The Role of the Health Professional in Supporting Self Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Patient Care Through Telepharmacy September 2016
Patient Care through Telepharmacy September 2016 Gregory Janes Objectives 1. Describe why telepharmacy started and how it has evolved with technology 2. Explain how telepharmacy is being used to provide better patient care, especially in rural areas 3. Understand the current regulatory environment around the US and what states are doing with regulation Agenda ● Origins of Telepharmacy ● Why now? ● Telepharmacy process ● Regulatory environment ● Future Applications Telepharmacy Prescription verification CounselingPrescription & verification Education History Origins of Telepharmacy 1942 Australia’s Royal Flying Doctor Service 2001 U.S. has first state pass telepharmacy regulation 2003 Canada begins first telepharmacy service 2010 Hong Kong sees first videoconferencing consulting services US Telepharmacy Timeline 2001 North Dakota first state to allow 2001 Community Health Association in Spokane, WA launches program 2002 NDSU study begins 2003 Alaska Native Medical Center program 2006 U.S. Navy begins telepharmacy 2012 New generation begins in Iowa Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii NDSU Telepharmacy Study Study from 2002-2008 ● 81 pharmacies ○ 53 retail and 28 hospital ● Rate of dispensing errors <1% ○ Compared to national average of ~2% ● Positive outcomes, mechanisms could be improved Source: The North Dakota Experience: Achieving High-Performance -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

Botswana Health Professions Council (BHPC) Before Seeing Patients
BHPC Application Instructions for BUP Travelers Just as no person would be allowed to walk onto the wards of HUP or any other US hospital and begin treating patients without presenting their credentials, no one may practice in any hospital or clinic in Botswana without official permission. Any physician practicing medicine in Botswana is required to register with the Botswana Health Professions Council (BHPC) before seeing patients. To register you must bring the following documents with you to Botswana: 4 x passport photos 1 x notarized copy of passport photo page 2 x letters of recommendation from doctors/supervisors you work with (letters to be original, no digital copies allowed by BHPC, dated no older than six months) 1 x notarized copy of your medical degree/diploma 1 x notarized copy of your state medical license/registration 1 x CV Copy of offer letter (provided in Botswana) Cover letter of application form (provided in Botswana) Application fee (P30 ≈ $3) BUP staff will assist you in completing the application (pp 3-6 of this document) in country and take you to the BHPC on your first day during orientation to submit the forms and then again on the Wednesday following arrival to receive your approval. Note that you cannot practice medicine until the BHPC registration is completed. You should plan to arrive in Botswana on the weekend prior to when you plan to work so that your BHPC application can be turned in on Monday and you can receive registration certification on Wednesday afternoon. You will then be able to start to practice medicine on Thursday. -

Pre-Med & Other Health Programs
PRE-MED & OTHER HEALTH PROGRAMS Berkeley offers excellent undergraduate preparation for medical and other health-related professional schools and sends an impressive number of students on to these graduate programs each year. Cal, like most universities, does not offer a specific “pre-med” major. Few colleges in the United States do, because there is no specific major required for admission to medical or other health- related schools. All students obtain a bachelor’s degree before admission to medical school. For students seeking admission to dentistry, veterinary medicine, optometry, and other health- related graduate programs, many have received a bachelor’s degree prior to admission. What should I major in at Berkeley, AP credits will not satisfy prerequisites at most Does it make a difference where I if I want to go to medical school? medical schools.) Select an academic major that complete my academic preparation for interests you and allows flexibility in taking the There is no preferred pre-med major. Every year medical or other health-related schools? required pre-med courses. students with majors in the social sciences, The quality and reputation of the college or humanities, chemistry and engineering are What should I do when I’m not in class? university from which you graduate can play a accepted to medical school from Berkeley. role in your acceptance to a medical school. If you want to study biology at Berkeley, you One option is to experience the health care The high quality of Berkeley students and can choose from more than 25 areas of environment in a paid or volunteer position during the campus’ worldwide academic reputation specialization in the biological sciences, such college. -

Oklahoma Primary Care Health Care Workforce Gap Analysis
Oklahoma Primary Care Health Care Workforce Gap Analysis DRAFT Prepared by OSU Center for Rural Health OSU Center for Health Sciences Tulsa, Oklahoma June 2015 Table of Contents Table of Figures ..................................................................................................................................................... ii Tables........................................................................................................................................................................ iii Introduction ............................................................................................................................................................ 1 Background & Data Acquisition ...................................................................................................................... 2 Methodology ........................................................................................................................................................... 2 Primary Care Provider Supply ......................................................................................................................... 3 Primary Care Provider Demand ................................................................................................................... 10 Conclusions .......................................................................................................................................................... 12 Limitations ........................................................................................................................................................... -

Primary Care Network Listing | Healthpartners
DHS-6594C-ENG HealthPartners® Minnesota Senior Health Options (MSHO) (HMO SNP) Network April 2018 – September 2018 PRIMARY CARE NETWORK LISTING Minnesota Counties: Anoka, Benton, Carver, Chisago, Dakota, Hennepin, Ramsey, Scott, Sherburne, Stearns, Washington, Wright HealthPartners 8170 33rd Ave S. P.O. Box 1309 Minneapolis, MN 55440-1309 Member Services: 952-967-7029 or 1-888-820-4285 (TTY/TDD 711) Oct. 1 – Feb. 14 8 a.m. to 8 p.m. CT, seven days a week Feb. 15 – Sept. 30 8 a.m. to 8 p.m. CT, Monday – Friday healthpartners.com/msho HealthPartners is a health plan that contracts with both Medicare and the Minnesota Medical Assistance (Medicaid) program to provide benefits of both programs to enrollees. Enrollment in HealthPartners depends on contract renewal. HealthPartners MSHO Plan 16697_Print April 2018 H2422 108677 DHS Approved 1/25/2018 1-888-820-4285 Attention. If you need free help interpreting this document, call the above number. ያስተውሉ፡ ካለምንም ክፍያ ይህንን ዶኩመንት የሚተረጉምሎ አስተርጓሚ ከፈለጉ ከላይ ወደተጻፈው የስልክ ቁጥር ይደውሉ። مﻻحظة: إذا أردت مساعدة مجانية لترجمة هذه الوثيقة، اتصل على الرقم أعﻻه. သတိ။ ဤစာရြက္စာတမ္းအားအခမဲ့ဘာသာျပန္ေပးျခင္း အကူအညီလုုိအပ္ပါက၊ အထက္ပါဖုုန္းနံပါတ္ကုုိေခၚဆုုိပါ။ kMNt’sMKal’ . ebIG~k¨tUvkarCMnYyk~¬gkarbkE¨bäksarenHeday²tKit«f sUmehATUrs&BÍtamelxxagelI . 請注意,如果您需要免費協助傳譯這份文件,請撥打上面的電話號碼。 Attention. Si vous avez besoin d’une aide gratuite pour interpréter le présent document, veuillez appeler au numéro ci-dessus. Thov ua twb zoo nyeem. Yog hais tias koj xav tau kev pab txhais lus rau tsab ntaub ntawv no pub dawb, ces hu rau tus najnpawb xov tooj saum toj no. -

Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals
Allied Health Professionals Consumer Fact Sheet Board of Registration of Allied Health Professionals The Board of Registration in Allied Health evaluates the qualifications of applicants for licensure and grants licenses to those who qualify. It establishes rules and regulations to ensure the integrity and competence of licensees. The Board is the link between the consumer and the allied health professional and, as such, promotes the public health, welfare and safety. Allied health professionals are occupational therapists and assistants, athletic trainers, and physical therapists and assistants. Occupational Therapists/Occupational Therapist Assistants Occupational therapists are health professionals who use occupational activities with specific goals in helping people of all ages to prevent, lessen or overcome physical, psychological or developmental disabilities. Occupational Therapists and Occupational Therapist Assistants help people with physical, psychological, or developmental problems regain abilities or adjust to handicaps. They work with physicians, physical and speech therapists, nurses, social workers, psychologists, teachers and other specialists. Patients may face handicaps, injuries, illness, psychological or social problems, or barriers due to age, economic, and cultural factors. Occupational Therapists: Consult with treatment teams to develop individualized treatment programs. Select and teach activities based on the needs and capabilities of each patient Evaluate each patient's progress, attitude and behavior. Design special equipment to aid patients with disabilities. Teach patients how to adjust to home, work, and social environments. Test and evaluate patients' physical and mental abilities. Educate others about occupational therapy. The goal of occupational therapy (OT) is for persons to achieve the highest level of independence after an injury or illness. OT addresses the whole person - cognitive, physical and emotional status. -

PRIMARY CARE SECTOR OVERVIEW June 2016
PRIMARY CARE SECTOR OVERVIEW June 2016 Investment banking services are provided by Harris Williams LLC, a registered broker-dealer and member of FINRA and SIPC, and Harris Williams & Co. Ltd, which is and regulated by the Financial Conduct Authority. Harris Williams & Co. is a trade name under which Harris Williams LLC and Harris Williams & Co. Ltd conduct business. TABLE OF CONTENTS I PRIMARY CARE SECTOR OVERVIEW II APPENDIX: SELECT MARKET PARTICIPANTS PRIMARY CARE SECTOR OVERVIEW The delivery and coordination of primary care is taking on renewed and increasing importance as the system’s gatekeeper in the evolving U.S. healthcare landscape. Primary care accounts for nearly $250 billion of annual industry revenue and over 55% of total office-based physician visits1,2 . However, the systematic under-investment of this integral component of the healthcare system has created a number of well publicized challenges, including: • Insufficient supply of new primary care physicians from medical school • Lower compensation vis-à-vis other specialties • Demands of an aging population outstripping system resources • Under-supply of primary care to rural areas . As the initial contact point for patients, the primary care system will increasingly function as the gatekeeper for care coordination and patient referrals for public and private payors and for healthcare systems . Therefore primary care now fills a critical role in the transition from fee-for-service (“FFS”) to value-based care . To meet these challenges new, innovative primary care practice models have emerged to address care coordination, access and quality of care, and cost, including the following four models highlighted in this report: • Medicare Advantage/Managed Medicaid • Employer Sponsored Health Clinics • Retail Clinics • Concierge Clinics . -

Allied Health Professionals
POLICY and PROCEDURE TITLE: Allied Health Professionals Number: 13373 Version: 13373.3 Type: Administrative - Medical Staff Author: Martha Hoover Effective Date: 1/15/2015 Original Date: 8/31/1997 Approval Date: 1/8/2015 Deactivation Date: Facility: Banner Churchill Community Hospital Population (Define): Medical Staff Replaces: Approved by: Medical Executive Committee, Banner Health Board TITLE: Allied Health Professionals I. Purpose/Expected Outcome: A. To allow Allied Health Professionals to function at Banner Churchill Community Hospital (the Hospital) in strict compliance with this Policy and applicable sections of the Medical Staff Bylaws and Rules and Regulations of the Medical Staff, subject to the continuing approval of the Medical Executive Committee and the Governing Board of Banner Health. B. This policy contains the credentialing process for Allied Health Professionals (AHPs) at Banner Churchill Community Hospital as well as the general parameters for the functioning of these individuals within the Hospital. All such AHPs who are permitted to practice at the Hospital fall within two (2) broad categories, Independent Allied Health Professionals and Dependent Allied Health Professionals, each having a slightly different relationship to the hospital. II. Definitions: A. ALLIED HEALTH PROFESSIONALS: The term “Allied Health Professionals” means those Dependent Allied Health Professionals and Independent Allied Health Professionals, also referred to as practitioners, who are permitted to evaluate and/or treat patients at Banner Churchill Community Hospital, but who are not members of the Medical Staff. Allied Health Professionals may also be employees of Banner Churchill Community Hospital. B. MEDICAL STAFF: The term “Medical Staff” means the formal organization of all licensed physicians, dentists and podiatrist who are credentialed and privileged to attend patients at Banner Churchill Community Hospital. -

Patient Self-Management Support Programs: an Evaluation
Final Contract Report ______________________________________________________________________________ Patient Self-Management Support Programs: An Evaluation Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 282-00-0005 Prepared by: RAND Health Santa Monica, CA Marjorie L. Pearson, PhD, MSHS Soeren Mattke, MD, DSc Rebecca Shaw, MA M. Susan Ridgely, JD Shelley H. Wiseman, BA AHRQ Publication No. 08-0011 November 2007 This report was prepared by RAND Health under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 282-00-0005). The views expressed in this report are those of the authors, who are responsible for its content. No statement in this report should be construed as an official endorsement by the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services. This document is in the public domain and may be used and reprinted without permission. AHRQ appreciates citation as to source. The suggested citation format is: Pearson ML, Mattke S, Shaw R, Ridgely MS, Wiseman SH. Patient Self-Management Support Programs: An Evaluation. Final Contract Report (Prepared by RAND Health under Contract No. 282-00-0005). Rockville, MD: Agency for Healthcare Research and Quality; November 2007. AHRQ Publication No. 08-0011. ii Acknowledgments The authors acknowledge and thank the following individuals who participated in interviews for this report. We are grateful -

HEALTH and SELF-CARE: a Look Inside Patient and Physician Perspectives on Self-Care
HEALTH AND SELF-CARE: A Look Inside Patient and Physician Perspectives on Self-care Summer 2019 DrWayneJonas.com HEALTH AND SELF-CARE: A Look Inside Patient and Physician Perspectives on Self-care EXECUTIVE SUMMARY . 3 A LETTER FROM DR . WAYNE JONAS . 5 NATIONAL SURVEY INFOGRAPHIC . 7 WHAT DO THE DATA TELL US ABOUT SELF-CARE? . 9 The Evidence Base for Self-Care .. 9 The Samueli Integrative Health Programs/Harris Poll Survey . 10 DEFINING SELF-CARE . 15 Types of Self-Care . 17 Correcting Patient Misconceptions About Self-Care . 18 HOW CAN INTEGRATIVE HEALTH LEAD TO MORE SELF-CARE? . 19 Self-Care’s Role in Integrative Health . 19 Self-Care and Shared Decision Making . 19 SURVEY METHODOLOGY . 20 REFERENCES . 21 Health and Self-Care: A Look Inside Patient and Physician Perspectives on Self-care 2 EXECUTIVE SUMMARY ix in ten adults in the U .S . have a chronic disease and four in ten adults have two or more, according Sto the latest data from the Centers for Disease Control and Prevention. Conditions such as heart disease, cancer, and diabetes are making more people sick every day and will continue to do so without behavior change and self-care. As rates of chronic disease continue to rise, self-care practices will become increasingly important to the nation’s health. This report – developed by Samueli Integrative Health Programs in concert with The Harris Poll – demonstrates the importance of self-care to patients’ health and well-being, explains how to implement self-care services in the healthcare care setting, and discusses the current trends in both doctors’ and patients’ self-care beliefs and practices. -
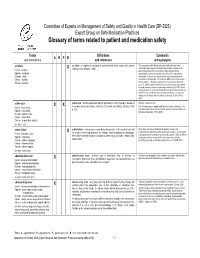
Glossary of Terms Related to Patient and Medication Safety
Committee of Experts on Management of Safety and Quality in Health Care (SP-SQS) Expert Group on Safe Medication Practices Glossary of terms related to patient and medication safety Terms Definitions Comments A R P B and translations and references and synonyms accident accident : an unplanned, unexpected, and undesired event, usually with adverse “For many years safety officials and public health authorities have Xconsequences (Senders, 1994). discouraged use of the word "accident" when it refers to injuries or the French : accident events that produce them. An accident is often understood to be Spanish : accidente unpredictable -a chance occurrence or an "act of God"- and therefore German : Unfall unavoidable. However, most injuries and their precipitating events are Italiano : incidente predictable and preventable. That is why the BMJ has decided to ban the Slovene : nesreča word accident. (…) Purging a common term from our lexicon will not be easy. "Accident" remains entrenched in lay and medical discourse and will no doubt continue to appear in manuscripts submitted to the BMJ. We are asking our editors to be vigilant in detecting and rejecting inappropriate use of the "A" word, and we trust that our readers will keep us on our toes by alerting us to instances when "accidents" slip through.” (Davis & Pless, 2001) active error X X active error : an error associated with the performance of the ‘front-line’ operator of Synonym : sharp-end error French : erreur active a complex system and whose effects are felt almost immediately. (Reason, 1990, This definition has been slightly modified by the Institute of Medicine : “an p.173) error that occurs at the level of the frontline operator and whose effects are Spanish : error activo felt almost immediately.” (Kohn, 2000) German : aktiver Fehler Italiano : errore attivo Slovene : neposredna napaka see also : error active failure active failures : actions or processes during the provision of direct patient care that Since failure is a term not defined in the glossary, its use is not X recommended.