. ESVAC sales data ............................................................................................................... 5 2.1. -

ZEMDRI (Plazomicin) Injection, for Intravenous Use (Ml/Min) ZEMDRI B Dosing Interval Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION Recommended initial dosage regimen for patients with renal These highlights do not include all the information needed to use impairment is shown in the table below. (2.3) ZEMDRI safely and effectively. See full prescribing Recommended information for ZEMDRI. Estimated CLcr a Dosage for ZEMDRI (plazomicin) injection, for intravenous use (mL/min) ZEMDRI b Dosing Interval Initial U.S. Approval: 2018 Greater than or equal to 60 15 mg/kg Every 24 hours WARNING: NEPHROTOXICITY, OTOTOXICITY, to less than 90 NEUROMUSCULAR BLOCKADE and FETAL HARM Greater than or equal to 30 10 mg/kg Every 24 hours See full prescribing information for complete boxed warning. to less than 60 Nephrotoxicity has been reported with ZEMDRI. The risk Greater than or equal to 15 10 mg/kg Every 48 hours of nephrotoxicity is greater in patients with impaired renal to less than 30 a CLcr estimated by the Cockcroft-Gault formula. (2.3) function, the elderly, and in those receiving concomitant b nephrotoxic medications. (5.1) Calculate dosage using Total Body Weight (TBW). For patients Ototoxicity, manifested as hearing loss, tinnitus, and/or with TBW greater than IBW by 25% or more, use adjusted body weight. (2.3) vertigo, has been reported with ZEMDRI. Symptoms of aminoglycoside associated ototoxicity may be irreversible See Full Prescribing Information for subsequent dosage and may not become evident until after completion of adjustment based on changes in renal function or Therapeutic therapy. (5.2) Drug Monitoring (TDM). (2.3, 2.4). Aminoglycosides have been associated with neuromuscular See Full Prescribing Information for instructions on preparation blockade.