National Neonatal Audit Programme (NNAP) 2018 Annual Report on 2017 Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Guideline for Management at the Extremes of Prematurity
Thames Valley & Wessex Operational Delivery Networks (Hosted by University Hospital Southampton NHS Foundation Trust) THAMES VALLEY & WESSEX NEONATAL OPERATIONAL DELIVERY NETWORK Guideline for Management at the Extremes of Prematurity Approved by/on: Thames Valley & Wessex Neonatal ODN Governance Group December 2020. Date of publication September 2020 Last Reviewed January 2021 Review date (Max 3 years) January 2024 Natalie Crawford, Patient Safety Felloe, O&G Trainee Lambri Yianni, Neonatal Transformation Fellow, TV&W Neonatal GRID Authors Trainee Tara Selman, UHS Consultant Obstetrician Victoria Puddy Wessex Neonatal ODN Clinical Lead Distribution Thames Valley and Wessex Neonatal Clinical Forum Thames Valley and Wessex Neonatal Network website Thames Valley and Wessex Neonatal Network e-bulletin Related documents References BAPM 2019. Perinatal Management of Extreme Preterm Birth before 27 weeks of gestation. A Framework for Practice. https://hubble-live- assets.s3.amazonaws.com/bapm/attachment/file/182/Extreme_Preterm_28- 11-19_FINAL.pdf Royal College of Obstetricians & Gynaecologists, 2014. Perinatal management of pregnant women at the threshold of infant viability (the obstetric perspective) scientific impact paper no. 41. UK: RCOG. Crowther et al Repeated doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev 2015 7: CD003935 McKinlay et al Repeat antenatal glucocorticoids for women at risk of preterm birth: a Cochrane Systematic Review. Am J OG 2012 206 (3): 187- 194 https://www.togetherforshortlives.org.uk/wp- content/uploads/2018/01/ProRes-Core-Care-Pathway.pdf Macfarlane PI, Wood S, Bennett J. Non-viable delivery at 20-23 weeks gestation: observations and signs of life after birth. -

Sonet Is a Dedicated Neonatal Transfer Service Designed to Move Babies from One Hospital to Neonatal Another for Specialised Or Ongoing Care Across
THAMES VALLEY AND WESSEX NEONATAL NETWORK Southampton Oxford Phone: 01865 223344 SONeT is a dedicated neonatal transfer service designed to move babies from one hospital to Neonatal another for specialised or ongoing care across Thames Valley and Wessex Neonatal Network Hospitals in our Network SONeT operates from two hubs Transport 1) Milton Keynes University Hospital, Milton Keynes : 01908 995591 a) Oxford Hub- covering north patch 2) Oxford University Hospital, Oxford b) Southampton Hub- covering south patch : 01865 223201 3) Stoke Mandeville Hospital, Aylesbury SONeT Oxford Hub : 01296 316115 Level 2, Neonatal Unit 4) Wexham Park Hospital, Slough Women Centre : 01753 634533 Oxford University Hospital, Oxford 5) Royal Berkshire Hospital, Reading OX3 9DU : 0118 3227430 Email: [email protected] 6) Basingstoke and North Hampshire Hospital 01256 313686 7) Queen Alexandra Hospital, Portsmouth SONeT Southampton Hub 02392 283231 Transport office, 8) Princess Anne Hospital, Southampton Neonatal Intensive care Unit 02381 208164 Parent and Carers Mail Point 607 9) Dorset County Hospital, Dorchester Princess Anne Hospital 01305251150 Information University Hospital Southampton 10) Poole Hospital NHS Trust, Poole SO16 5YA 01202 442330 Leaflet Email: [email protected] 11) St Richard’s Hospital, Chichester 01243788122 12) St Mary’s Hospital, Newport, Isle of Wight This leaflet is to help you understand why your If you have any comments about the SONeT 01983524081 baby is being transferred to another hospital. It service, please talk to a member of staff or use the 13) Salisbury NHS Foundation Trust, Salisbury is also intended to give you information about feedback form that the team gives you or you can 01722425180 the Southampton Oxford Newborn Emergency email us on the above emails. -

RHM University Hospital Southampton NHS Foundation Trust
University Hospital Southampton NHS Foundation Trust Inspection report Trust Management Offices, Mailpoint 18 Southampton General Hospital, Tremona Road Southampton Hampshire SO16 6YD Date of inspection visit: 4 - 6 Dec 2018, 22 - 24 Jan Tel: 02380777222 2019 www.uhs.nhs.uk Date of publication: 17/04/2019 We plan our next inspections based on everything we know about services, including whether they appear to be getting better or worse. Each report explains the reason for the inspection. This report describes our judgement of the quality of care provided by this trust. We based it on a combination of what we found when we inspected and other information available to us. It included information given to us from people who use the service, the public and other organisations. This report is a summary of our inspection findings. You can find more detailed information about the service and what we found during our inspection in the related Evidence appendix. Ratings Overall rating for this trust Good ––– Are services safe? Requires improvement ––– Are services effective? Outstanding Are services caring? Good ––– Are services responsive? Requires improvement ––– Are services well-led? Good ––– Are resources used productively? Good ––– 1 University Hospital Southampton NHS Foundation Trust Inspection report 17/04/2019 Summary of findings Combined quality and resource rating Good ––– We rated well-led (leadership) from our inspection of trust management, taking into account what we found about leadership in individual services. We rated other key questions by combining the service ratings and using our professional judgement. Background to the trust University Hospital Southampton NHS Foundation Trust has had foundation trust status since 1 October 2011. -
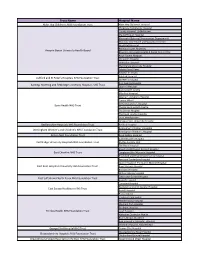
Trust Name Hospital Name
Trust Name Hospital Name Alder Hey Children's NHS Foundation Trust Alder Hey Children's Hospital Chepstow Community Hospital County Hospital, Griffithstown Maindiff Court Hospital Mamhalid (External Procurement Department) Monnow Vale Health and Social Care Centre Nevill Hall Hospital Redwood Suite, Rhymney Aneurin Bevan University Health Board Rhymney Integrated Health & Social Care Centre Royal Gwent Hospital St Cadoc's Hospital St Woolos Hospital The Grange University Hospital Ysbyty Ystrad Fawr Ysbyty'r tri Chwm Ashford Hospital Ashford and St Peter's Hospitals NHS Foundation Trust St Peter's Hospital King George Hospital Barking, Havering and Redbridge University Hospitals NHS Trust Queen's Hospital Barking Birth Centre Mile End Hospital Newham University Hospital Canary Wharf St Bartholomew's Hospital Barts Health NHS Trust The Barkantine Birth Centre The Dental Hospital The Royal London Hospital Trust Headquarters Whipps Cross University Hospital Bedfordshire Hospitals NHS Foundation Trust Bedford Hospital Birmingham Children's Hospital Birmingham Women's and Children's NHS Foundation Trust Birmingham Women's Hospital Bolton NHS Foundation Trust Royal Bolton Hospital Addenbrooke's Hospital Cambridge University Hospitals NHS Foundation Trust Ely Day Surgery Unit The Rosie Hospital Macclesfield District General Hospital East Cheshire NHS Trust Congleton War Memorial Hospital Knutsford and District Community Hospital Kent and Canterbury Hospital Queen Elizabeth The Queen Mother Hospital East Kent Hospitals University NHS Foundation -

Candidate Brief for the Position of Chief Strategy Officer University Hospital Southampton NHS Foundation Trust
Chief Strategy Officer | University Hospital Southampton NHS Foundation Trust Candidate brief for the position of Chief Strategy Officer University Hospital Southampton NHS Foundation Trust August 2021 odgersberndtson.com 1 Chief Strategy Officer | University Hospital Southampton NHS Foundation Trust Contents About University Hospital Southampton NHS Foundation Trust 3 Job Description 11 Person Specification 14 How to Apply 16 odgersberndtson.comodgersberndtson.com 2 Chief Strategy Officer | University Hospital Southampton NHS Foundation Trust About University Hospital Southampton NHS Foundation Trust University Hospital Southampton NHS Foundation Trust (UHS) provides services to some 1.9 million people living in Southampton and south Hampshire as well as specialist services including neurosciences, cardiac and specialist children’s services to more than 3.7 million people in central southern England and the Channel Islands. With a turnover last year of more than £1bn, the Trust is one of the largest in the country. Every year over 12,000 staff: ° treat c. 170,000 inpatients and day patients, including about 750,000 emergency admissions; ° see approximately 700,000 people at outpatient appointments; and ° deal with around 140,000 cases in our emergency department. Providing these services costs about £2.75million a day. UHS is a centre of excellence for training the doctors and nurses of the future and developing treatments for tomorrow’s patients. Its role in research and education, developed in active partnership with the University of Southampton, distinguishes it as a hospital that works at the leading edge of healthcare developments in the NHS and internationally. We are a nationally leading hospital for research into cancer, respiratory disease, nutrition, cardio-vascular disease, bone and joint conditions and complex immune system problems. -

20 September 2019
20 SEPTEMBER 2019 ADVANCES IN IMAGING ORGANISED BY THE BIR WESSEX BRANCH Venue: Heartbeat Lecture Theatre, University of Southampton CPD: 4 CREDIT Platinum sponsors Silver sponsor Bronze sponsors Bayer have part funded this event ADVANCES IN IMAGING ORGANISED BY THE BIR WESSEX BRANCH Venue: Heartbeat Lecture Theatre, University of Southampton CPD: 4 CREDITS This event will begin with a lunch followed by an afternoon of lectures. This years’ meeting will focus on advances in imaging: Artificial intelligence, machine learning and beyond. The day is aimed at presenting advances in current medical imaging and how these advances are currently being utilised and how they may effect imaging practice in the future. Topics discussed will include artificial intelligence and machine learning along with cutting-edge new imaging techniques in other fields of imaging. Who should attend: Radiology consultants and trainees, medical physicists, radiographers and non-radiology medical specialists with an interest in imaging (cardiologists, oncologists etc) Educational aims: • To inform the audience of new advances in medical imaging • To explain how these advances are being applied in current clinical practice • To predict how these advances may be applied in the future and what implications that has for current imaging practitioners 12:00 Lunch and registration 14:35 Artificial intelligence in radiology: how will we be 13:00 Welcome and introduction affected? Dr Simon Wong, ST2 Radiology 13:05 Machine Learning and AI – Registrar, University Hospital what -

Trust Name Site Principal Investigator RM / Coordinator Airedale NHS
PAN-COVID project partners (planning funding application, study conduct) Dr Mandish Dhanjal Imperial College Healthcare NHS Trust Professor Tg Teoh Imperial College Healthcare NHS Trust, Imperial College London Dr Alison Wright Royal Free NHS Foundation Trust, London Professor Liona Poon Chinese University of Hong Kong Alison Perry Manager, Women's Health Research Centre, Imperial College London Dr Caroline Shaw Clincial Lecturer, Imperial College London Professor Dirk Timmerman KU Leuven, Belgium Professor Neil Ferguson Imperial College London Professor Neena Modi Imperial College London PAN-COVID Investigators Trust Name Site Principal Investigator RM / Coordinator Airedale NHS Foundation Trust Soum Nallapeta emma dooks Aneurin Bevan University Health Board Royal Gwent Hospital Emma Mills Tracy James Ashford and St Peter's Hospitals NHS Foundation Trust St Peter’s Hospital Beth Peers Hayley Tarft Barnsley Hospital NHS Foundation Trust Sarah Stables Allison Daniels Barts Health NHS Trust Royal London Hospital Dr Stamatina Iliodromiti Megan Parrott Barts Health NHS Trust Newham Hospital Tabitha Newman Barts Health NHS Trust Whipps Cross Hospital Amy Thomas Betsi Cadwaladr University Health Board Wrexham Maelor Maggie Armstrong SARAH DAVIES Betsi Cadwaladr University Health Board Ysbyty Gwynedd Hilary Owen Betsi Cadwaladr University Health Board Glan Clwyd MEL HOLLINS Birmingham Women's and Children's NHS Foundation Birmingham Women’s Hospital Shanteela Mccooty Amy Woodhead Black Country Healthcare NHS Foundation trust Dorothy Pattison -

Association of Early Postnatal Transfer and Birth Outside a BMJ: First Published As 10.1136/Bmj.L5678 on 16 October 2019
RESEARCH Association of early postnatal transfer and birth outside a BMJ: first published as 10.1136/bmj.l5678 on 16 October 2019. Downloaded from tertiary hospital with mortality and severe brain injury in extremely preterm infants: observational cohort study with propensity score matching Kjell Helenius,1,2,3 Nicholas Longford,3 Liisa Lehtonen,1,2 Neena Modi,3 Chris Gale,3 on behalf of the Neonatal Data Analysis Unit and the United Kingdom Neonatal Collaborative 1Department of Paediatrics and ABSTRACT odds of death before discharge (odds ratio 1.22, 95% Adolescent Medicine, Turku OBJECTIVE confidence interval 0.92 to 1.61) but significantly University Hospital, Turku, Finland To determine if postnatal transfer or birth in a non- higher odds of severe brain injury (2.32, 1.78 to 3.06; 2Department of Clinical tertiary hospital is associated with adverse outcomes. number needed to treat (NNT) 8) and significantly Medicine, University of Turku, DESIGN lower odds of survival without severe brain injury Turku, Finland (0.60, 0.47 to 0.76; NNT 9). Compared with controls, 3 Observational cohort study with propensity score Section of Neonatal Medicine, matching. infants in the non-tertiary care group had significantly Department of Medicine, higher odds of death (1.34, 1.02 to 1.77; NNT 20) but Chelsea and Westminster SETTING no significant difference in the odds of severe brain campus, Imperial College National health service neonatal care in England; London, London SW10 9NH, UK injury (0.95, 0.70 to 1.30) or survival without severe population data held in the National Neonatal Correspondence to: C Gale brain injury (0.82, 0.64 to 1.05). -

TV Wessex Surgical Care Pathway
Thames Valley & Wessex Operational Delivery Networks (Hosted by University Hospital Southampton NHS Foundation Trust) THAMES VALLEY & WESSEX NEONATAL OPERATIONAL DELIVERY NETWORK THAMES VALLEY & WESSEX ODN NEONATAL SURGICAL PATHWAY Approved by/ on: Thames Valley & Wessex Neonatal ODN Governance Group 19th October 2017 Date of publication September 2017 Last Reviewed New Guideline Review date (Max 3 years) September 2020 Dr Eleri Adams TV Clinical Lead Authors Dr Victoria Puddy Wessex Clinical Lead Distribution Thames Valley and Wessex Neonatal Clinical Forums Thames Valley and Wessex Neonatal Network website Related documents British Association of Perinatal Medicine (BAPM) Service Standards (August 2010) Report of Department of Health Expert Working Group on Neonatal Intensive Care Services (2003) Department of Health: Toolkit for High Quality Neonatal Services (2009) NHS England Neonatal Critical Care (Intensive Care, HDU and Special Care) Service Specification E08/S/a NHS England Neonatal Intensive Care, Transport. Service Specification E08/S/b NHS England Paediatric Surgery: Neonates - Service Specification E02/S/c Implications of race, This guideline must be implemented fairly and without prejudice equality & other diversity whether on the grounds of race, gender, sexual orientation or religion. duties for this document Page 1 of 5 Neonatal Surgery Care Pathway – Final TV & W Surgical Pathway September 2017 ratified Neonatal Generic email: [email protected] Neonatal Website: http://southodns.nhs.ukneonatal-network 1.0 Aim of Pathway The aim of TV & Wessex Neonatal surgical pathway is to describe the care pathway for neonates who have been identified as having a surgical abnormality within Thames Valley and Wessex Neonatal Network. 2.0 Scope of Pathways This pathway applies to all neonatal and maternity units covered by Thames Valley Neonatal Network. -

UKOSS Newsletter 53
UK Obstetric Surveillance System 53 NEWSLETTER 53 - April 2018 53 Applications sought for new members of the UKOSS Steering Committee: Anaesthetist and Epidemiologist/ Trainee with an interest in Epidemiology The UK Obstetric Surveillance System (UKOSS), a joint initiative between the National Perinatal Epidemiology Unit and the Royal College of Obstetricians and Gynaecologists, currently has vacancies for an Anaesthetist and Epidemiologist on its Steering Committee. We especially welcome applications from Scottish representatives as we would like to increase Scottish representation on the committee and will also consider applications from experienced trainees with an interest in epidemiology. UKOSS was launched in February 2005 and is designed to be used to study a range of uncommon conditions in pregnancy. It is also supported by the Royal College of Midwives, the Obstetric Anaesthetists Association, the NCT, the Faculty of Public Health and Public Health England. Currently, all 198 consultant-led maternity units in the UK contribute to UKOSS and the system has been extremely successful over the past few years in collecting information on women with rare disorders of pregnancy (conditions with an estimated incidence of less than one in 2000 births), allowing us to document the incidence, management and outcomes of these conditions, and thus to contribute to improvement of maternity care in the future. More information on UKOSS can be found at https://www.npeu.ox.ac.uk/ukoss. The UKOSS Steering Committee is multi-disciplinary and meets three times a year. Its main roles are to consider applications for inclusion of new studies on the UKOSS programme and to monitor the progress of ongoing studies. -

Swansea Department of Liaison Psychiatry
Updated April 2020 Organisation Team Name and Hospitals Covered Status Swansea Department of Liaison Psychiatry Swansea Bay University Morriston Hospital, Swansea; Singleton Hospital, Accredited Health Board Swansea; Neath Port Talbot Hospital; Baglan and Gorseinon Hospital, Swansea Great Western Hospital Mental Health Liaison Avon & Wiltshire Mental Health Service Accredited Partnership NHS Trust Great Western Hospital, Swindon Barnet, Enfield and Haringey North Middlesex Mental Health Liaison Service Members Mental Health NHS Trust North Middlesex University Hospital Barnet, Enfield and Haringey Barnet Hospital Mental Health Liaison Service Accredited Mental Health NHS Trust Barnet Hospital Royal Berkshire Hospital Psychological Medicine Berkshire Healthcare NHS Service Members Foundation Trust Royal Berkshire Hospital Berkshire Healthcare NHS East Berkshire Psychological Medicine Accredited Foundation Trust Wexham Park Hospital Birmingham and Solihull Birmingham City Hospital Liaison Psychiatry Mental Health NHS Foundation Team Accredited Trust Birmingham City Hospital Birmingham and Solihull Good Hope Hospital Liaison Psychiatry Team Mental Health NHS Foundation Accredited Good Hope Hospital Trust Birmingham and Solihull Solihull Hospital Liaison Psychiatry Team Mental Health NHS Foundation Not Accredited Solihull Hospital Trust Updated April 2020 Birmingham and Solihull Heartlands Liaison Psychiatry Team Mental Health NHS Foundation Not Accredited Heartlands Hospital Trust Birmingham and Solihull Queen Elizabeth Hospital, Birmingham, -

Freedom of Information Act 2000|RESPONSE to REQUEST
Freedom of Information Act 2000|RESPONSE TO REQUEST INFORMATION PROVIDED BY THE UNIVERSITY OF SOUTHAMPTON Arem Seven https://www.whatdotheyknow.com/body/university_of_southamptonBy email: [email protected] 4 June 2021 Dear Arem Seven, G00296: Freedom of Information Request We refer to your request for information dated 06/05/2021 under the Freedom of Information Act 2000 (the “Act”). Question Dear University of Southampton, Could you please provide me with a list of all the hospitals in which medical students from the University of Southampton School of Medicine undertake clinical placements in. Please provide a list of the individual hospitals and not the NHS trusts e.g. "Southampton General Hospital" rather than "University Hospital Southampton NHS Foundation Trust". Yours faithfully, Arem Seven ------------------------------------------------------------------- Please use this email address for all replies to this request: [email protected] your organisation's FOI page. Answer Please find below your question, with the University’s corresponding response. Antelope House/ College Keep Basingstoke and North Hampshire Hospital Colebrook Centre Dorset County Hospital Legal Services, 37, Highfield Campus, University of Southampton, Southampton SO17 1BJ United Kingdom Tel: +44 (0)23 8059 4684 Fax: +44 (0)23 8059 5781 www.southampton.ac.uk Farnham Road Hospital Fountain Way Hospital Frimley Park Hospital Gosport War Memorial Hospital Jersey General Hospital FreedomLymington of Information New